Microinvasive Carcinoma
Microinvasive carcinoma is characterized by the extension of cancer cells beyond the basement membrane of the ductal-lobular system into the adjacent tissue, with no focus more than 0.1 cm in greatest dimension. Lesions that fulfill this definition are staged as T1mi.1 According to the 7th edition of the American Joint Commission on Cancer (AJCC) Cancer Staging Manual, when there are multiple foci of microinvasion, the pathologist should attempt to quantify the number of foci and the range of their sizes, including the largest, but should not report the size of the tumor as the sum of the sizes.1
CLINICAL PRESENTATION
There are no clinical or radiologic features that distinguish microinvasive carcinoma in association with ductal carcinoma in situ (DCIS) from pure DCIS of equivalent size and grade.
GROSS PATHOLOGY
Microinvasive carcinomas cannot, by definition, be identified on gross pathologic examination and are typically detected during microscopic examination of specimens containing DCIS.
HISTOPATHOLOGY
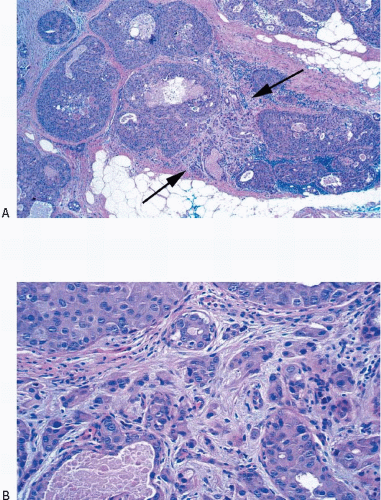
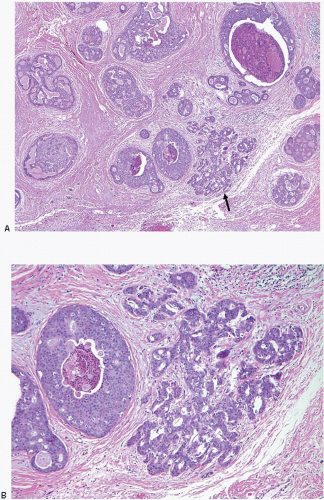
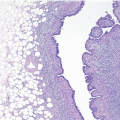
Foci of microinvasive carcinoma are most often seen in association with large areas of high-grade DCIS, but may also be seen with DCIS of any grade or with lobular carcinoma in situ.2, 3 and 4 Rarely, foci of microinvasive carcinoma are identified in the absence of coexistent carcinoma in situ. The presence of periductal stromal desmoplasia and periductal lymphoid infiltrates and the involvement of lobules in association
with high-grade DCIS should heighten the suspicion of microinvasion. However, these features are commonly present in association with high-grade DCIS without demonstrable microinvasion; therefore, their presence alone cannot be depended upon to make this distinction.
with high-grade DCIS should heighten the suspicion of microinvasion. However, these features are commonly present in association with high-grade DCIS without demonstrable microinvasion; therefore, their presence alone cannot be depended upon to make this distinction.
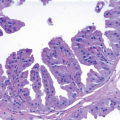
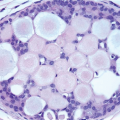
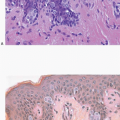
The cells comprising microinvasive foci associated with DCIS typically have the same cytologic features as the cells comprising the DCIS itself and may be present as single cells, small, solid cell clusters, or glands. Although the AJCC criteria define an upper boundary for microinvasive carcinoma (i.e., 0.1 cm), there is no universal agreement on the lower boundary or minimum criteria for identifying microinvasion. Page and Anderson5 require “more than a single collection of cells outside the lobular unit or immediate periductal area.” Fisher6 indicates that the suspicious focus should comprise a “recognized type of invasive cancer.” Elston and Ellis7 state that “only when unequivocal invasion is seen outside the specialized lobular stroma should microinvasive carcinoma be diagnosed.” The definition offered by Silver and Tavassoli8 is less restrictive and recognizes as microinvasive any tumor cells singly and in clusters in the periductal stroma. de Mascarel et al.2 recognize two types of microinvasion, those characterized by the presence of single infiltrating tumor cells and those characterized by infiltrating tumor cell clusters.
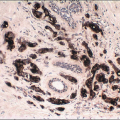
We believe that it is most prudent to consider as microinvasion any tumor cells singly or in small nests within the stroma that are clearly not present within pre-existing ductal-lobular structures or within a benign sclerosing lesion, even if these cells are in the stroma immediately adjacent to ducts and lobules (Figs. 9.1, 9.2, 9.3, 9.4, 9.5, 9.6 and 9.7, e-Figs. 9.1, 9.2, 9.3, 9.4, 9.5 and 9.6). Although the nuclear grade of the neoplastic cells comprising the microinvasive foci can be readily assessed, the extent of these foci is, by definition, limited and this often precludes accurate assessment of a combined histologic grade.
A diagnosis of microinvasion should only be rendered in the presence of unequivocal histologic findings supporting that diagnosis. This is particularly important in core-needle biopsy samples because a diagnosis of microinvasion in a core-needle biopsy is commonly viewed as an indication for sentinel node biopsy or other forms of axillary lymph node examination, whereas a diagnosis of pure DCIS will not result in axillary node examination if the DCIS is of limited extent.
The key features of microinvasive carcinoma are summarized in Table 9.1.
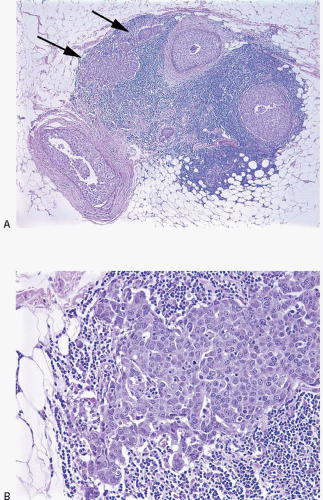 FIGURE 9.3 Microinvasive carcinoma. A:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|