Fig. 10.1
Picture depicts a very narrow mouth opening secondary to previous reconstruction of a dog bite with local advancement flaps. The patient who is currently a teenager had undergone the reconstructive surgery when she was a small child
10.2 Surgical Planning
In order to achieve a successful microvascular reconstruction, the extent of the anticipated tissue defect must be thoroughly addressed during preoperative planning [3]. This includes evaluation of the subunits involved—upper lip, lower lip, commissure, chin, cheek, maxilla, and/or mandible—as well as taking into account the role each of the violated subunits plays in important functions such as speech production, swallowing, eating, drinking, and even puckering. This determination, of the tissue’s functional and esthetic needs, guides the surgeon in the selection of the microvascular free flap that is best suited to allow for return of the patient to a state comparable to his or her preoperative condition. An upper lip reconstruction is not as functionally demanding given the fact that it can be static yet still maintain oral competence if the lower lip is normal [4] (Fig. 10.2a–j). This allows for harvest of a flap without the tendons required for suspension. In male patients, flap choice may be guided by the need to camouflage the reconstruction with hair-bearing skin, allowing for growth of a mustache [7]. If maxillary bone is to be included in the resection, then reconstruction could be achieved with multiple flaps: an osteocutaneous free fibula flap for the maxilla and a fasciocutaneous radial forearm flap for the lip. Other potential options include an osteocutaneous radial forearm flap or a subscapular system flap with both an osteofasciocutaneous and a separate fasciocutaneous paddle both based on the circumflex scapular artery [16]. For lower lip reconstruction, the options include a fasciocutaneous radial forearm flap, fasciocutaneous anterolateral thigh flap or a free gracilis flap. If minimal mandibular bone is involved, then an osteofasciocutaneous radial forearm flap can be used, or as in the maxilla, a multiple flap reconstruction can be undertaken. When other facial subunits are involved, such as the cheek or chin, then a fasciocutaneous anterolateral thigh flap can be used for its added tissue bulk. Other individual patient variables may play into a surgeon’s flap selection, but an appropriate choice should facilitate a successful reconstruction.
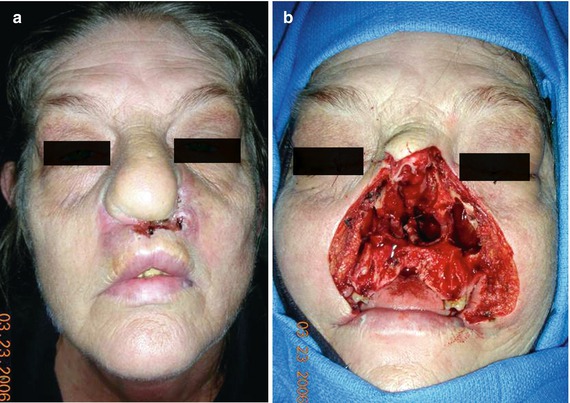

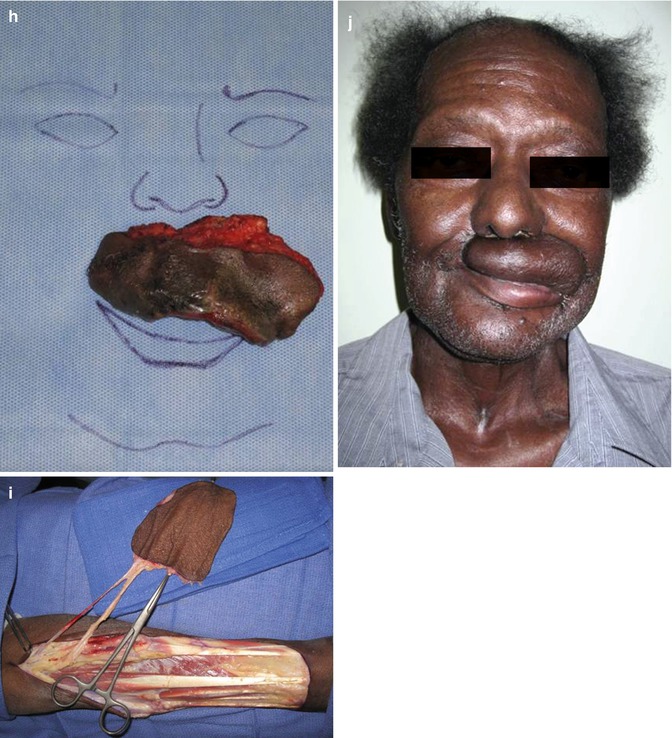
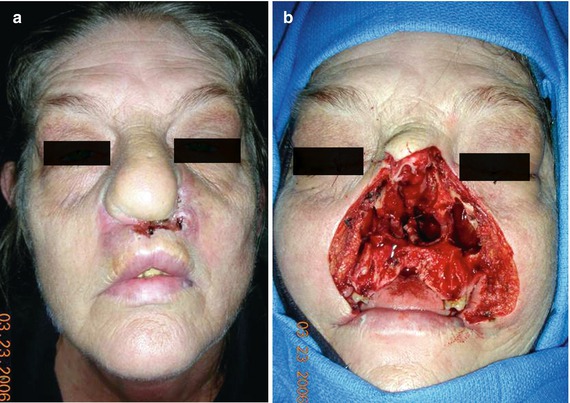

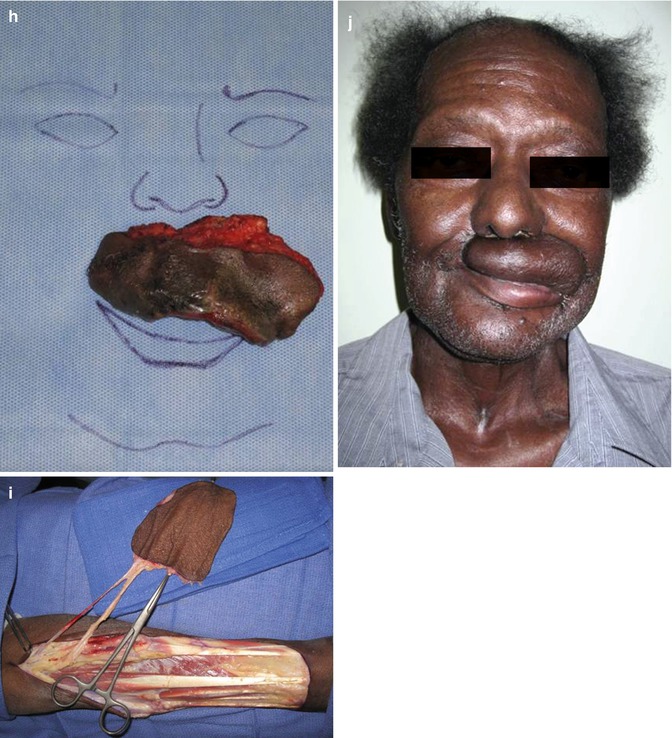
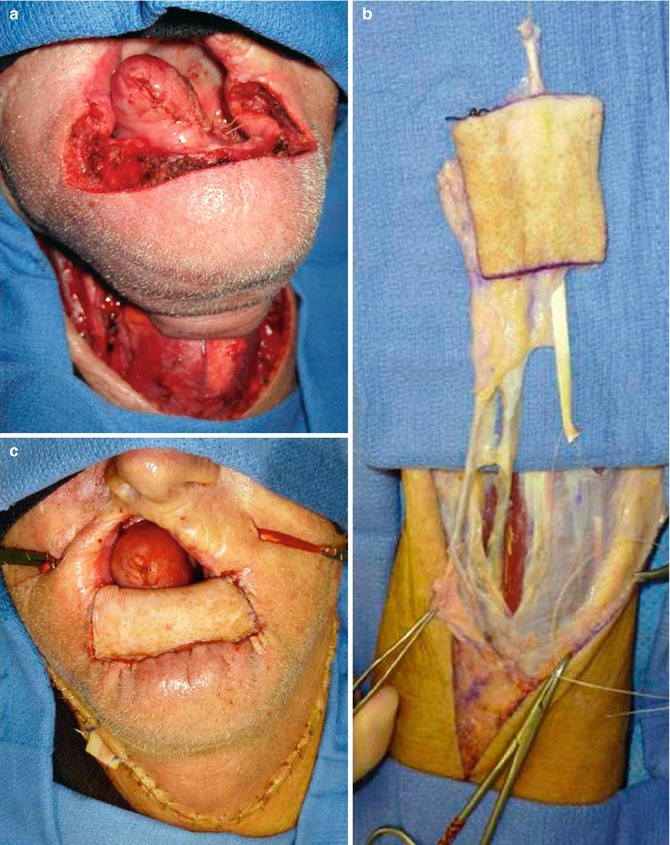
Fig. 10.2
(a) Patient with a large squamous cell carcinoma of the nose with extension to the upper lip and anterior maxilla. (b) Defect secondary to a total rhinectomy, total upper lip resection and anterior maxillectomy. (c) A radial forearm free flap was raised to reconstruct the lip defect and to separate the oral cavity from the nasal cavity. (d) Early post-operative view of the patient after the initial reconstructive surgery. (e) Late view of the patient after radiation therapy. Note the flap is intact and there is a good separation of the oral cavity from the nasal cavity. (f) A middle age African American male presented with a very large squamous cell carcinoma of the left upper lip which extended to the commissure. He underwent bilateral selective neck dissection as seen here. (g) The defect after the radical excision of the primary resulted in a total upper lip defect with extension to the left commissure and slight extension to the lower lip. (h) The specimen shows the extent of resection. (i) A radial forearm free flap with incorporation of the palmaris longus tendon was used to reconstruct the defect. (j) Early post-operative view of the patient showing the reconstructed lip defect with moderate edema still present
10.3 Surgical Template Use
Intraoperatively, once the volume loss has been established, a surgical template can be fabricated to guide flap design (Fig. 10.3). The template helps to ensure that the harvested tissue will have accurate dimensions so that the skin and mucosal deficits can be adequately reconstructed. Of importance to note is that the length of the flap should be smaller than the defect; this will allow for adequate tension to be placed across the flap. The height of the flap, however, should be equal to or slightly greater than the defect. This is especially important on the mucosal side of the reconstruction because of the expected scar contracture, which will decrease the depth of the vestibule [15]. With many oncologic patients undergoing simultaneous neck dissections, template flap design can help to determine the vessel length needed particularly when there is a question of which vessels are present and on which side of the neck the anastomosis will occur. Templates also help determine the best orientation of the vessels to avoid kinking or compression as the flap is folded upon itself. The main benefit, however, of utilizing a surgical template is minimizing the operative time for an already potentially lengthy procedure. A well-designed template allows for both streamlined harvest and circumventing difficulties during inset of the flap. While the oncologic resection procedure is being completed, the harvest team will be able to prepare the flap with appropriate size, inset orientation, neo-vermilion preparation, commissure formation, and vessel preparation for microvascular anastomosis. Template use will also aid in planning the harvest site closure by determining the need for skin grafts. This will allow the operating room personnel to prepare ahead of time for the additional procedure. This, again, helps to minimize operative time, improving patient recovery by limiting the duration of time under a general anesthetic.
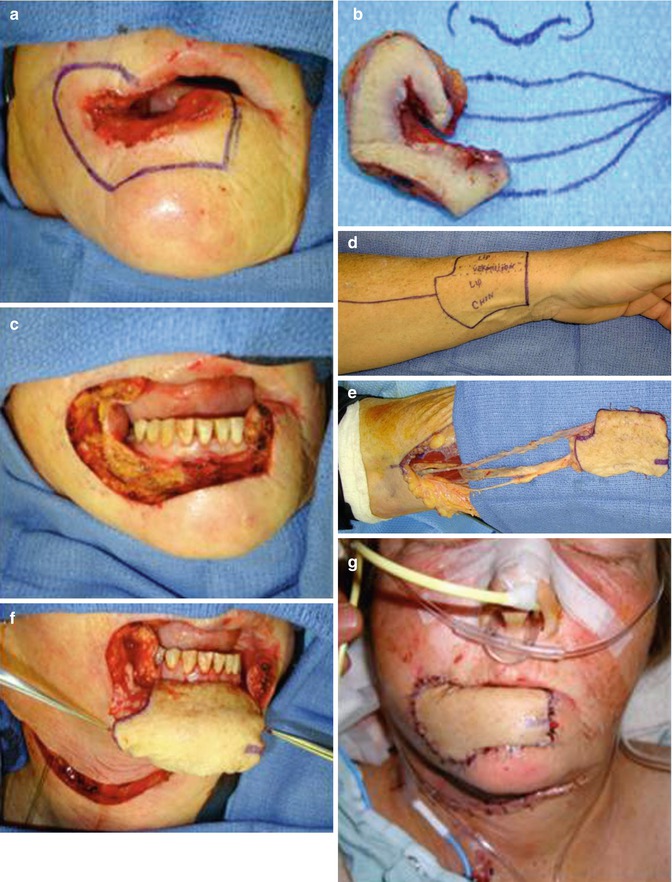

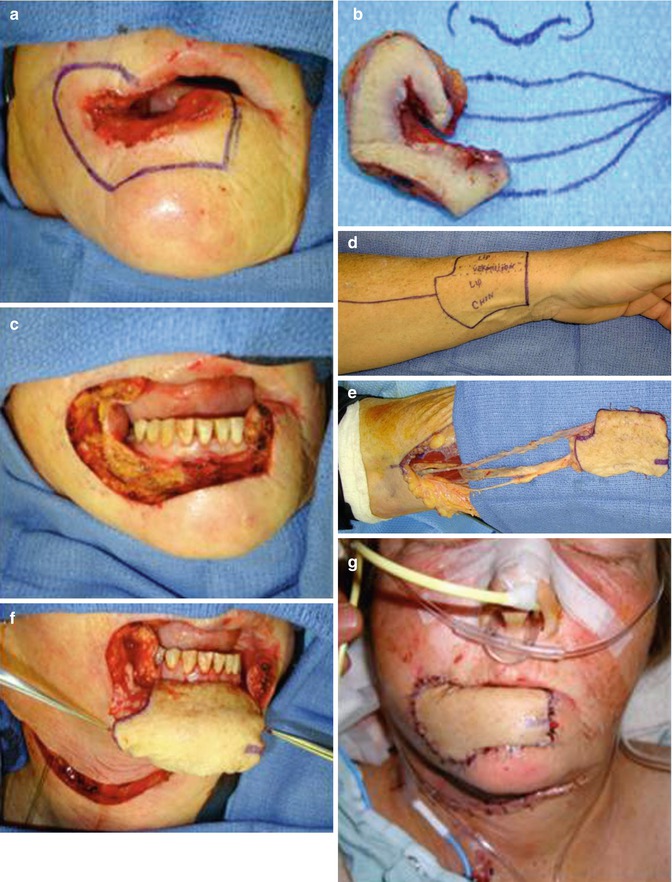

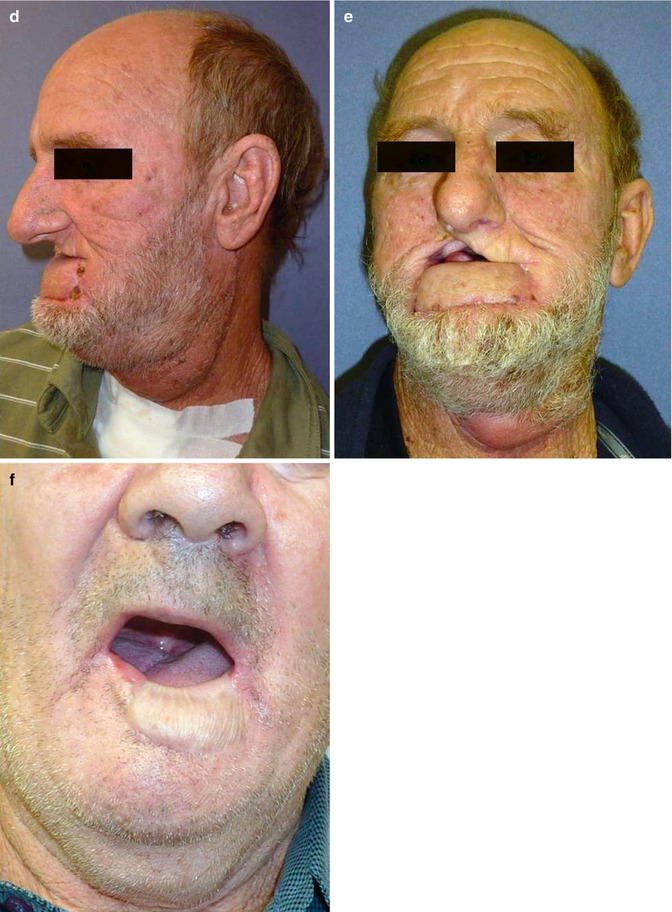
Fig. 10.3
(a) A patient was referred to the clinic with a neglected squamous cell carcinoma of the lower lip which extended to the commissure on the right side and slightly into the upper lip. (b) The resected specimen. (c) The resultant defect after resection of the tumor encompassed nearly the entire lower lip extending to the sulcus and the commissure. (d) Markings for the radial forearm. (e) Elevated flap with inclusion of the palmaris longus tendon to be able to suspend the flap and maintain oral competence. (f) The inset of the flap is shown with care to re-establish the sulcus by first insetting the flap at the depth and then resuspending it with the aid of the tendon. (g) The patient in the early post-operative view with the mouth closed. (h) Patient view with mouth opened
10.4 Flap Description
10.4.1 Radial Forearm Free Flap Advantages
The free radial forearm flap has become the workhorse flap for lip reconstruction since its description by Sakai et al. in [17]. Based on the radial artery and its vena comitans, the radial forearm flap produces a thin, pliable skin paddle and offers numerous additional advantages including (1) relative ease of harvest, (2) distance from the recipient site to allow for a two-team approach, (3) long pedicle length with good vessel caliber, (4) adequate color match, and (5) relatively less hair-bearing ulnar skin [11]. Additionally, the flap can incorporate a static or dynamic suspension and can also be harvested with the lateral antebrachial cutaneous nerve to render the flap sensate.
10.4.2 Static Versus Dynamic Suspension of Radial Forearm Free Flap
With the inclusion of the palmaris longus tendon upon which the flap is centered during harvest, both static and dynamic suspensions can be achieved (Fig. 10.4). This flap design allows for an internal mucosal lining with a watertight closure that will recreate the depth of the vestibule to help maintain oral competence and containment of salivary secretions. An external skin paddle is approximated to the remaining facial soft tissue and is placed under some tension to prevent lip ptosis or inversion. The vascular pedicle should be placed on the side of the flap that will reconstitute the external skin and run parallel to the axis of the palmaris longus tendon to prevent kinking when the palmaris longus tendon sling is tightened across the lip margin. The palmaris longus tendon can then be sutured to the periosteum of the zygoma or the modiolus for a static suspension [5]. A dynamic suspension can be accomplished by suturing the palmaris longus tendon to the remaining orbicularis oris muscle [9] or masseter muscle [18], which would aid in closure of the oral stoma upon contraction of the residual muscles. In 2004 [13], Jeng et al. described harvesting 5 cm of palmaris longus tendon on either side of the flap to allow for the tendon to be passed intramuscularly through the modiolus and anchored to the remaining orbicularis muscle of the upper lip to maximize the oral competence that could be achieved. Another technique described for the dynamic suspension of the radial forearm flap is to turndown bilateral temporalis muscle flaps and suture the palmaris longus tendon to the strip of temporalis muscle under slight tension to simulate the lower lip in repose. These patients are instructed on the immediate postoperative use of the temporalis muscle which shortens with biting, achieving lower lip elevation [6]. Of note, in the event of an anatomical variation in which the palmaris longus tendon is absent, the flap can alternatively be centered over the flexor carpi radialis tendon with similar functional outcomes.