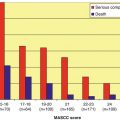
Fig. 5.1
Frequency of single-agent bacteremia in IATC-EORTC trials
Since the turn of the twenty-first century, the reports emerged indicating that GNB have gained importance again but this time with increased resistance to available broad-spectrum agents [24, 25, 29, 31, 34, 38, 41, 44, 47, 50, 67, 88, 98, 104, 105, 152, 154, 158, 198]. The latest published trial of EORTC-IATG including high-risk patients [54] found that 47 % of all bacteremic episodes were due to GNB. Whereas in the two recent EORTC trials [107, 109] in which patients were considered having low-risk neutropenia, the incidence of Gram-negative bacteremias rose to 59 and 50 %, respectively. But one should note that these trials included more patients with solid tumors and the frequencies of patients with acute leukemia were 32 and 51 %, respectively. Reemergence of Gram-negative bacterial infections has also been reported from other cancer centers [92, 152, 154]: Collin et al. [53] observed a decline in ratio of GPB/GNB from 2.7 to 2.3 between 1991 and 1997. Similarly, Mikulska et al. [139] reported from a single center in Italy with patients undergoing HSCTs that the ratio of GPB/GNB decreased from 2.4 in 2004 to 1 in 2007 (p = .043). Unpublished data from the most recent European Conference on Infections in Leukaemia (ECIL) group also indicated that several European cancer centers recently observed a similar increase of GNB in neutropenic cancer patients; however, GPB are still a majority in bloodstream infections (BSIs) [140].
If one compares epidemiology between different countries, in general, US centers reported that GPB are still the predominant microorganisms in cancer patients [210]. Elsewhere, many surveillance studies provided data that the incidence of GNB has become numerically higher than GPB in hematological cancer or hematopoietic stem cell transplant (HSCT) recipients [8, 41, 86, 88]. Interestingly, GNB dominance or equivalence to GPB was usually reported from outside the United States including studies from Brazil [198], Guatemala [23], Japan [50], and several southeastern Asian [25, 48, 49, 98] and Mediterranean countries [44, 86, 88, 104, 105, 158]. But similar reports from some of the Western European countries have also been available [67, 179]. The reasons for this geographical variation are not clear but may be related to the lack of widespread quinolone prophylaxis in at least some of these centers reporting more infections with GNB [86, 105], and in those still using this type of prophylaxis, emerging fluoroquinolone (FQ)-resistant E. coli bacteremias can be accounted for this epidemiology [44, 108]. Another theory which has originally been proposed about the spread of carbapenemase-producing enteric GNB may also be applicable to cancer patients in those countries where environmental sanitation is poor and resistant Gram-negative pathogens can be found in abundance in water and food [7]. Thus, via oral-fecal route, cancer patients may get colonized in the outpatient settings and when they become neutropenic with compromised gastrointestinal mucosa due to chemotherapy, they can acquire bacteremia with these resistant pathogens. It is also noteworthy that in some of these centers, GNB have been the leading pathogens during the last two decades [54, 55, 91, 110]. In our center in Ankara, we observed a similar picture [88, 105]. In a retrospective evaluation of bacteremic episodes in hematological cancer patients with febrile neutropenia, we analyzed 3,703 neutropenic episode in 2,098 patients between 2005 and 2009 [105]. Overall, single Gram-negative bacteremia were detected in 61 % of these episodes. Except 2005 (incidence of GNB, 48 %), GNB were the main type of microorganisms during all study years (range 58–66 %). A previous study dated back to 1997 reported similar figures [88].
Catheter-related bacteremic episodes in neutropenic patients are usually caused by coagulase-negative staphylococci (CNS) [1]. Gram-negatives, albeit much rare, can also be responsible for this picture [47].
5.2.1 Gram-Positive Bacteria and Their Antimicrobial Susceptibility
5.2.1.1 Coagulase-Negative Staphylococci (CNS)
Coagulase negative staphylococci are the most frequent GPB reported as the cause of BSIs in neutropenic cancer patients [1, 9, 113]. The rate of methicillin resistance in these microorganisms is high and varies between 33 and 100 % [38, 44, 88, 139]. In most instances CNS infections are associated with catheter-related BSI involving biofilm production [70]. There are 46 species of CNS described and at least 18 of them are human pathogens [26]. Several of them can cause bacteremia in neutropenic patients and these include S. epidermidis, S. haemolyticus, S. warneri, and S. hominis [26]. Antimicrobial susceptibility to glycopeptides and other anti-Gram-positive agents may differ between these species, thus identification into species level might be important when a CNS is isolated from blood cultures in febrile neutropenic cancer patients especially in case of failing antimicrobial therapy. S. haemolyticus may exhibit decreased glycopeptide susceptibility which is usually more augmented to teicoplanin than vancomycin [30, 73, 155, 168]. Decreased susceptibility is attributable to alterations in the cell wall’s peptidoglycan rather than acquisition of resistance genes via horizontal gene transfer [144]. Resistance to linezolid has also been reported [22].
5.2.1.2 Staphylococcus aureus
This bacterium has been found responsible for up to 7 % of all bacteremic episodes in neutropenic cancer patients [84] with an overall mortality of 23–40 % [177]. Bacteremia is usually associated with skin and soft tissue infections and could also be catheter related. But in most patients, the focus of bacteremia remains undetected [199]. The incidence of methicillin resistance has been reported between 18 and 100 % in patients with hematological malignancies [38, 88, 139, 170, 199, 213]. But, the attributable hospital mortality rate was considerably low (3.5 %) as compared with Gram-negative bacteremias [199].
Staphylococcus aureus was shown to cause late bacteremia (occurring >50 days after transplant) in HSCT recipients, and the incidence was 6/100,000 patient days [137]. Eighty-four percent of bacteremias were community acquired and 85 % of patients had an indwelling central venous catheter (CVC) at presentation. Skin GVHD and length of hospital stay were found to be significant determinants for bacteremic episodes [137]. The incidence rate of methicillin-resistant S. aureus (MRSA) was 23 % compared to 38 % in blood isolates of non-HSCT patients in the same hospital during the same period. The mortality rate (15.4 %) was significantly higher as compared with the control cases. The case fatality rate of MRSA bacteremia was higher than that of methicillin-sensitive S. aureus (MSSA) bacteremia (33 % vs. 10 %).
Community-acquired MRSA isolates are frequently reported as the cause of skin and soft tissue infections in the United States, but relatively rare in Europe [60]. These strains are resistant to beta-lactam antibiotics but maintain susceptibility to many non-beta-lactam antibiotics. In Europe, there has been an increasing problem of transmission of MRSA from colonized livestock (mainly pigs) to those who are in contact with such animals [99]. Although it has not been described as a problem specifically in hematology patient population, it would be wise to advise patients with hematological cancer and immunosuppression to avoid such contacts.
Recently, heteroresistant vancomycin-intermediate S. aureus (hVISA) strains have gained importance. Although their incidence in hematology patients has not been clearly determined, infections with these isolates undermine the efficacy of glycopeptide antibiotics [63, 101, 102]. Those isolates are difficult to detect with routine microbiological work-up, and several reports indicated that patients infected with such strains with a vancomycin MIC >1.5 μg/mL may fail to standard-dose glycopeptide treatment [64, 101].
5.2.1.3 Enterococci
Enterococci can colonize the gastrointestinal tract and may cause BSI in hematology patients. Risk factors for bacteremia in HSCT recipients include mismatched-related or cord-blood transplant, grade 3–4 mucositis, pharyngeal enterococci colonization, and previous cephalosporin use [138]. Vancomycin-resistant E. faecium (VRE) infections are among the most commonly reported causes of bacteremia from many hemato-oncology centers and these bacteria may cause epidemics [106, 112, 138, 169, 170, 211, 212]. Several risk factors described for colonization and for consequent bacteremia include use of broad-spectrum cephalosporins and vancomycin and AML as the underlying disease [12, 116, 145, 186]. Cross-contamination and cross-infection are common in closed units, thus maximum infection control practices including strict isolation of colonized/infected patients are required [178]. Vancomycin-resistant E. faecium colonization rates in HSCT recipients range from 5 to 27 % and the rate of VRE bacteremia in colonized patients is around 30 % [133, 169, 217]. Early VRE bacteremia after HSCT ranged from 3.6 to 22 % with mortality ranging from 0.04 to 85 % [11, 147, 207, 217]. In a recent study, VRE was detected as the leading cause of bacteremia occurring within 30 days of HSCT [103]. Fifty-three and a half percent of patients with bacteremia during this period had VRE. However, only 57 % had VRE colonization before transplantation, indicating that pre-HSCT screening may not identify all patients who are at risk for VRE bacteremia. Attributable mortality was 9 %.
5.2.1.4 Viridans Streptococci
These bacteria are frequently found in the oral flora and can colonize the respiratory and the female genital tracts. The prevalence of their infections varies from 7.8 % in neutropenic cancer patients to 48 % in those receiving high-dose cytosine arabinoside, cyclophosphamide, and idarubicin or undergoing HSCT [32, 55, 65]. Other predisposing factors include use of acid-lowering agents, FQ, or trimethoprim-sulfamethoxazole (TMP-SMX) prophylaxis [71, 167]. Mucositis leading to the breach of integrity of oral mucosa is a significant predisposing factor for streptococcal bacteremia. Other factors causing mucositis such as oral cavity irradiation and lack of H. simplex prophylaxis have also been described as risk factors [211]. Viridans streptococci may be related with septic shock [36]. Penicillin and 3rd-generation cephalosporin resistance may be a problem in some centers and may compromise the treatment [32, 55].
5.2.1.5 Streptococcus pneumoniae
Pneumococcal bacteremia is relatively rare and the incidence of non-bacteremic infections has not been clearly defined in neutropenic patients with cancer. However, in HSCT recipients with GVHD, impaired spleen function due to total body irradiation and decreased production of antipneumococcal antibodies may predispose patients to have invasive pneumococcal disease (IPD) [72, 117]. In a recent retrospective analysis, 135 patients with cancer and pneumococcal bacteremia were investigated [119]: 63 (52 %) had hematological malignancy and 29 (21 %) had HSCT of whom 11 had GVHD. Twenty-two percent of bacteremic episodes were breakthrough in nature. Sixteen (12 %) occurred nosocomially in which nine patients were neutropenic (56 %). Neutropenia was present only in 13 % of patients who acquired bacteremia in the outpatient setting (p < 0.0002). Sixty-seven percent of patients had pneumonia, whereas in 16 % a catheter-related pneumococcal bacteremia was documented. Thirty-six percent of all isolates were non-susceptible to penicillin (MIC >2.0 μg/mL) and 7 % had intermediate susceptibility to ceftriaxone (MIC <2 and >0.5 μg/mL). Attributable mortality was 13.3 %; however, initial inappropriate antimicrobial therapy did not lead to increased mortality.
The overall incidence of IPD was reported as 7 per 1,000 HSCTs, being more prevalent in allogeneic recipients than in patients with auto allografts (9 vs. 5 per 1,000 HSCTs) [214]. Findings reported in a European survey identified more frequent IPD (8.63 per 1,000 HSCT) during >100 days post-transplant period as compared with 2.03/1,000 occurring during the first month post-transplant [72].
Since more than one type of effective vaccines are available against pneumococci and the new conjugated pneumococcal vaccines (CPVs) are more immunogenic than the classical polysaccharide one, CPVs should be used in HSCT recipients [61].
5.2.2 Gram-Negative Bacteria and Their Antimicrobial Susceptibility
5.2.2.1 Enteric Gram-Negatives
Emerging resistance to FQs and broad-spectrum cephalosporins in E. coli has become a significant concern recently, not only in neutropenic cancer patients but also in the community- and hospital-acquired infections worldwide [147, 216]. These trends have significant implications for empirical therapy with ecological and economical consequences: The infections caused by such resistant strains will cause increased use of carbapenems [191], and liberal use of these antibiotics carries the risk of emerging resistance due to carbapenemase production. This phenomenon has been well described worldwide in hospital- and community-acquired infections, but not investigated in hematology patients [7].
In Europe, EARS-NET data in 2010 indicate that E. coli isolated from invasive infections have an unimpeded increase in antimicrobial resistance [68]. The highest resistance was against aminopenicillins (54.2 %, ranged 33.8–83.6 %); increased resistance to third-generation cephalosporins (8.5 %, ranged 2.6–24.8 %) which was related with extended-spectrum beta-lactamase (ESBL) production in 65–100 % of isolates and to FQs (20.7 %, ranged 8.4–42.8 %) was also observed. Usually a north-to-south gradient is evident; more resistance was observed in southern Europe than in the northern countries. However, EARSS data do not specifically provide figures for cancer patients. But, several individual reports reflects the magnitude of the problem in this patient population.
Quinolone resistance in these bacteria is closely related with widespread prophylactic use of FQs in neutropenic patients [29, 43, 108, 110, 173, 190]. Quinolone prophylaxis reduces incidence of GNB in patients including those with acute leukemia and HSCT [37, 38, 59, 87]. Several metanalyses found that mortality is reduced and colonization and infection with FQ-resistant bacteria did not increase in patients receiving such prophylaxis [75–77, 97]. However, these studies usually did not report on baseline colonization in patients and did not take into account the delayed impact of FQs on emerging resistance not only to quinolones but also to the other antibiotics. Moreover, significant heterogeneity in studies that included these metanalyses occurred as well; studies spanned a long period of time including trials as old as 18 years, with different FQs with varying spectrum of activity.
Quinolone resistance has been on rise in the community due to extensive use of FQs for various indications, and patients previously exposed to these antibiotics may get colonized with FQ-resistant E. coli [123]. Thus, local epidemiological data need to be carefully considered before deciding FQ prophylaxis, and if given, the emergence of resistance in bacterial pathogens should be monitored closely. On the other hand, it has been shown that in areas with high prevalence of QR E. coli, FQ prophylaxis may safely be abandoned [83].
Quinolone resistance and extended-spectrum beta-lactamase production by E. coli and to a lesser extent by K. pneumoniae is usually a common occurrence in the same strain. Indeed, data in the literature indicated that use of FQs, previous hospitalization, and previous cancer chemotherapy were significant risk factors for selecting MDR E. coli (i.e., resistant to FQs plus to one other antimicrobial including extended-spectrum cephalosporins or penicillins and aminoglycosides) and causing breakthrough bacteremia [201]. In an analysis of data including 364 patients with 187 documented infections and 164 bacterial isolates in an Italian center, E. coli accounted for 20.1 % of all isolates and 86.8 % of these strains expressed resistance to FQs [44]. Multivariate analysis for identifying risk factors for FQ resistance found that FQ prophylaxis and neutropenia were independent factors.
Resistance profile in K. pneumoniae is similar to that of E. coli, although to a lesser extent. Enterobacter cloacae infections with resistant beta-lactam strains could pose another problem in neutropenic cancer patient population [85, 111, 158]. In our center, 50–65 % of E. coli and 7–25 % of K. pneumoniae blood isolates from neutropenic cancer patients between 2005 and 2009 were resistant to FQs. Resistance rates increased over the years during which FQ prophylaxis was solely used in patients with allogeneic HSCTs but not in others [105].
Availability of local surveillance data and identifying those patients who are likely to get colonized and infected with resistant Enterobacteriaceae have outmost importance for determining the empirical therapy since any delay for giving appropriate therapy would lead to a significant increase in mortality [56, 124, 192].
5.2.2.2 Pseudomonas aeruginosa
Currently the relative frequency of P. aeruginosa in BSI in febrile neutropenic cancer patients is around 10 % (reported range in the literature 0–30 %) [11, 41, 100, 139, 148, 189]. This figure represents a slight increase from prevalence in early 1990s. Pseudomonas aeruginosa is intrinsically resistant to many antimicrobials, but emergence of MDR strains (i.e., a strain resistant to ≥3 of the following antimicrobials: ciprofloxacin, ceftazidime, cefepime, aminoglycosides, piperacillin, or piperacillin-tazobactam) has become of a great concern. Previous exposure to FQs is a significant risk factor for MDR pattern [125]. Other risk factors include previous transplantation (solid organ or HSCT), hospital-acquired BSI, and prior admission to the ICU [100].
In a trial with 12 pediatric hematology centers in Italy, between 2000 and 2008, 127 patients with P. aeruginosa BSIs were analyzed: 31 % of isolates were MDR strains. Total mortality was 19.6 %, whereas mortality in patients infected with MDR P. aeruginosa was 35.8 %. Multivariate analysis indicated that MDR P. aeruginosa infection was the only significant factor associated with infection-related death [42].
The frequency of MDR strains in adult hematology patients was reported up to 71.1 % in a multicenter Italian trial, although the total number of patients was small (n = 38) [189]. Resistance to carbapenems was also high and reported as 60 % (10 % in non-MDR vs. 80 % in MDR strains). Death within the 30 days of the first blood culture was 30.1 % (9.1 % for non-MDR vs. 40.1 % with MDR strains, p = 0.06). A high mortality rate (67 %) was also reported in HSCT recipients. All these figures indicate that P. aeruginosa is responsible for a high mortality in hematological cancer patients, despite its prevalence which remains relatively low as compared with Enterobacteriaceae.
5.2.2.3 Other Non-fermentative Bacteria
Stenotrophomonas maltophilia is an ubiquitous Gram-negative bacterium with limited virulence. However, it may possess significant antimicrobial resistance and cause considerable morbidity and mortality in hematology patients [171]. The organism is unique to produce two different inducible beta-lactamases which can hydrolyze carbapenems, broad-spectrum penicillins, and cephalosporins, thus rendering these antibiotics ineffective for the treatment [6]. Other resistance determinants include a number of multidrug efflux pumps and aminoglycoside-inactivating enzymes [174]. Plasmid-mediated FQ resistance genes have also been described in S. maltophilia genome [175]. All of these mechanisms confer resistance to most available antibiotics for treatment of infections caused by this bacterium. Trimethoprim-sulfamethoxazole is the preferred agent for treating S. maltophilia infections. However, resistance to this agent has been increasingly reported and usually predicts multiresistance in these strains. Recent reports indicate increased incidence of S. maltophilia infections in cancer patients [156, 171]. The bacterium causes CVC-related bacteremia [17, 33] and also colonizes the respiratory tract and may result in consequent infections in patients with tracheostomy and prolonged ventilation [149]. Catheter-related bacteremia was reported to be frequently polymicrobial and prompt removal of catheter is an essential part of the treatment [33]. Gastrointestinal colonization in patients with diarrhea and with previous treatment of carbapenems has also been reported and was proposed to be a source of bacteremia in cancer patients [15, 16]. Other risk factors for S. maltophilia infections include neutropenia, mucosal damage, tracheostomy and mechanical ventilation, and graft-versus-host disease. Previous usage of broad-spectrum antimicrobials including carbapenems and FQs can select resistant S. maltophilia.
Acinetobacter baumannii infections have significantly increased worldwide, especially infecting patients mechanically ventilated in the ICU [66, 78]. MDR pattern is common with most isolates usually susceptible to only colistin in vitro.
In a recent analysis with 128 patients with hematological malignancies admitted to the ICU, 35 (27 %) develop infections with A. baumannii. Pneumonia was the most common site and older age, prior exposure to aminoglycosides, central venous catheterization, and the presence of a nasogastric tube were independent risk factors for infection. Mortality was related with low Glasgow coma score, prior immunosuppressive therapy, neutropenia, mechanical ventilation, and severe sepsis [194].
The frequency of Acinetobacter infections in hematology patients was reported to be 5–7 %, more frequently in non-neutropenic cases [49, 69, 79, 158, 198]. In Hacettepe University, we found that A. baumannii caused 8 % of all bacteremic episodes in hematology patients between 2005 and 2009 [105]. The incidence was lower in patients with acute leukemia and HSCT (6.25 %) as compared with cases with other hematological malignancies (10.4 %).
5.2.3 Anaerobic Bacteria
Although 0.5–17 % of all nosocomial bacteremias are caused by anaerobic bacteria [35, 215], these pathogens are usually underestimated and overlooked in hematological cancer patients.
Clostridium difficile is a major cause of nosocomial infectious diarrhea and can cause severe problems in patients with hematological cancer and HSCT [51, 141, 208]. One-year incidence in HSCT recipients was reported as 9.2 % [13] or 5.6 cases per 10,000 patient days [208]. Among the risk factors were previous chemotherapy, receipt of broad-spectrum antimicrobials, and acute GVHD. Higher rates of treatment failure with metronidazole or vancomycin have been reported in North America as compared with Europe and Asia [197]. Previous FQ use was found as the predominant risk factor for a C. difficile-related epidemic [159]. Moxifloxacin was more frequently associated with C. difficile diarrhea than levofloxacin in neutropenic patients [204].
5.2.4 Unusual Bacteria
Many rare microorganisms have been reported as the cause of infection in hematological cancer patients. Among these are a variety of enteric pathogens such as Achromobacter spp. and Alcaligenes spp. [2], Kluyvera spp., Hafnia spp., and Rahnella spp. [91]. Many bacteria have been reported to cause catheter-related infections and among them are Bacillus spp., diphtheroids, and nontuberculous mycobacteria [27]. Rhodococcus equi can cause cavitary pulmonary disease and brain abscesses [3, 27]. A detailed review for rare microorganisms in cancer patients was published [27].
5.3 Invasive Fungal Infections
The last three decades witnessed a dramatic increase in the incidence and variety of fungal infections that is concurrently followed by the advent of a series of new antifungal agents [121, 162]. In patients with hematological malignancies and HSCT recipients, invasive aspergillosis has become the most prevalent invasive fungal infection (IFI) starting from the 1990s. During this period the incidence of invasive candidiasis (IC) decreased due to mainly widespread use of fluconazole. Recently, several centers throughout the world have reported a significant increase of non-aspergillus molds including Zygomycetes, Fusarium spp., and Scedosporium spp. and non-candida yeasts such as Trichosporon spp. [157, 172].
A multicenter retrospective study between 1999 and 2003 in 18 hematology wards in Italy (SEIFEM-2004) included 11,802 patients with hematological malignancies of whom 35 % had acute leukemia as the underlying disease [151]. Sixty-four percent of IFIs were due to mold infections of which 90 were caused by Aspergillus spp. that is followed by Zygomycetes (4 %) and Fusarium spp. (4 %). Candida albicans accounted for 91 % of yeast infections; other yeasts included Cryptococcus spp. (4 %) and Trichosporon spp. (4 %). The incidence of mold infections was 2.9 % and for yeasts 1.6 %. Attributable mortality rates due to IFI were higher for non-aspergillus molds than aspergillus and yeasts and were as follows: Aspergillus spp. (42 %), Zygomycetes (64 %), Fusarium spp. (53 %), and Candida spp. (33 %).
A retrospective autopsy series in MD Anderson Cancer Center between 1989 and 2003 provided information about invasive fungal infections in patients with hematological malignancies over three different periods of time (1989–1993, 1994–1998, 1999–2003) [45]. Three hundred fourteen IFIs were identified in 1,017 autopsies (31 %) among which invasive mold infections increased significantly (19 %, 24 %, and 25 %, respectively, during the aforementioned three periods, p = 0.05). Zygomycosis emerged as a significant pathogen (1, 4, and 3 %, respectively, p = 0.03), whereas prevalence of invasive aspergillosis (IA) remained stable (16, 19, and 19 %, p = 0.36) and that of invasive candidiasis decreased (13, 10, and 8 %, p = 0.07). More recent epidemiological studies in the United States reported similar observations [115, 157].
5.3.1 Candida spp.
Non-albicans Candida spp. are the predominant agents of IC in hematological cancer patients [80, 90, 187, 203] in contrast to patients with solid tumors or those with non-hematological severe diseases acquiring candidiasis in the ICU in whom C. albicans are still the main infecting fungus [80, 89, 90, 187, 203]. We have observed a similar trend in a survey between 2001 and 2010 with 858 Candida isolates in Hacettepe University in Ankara [14]. There were 381 single isolates from the first episodes of candidemia of which 60 were from patients with hematological malignancies. Non-albicans Candida had a frequency of 67 % and C. tropicalis (33 %) and C. parapsilosis (18 %) were the most frequent isolates.
Two recent, large epidemiological studies from the United States reported very similar results in patients with HSCT [115, 142]: TRANSNET study conducted in 23 US transplant centers between 2001 and 2006 identified 983 IFIs in 875 HSCT recipients [115]. Invasive candidiasis accounted for 30 % of all IFIs with nonalbicans Candida as the causative agent in 81 % of episodes. Candida glabrata (32 %) and C. parapsilosis (16 %) were leading yeasts. PATH registry reported 250 IFIs in 234 patients with HSCT in 16 centers in the United States [142]. Candida was isolated from only 26 % of patients of which 77 % were non-albicans spp. Another PATH registry with invasive candidiasis included <13 % of patients with hematological cancer [93]. Non-albicans Candida spp. were responsible for >92 % of invasive infections in hematology patients including those with HSCT, with C. krusei and C. tropicalis being the most frequent ones. Candidemia with C. krusei was associated with neutropenia, prior antifungal use, hematological malignancy or HSCT, and steroid use. Candida krusei candidemia had the highest 12-week mortality rate (52, 9 %), whereas that of C. parapsilosis had the lowest (23.7 %).
In European surveys, antifungal resistance was low in Candida isolates except in C. krusei which is intrinsically resistant to fluconazole [121]. Previous fluconazole use has been described as a risk factor for selecting C. krusei or other resistant spp. [5, 118]. A recent worldwide surveillance study reported emerging resistance to azoles (fluconazole 7.7 %, posaconazole 5.1 %, and voriconazole 6.4 %) and echinocandins (anidulafungin 3.8 %, caspofungin 5.1 %, and micafungin 3.2 %) in C. glabrata isolates [164]. A similar observation was also reported from Europe [126].
5.3.2 Other Opportunistic Yeast-Like Fungi
There are many opportunistic yeast-like fungi which rarely cause fungemia and disseminated infections in patients with hematological malignancies. Among these the most frequently encountered ones are Trichosporon spp., Rhodotorula spp., and Geotrichum spp. [18, 136, 163].
Trichosporon spp. are the second most common yeast infections in hematological malignancy cases. Patients with acute leukemia are the most vulnerable ones to infection with this pathogen and the most frequent type of infection is catheter-related fungemia [81]. The agent is usually resistant to polyenes and echinocandins, with only reliable in vitro susceptibility to voriconazole.
Rhodotorula spp. cause infections worldwide but most frequently in the Asia-Pacific region with an attributable mortality of 15 % [193]. Catheter-related fungemia is the most frequent presentation in cancer patients [94]. Amphotericin B has good activity against this yeast and successful treatment can be obtained along with removal of the indwelling catheter.
5.3.3 Aspergillus spp.
Aspergillus fumigatus is the leading pathogen for IFI in hematology patients [115, 129–131, 142, 151]. However, other non-fumigatus strains have been emerging and include mainly A. flavus and A. terreus which are well known for their reduced amphotericin B susceptibility [122, 129, 196].
Patients with hematological malignancies and those undergoing HSCT are at the highest risk of developing IA [28, 115, 129, 131]. In the latter group, there is a bimodal distribution of the disease; decreased frequency has been observed during the early neutropenic phase after the first month of post-transplant and higher incidence after the first 100 days of transplantation [115, 129, 130, 195]. Possible explanations of this distribution are shortened duration of neutropenia during the early phase of HSCT and developing chronic GVHD during the late phase and exposure of patients to aspergillus spores in the outpatient settings. Several well-known risk factors have been described for predisposing patients to acquire IA and these include neutropenia, previous broad-spectrum antibiotic therapy, anticancer chemotherapy, respiratory tract colonization with Aspergillus, CMV or Pneumocystis jirovecii infection, and mismatched HSCT [58, 130, 132, 150, 195].
During the 2000s a decrease in attributable mortality, as low as 13 % [153], was observed in patients with IAs as compared with data from the 1990s [151, 195]. Possible explanations of this decline include tools allowing early diagnosis (i.e., use of HRCT, serum levels of galactomannan and beta-D glucan, and PCR-related diagnosis), availability of active antifungals (e.g., liposomal amphotericin B and voriconazole), non-myeloablative induction regimens, and use of peripheral stem cells for transplantation which led to less severe immunosuppression in patients [58, 150, 151].
Recently, Aspergillus fumigatus strains were described acquiring resistance to multiple azole drugs including itraconazole, voriconazole, and posaconazole, both in patients with hematological malignancies and also those with aspergilloma and chronic aspergillosis [62, 184, 196, 200]. Resistance is most commonly associated with point mutations in the Cyp51A gene and mutations can develop during treatment [40, 200]. Although the true incidence of this problem has yet to be determined, there is at least one study reporting very high (up to 55 %) resistance mutations in clinical samples from patients with chronic aspergillosis [62]. Resistance up to 12.8 % has been reported from patients with acute IA in Netherlands and elsewhere, and treatment failure with azoles was described [135, 185], although other reports did not confirm such high incidence [10]. In Dutch cases this resistance has been linked to agricultural consumption of fungicide azole drugs structurally related with triazoles used for the treatment of IA [151, 182, 183].
5.3.4 Zygomycetes
There are two distinct types of infections by these fungi: mucormycosis caused by Mucorales and entomophthoramycosis by Entomophthorales, the latter occurring infrequently and usually restricted to tropical areas causing skin infections [46, 115, 161, 176]. Mucormycosis is the third most common IFI after IA and IC in patients with hematological malignancies [115, 161]. In a recent analysis of 230 cases of mucormycosis from 13 European countries, hematological malignancy was the most common (44 %) underlying disease [181]. The incidence of mucormycosis was reported between 1 and 8 % in patients with acute leukemia and 0.9–2 % in patients with HSCT [161]. Prolonged and severe neutropenia, presence of uncontrolled diabetes mellitus, iron overload, trauma, and use of corticosteroid are among the other risk factors for developing mucormycosis [150, 161]. Prolonged use of voriconazole has been linked to increased incidence of mucormycosis [96, 146, 150, 180]. But this observation has not been confirmed in two recent studies [128, 209]. However, none of these studies involved patients with high-risk factors for developing invasive mold disease. It has also been proposed that patients receiving voriconazole might be more complicated transplant patients and therefore have higher baseline risk for mucormycosis [157].
Mucormycosis is related to very high mortality rate in patients with hematological malignancies, up to 100 %, depending on the type of infection and the underlying disease [115, 131, 151]. In the recent European survey, older age and prior use of caspofungin were found to be significantly associated with mortality [57, 181].
5.3.5 Other Rare Molds
Several hyaline (nonpigmented) molds can cause invasive infection in hematological cancer patients [163]. Among them Fusarium spp. [39] and Scedosporium spp. [157] are the most frequent ones, although their incidence is far less as compared with IA. The risk factors for these mold infections are similar to those of IA, neutropenia in hematological cancer patients and acute and chronic GVHD in HSCT recipients [150]. Mortality is higher than IA and usually between the range of 50 % and more than 90 % [131, 151, 157].
Fusarium spp. demonstrate high MIC values for fluconazole, itraconazole, and posaconazole and caspofungin [19–21, 143, 205]. These values vary between 1 and 4 μg/ml for amphotericin B and 0.25 and 4 μg/ml for voriconazole [19–21]. However, the correlation between in vitro susceptibility and clinical outcome is not straightforward. Both posaconazole and voriconazole have been successfully used for the treatment of fusariosis [160, 165]; as expected the success rates were much higher in those who recovered from neutropenia during the treatment [165].
Scedosporium spp. are ubiquitous pathogens with two species having medical importance: Scedosporium apiospermum (the anamorph of Pseudallescheria boydii) and Scedosporium prolificans. While the former mold is susceptible to itraconazole, voriconazole, and posaconazole [206], the latter is considered to be resistant to all available antifungal agents, voriconazole being the most active one with an MIC of 4 μg/mL [134]. Infections caused by these molds are associated with very high mortality rates in patients with hematologic malignancies [52, 95, 120, 160, 188].
References
1.
Adler A, Yaniv I, Solter E, et al. Catheter-associated bloodstream infections in pediatric hematology-oncology patients: factors associated with catheter removal and recurrence. J Pediatr Hematol Oncol. 2006;28:23–8.PubMed
2.
Aisenberg G, Rolston KV, Safdar A. Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer (1989–2003). Cancer. 2004;101:2134–40.PubMed
3.
Akan H, Akova M, Ataoglu H, et al. Rhodococcus equi and Nocardia brasiliensis infection of the brain and liver in a patient with acute nonlymphoblastic leukemia. Eur J Clin Microbiol Infect Dis. 1998;17:737–9.PubMed
4.
Akova M. Emerging problem pathogens: a review of resistance patterns over time. Int J Infect Dis. 2006;10:S3–8.
5.
Akova M, Akalin HE, Uzun O, Gur D. Emergence of Candida krusei infections after therapy of oropharyngeal candidiasis with fluconazole. Eur J Clin Microbiol Infect Dis. 1991;10:598–9.PubMed
6.
Akova M, Bonfiglio G, Livermore DM. Susceptibility to beta-lactam antibiotics of mutant strains of Xanthomonas maltophilia with high- and low-level constitutive expression of L1 and L2 beta-lactamases. J Med Microbiol. 1991;35:208–13.PubMed
7.
Akova M, Daikos GL, Tzouvelekis L, Carmeli Y. Interventional strategies and current clinical experiences with carbapenemase producing Gram-negative bacteria. Clin Microbiol Infect. 2012;18:439–48.PubMed
8.
Aksu G, Ruhi MZ, Akan H, et al. Aerobic bacterial and fungal infections in peripheral blood stem cell transplants. Bone Marrow Transplant. 2001;27:201–5.PubMed
9.
Al-Tonbary YA, Soliman OE, Sarhan MM, et al. Nosocomial infections and fever of unknown origin in pediatric hematology/oncology unit: a retrospective annual study. World J Pediatr. 2011;7:60–4.PubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree