Squamous cell carcinoma of the anal canal (SCCA) represents an orphan disease. Although prior infection with human papilloma virus is associated with the development of SCCA, knowledge of this relationship has proven ineffective in identifying therapeutic agents that have activity in the management of metastatic SCCA. Combination chemotherapy with traditional cytotoxic agents has demonstrated efficacy in multiple small series. However, immune checkpoint blockade agents have demonstrated efficacy for patients with refractory metastatic SCCA; these agents hold promise in the horizon for patients with metastatic SCCA. Clinical trials should be considered for oncologists to manage patients with metastatic SCCA.
Key points
- •
Squamous cell carcinoma of the anal canal (SCCA) is a rare, understudied disease that can be cured by concurrent chemoradiation in the nonmetastatic setting.
- •
No consensus standard-of-care approach to the treatment of metastatic SCCA exists to date; cytotoxic doublet chemotherapeutic doublets have traditionally been utilized for metastatic disease.
- •
Early results from trials incorporating immune checkpoint blockade agents for the treatment of metastatic SCCA hold great promise for improving survival outcomes for patients with this disease.
Introduction
Anal cancer represents a rare disease that accounts for approximately 2% of all gastrointestinal (GI) malignancies. Although most patients will present with locoregional disease, a fraction of patients will develop distant metastases. This article focuses on the management of metastatic disease of anal cancers of squamous cell histology and not of other underlying histologies like adenocarcinoma or anal melanoma. Previous experiences with systemic chemotherapies and local therapies for oligometastases will be discussed, as will the role of emerging immunotherapy agents as a novel approach to the treatment of distant metastases.
Introduction
Anal cancer represents a rare disease that accounts for approximately 2% of all gastrointestinal (GI) malignancies. Although most patients will present with locoregional disease, a fraction of patients will develop distant metastases. This article focuses on the management of metastatic disease of anal cancers of squamous cell histology and not of other underlying histologies like adenocarcinoma or anal melanoma. Previous experiences with systemic chemotherapies and local therapies for oligometastases will be discussed, as will the role of emerging immunotherapy agents as a novel approach to the treatment of distant metastases.
Epidemiology
Over 90% of anal cancers are of squamous cell histology. In 2016, it is estimated that over 8000 new cases of squamous cell carcinoma of the anal canal (SCCA) will be diagnosed in the United States, with over 1000 deaths from this disease. The annual incidence of SCCA continues to rise, both in the United States and globally, and it is expected that this trend will continue for decades to come. Risk factors for the development of anal cancer include a prior history of gynecologic malignancy, tobacco use, a history of multiple sexual partners, and impaired immunity, whether from use of immunosuppressive agents, underlying autoimmune disease, or from coexisting human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS).
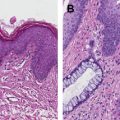
However, by far the most prevalent factor responsible for the development of SCCA is coinfection with human papilloma virus (HPV). This virus also plays an important role in other malignancies such as squamous cell carcinoma of the head and neck, cervical cancer, vaginal/vulvar cancer, and penile cancer. Incorporation of viral DNA into the host cell genome results in expression of the viral oncoproteins E6 and E7, which disrupt p53 and Rb, respectively, to promote oncogenesis. In a series of patients with metastatic SCCA treated at the authors’ institution, the presence of HPV, assessed by the detection of HPV by DNA in situ hybridization and/or p16 by immunohistochemistry, occurred in over 95% of tested tumors. Other groups have also reported that most anal cancers are associated with HPV infection, and it appears as though the presence of HPV serves as a positive prognostic biomarker from these reports, a trend that is similar to outcomes in other HPV-associated malignancies.
HPV-16 is the most common subtype of HPV associated with the development of SCCA. In recent years, preventative quadrivalent and nonavalent vaccines against the most common subtypes of HPV have been introduced to children and adolescents with no prior HPV exposure. Initial reports with this primary prevention approach in adolescent girls have suggested success rates in lowering the incidence of precancerous cervical lesions. Applied to SCCA, 1 prospective study demonstrated that, in a population of men who have-sex with men, use of preventative vaccines against HPV led to lower rates of anal dysplasia. These data have not fully matured to demonstrate lower rates of anal cancer with such vaccines, although updated results are greatly anticipated. The authors suspect that in the decades to come, a generalized trend toward decreased prevalence/incidence of SCCA will occur as the result of these HPV vaccines.
Management of locoregional squamous cell carcinoma of the anal canal
Most patients with newly diagnosed SCCA will present with locoregional disease that has not spread to distant organs. For these patients, the standard of care approach has not changed for decades. Here, patients receive concurrent chemoradiation with either 5–FU/mitomycin C or with 5–FU/cisplatin.
Although concurrent chemoradiation is successful in curing SCCA in the majority of patients, approximately 10% to 30% of this population will develop a locoregional failure with recurrent disease at the site of the primary tumor. Risk factors for recurrence include a primary tumor greater than 5 cm in longest dimension, the presence of regional lymph nodes at diagnosis, and male gender. For such patients who recur after chemoradiation, the standard of care is abdominoperineal resection (APR), which has a success rate with respect to 5-year survival of approximately 40% to 65% following surgery, despite the presence of a tumor that was not eradicated upfront by chemoradiation.
Management of metastatic squamous cell carcinoma of the anal canal with cytotoxic chemotherapy
Because SCCA represents an uncommon GI malignancy for which a small fraction of patients will develop distant metastases, the role of systemic chemotherapy in the management of metastatic disease remains an understudied topic for which extensive experience and robust data are lacking. Indeed, no prospective trial for metastatic SCCA using cytotoxic chemotherapeutic agents has ever been completed. At present, there is no accepted standard of care consensus for the management of distant disease. At large academic referral centers, the treatment approach is based upon published work in the literature from case series and small respective cohorts.
The combination of cisplatin and 5-fluorouracil has been reported as efficacious in multiple small series, and this chemotherapy doublet is the lone recommended therapy for the treatment of metastatic disease by the National Comprehensive Cancer Network (NCCN) panel. One initial report utilizing this combination involved 3 patients at a single institution with metastatic SCCA involving the liver. All patients here demonstrated partial or complete radiographic responses to this regimen, with 2 of the 3 patients experiencing drastic reductions in their tumor volumes, which led to prolonged survival outcomes. This series, however, included patients who had liver involvement as the only site of distant metastases. Nonetheless, it did provide some optimism regarding the use of cisplatin and 5-fluorouracil in the management of metastatic SCCA, consistent with known understanding that these agents have activity in the treatment of advanced/unresectable squamous cell cancers of other primary sites as well. Another single-institution series of 19 patients with metastatic SCCA who had involvement of many different sites of distant metastases examined the use of cisplatin with 5-fluorouracil. Here, 1 complete response was observed, and there were 11 partial responses (response rate 66%). The most common grade 3 to 4 toxicities were noted to be nausea (30%) and nonfebrile neutropenia (13%). At 1 year following initiation of treatment, 62% of patients were still alive, and 32% remained alive at 5 years, for a median survival of 34.5 months. Although the numbers of patients for both of these series are small, they do provide some suggestion that the use of cisplatin with 5-fluorouracil is active and associated with a tolerable toxicity profile for patients with metastatic SCCA.
With a lack of available options for treatment of distant metastases, other groups examined the role of taxanes as a therapeutic approach for the treatment of metastatic SCCA. The combination of carboplatin with paclitaxel is approved for the use of other advanced squamous cell tumors. One single-institution series recently reported outcomes of 18 patients with metastatic SCCA treated with this regimen. Here, 12 patients were administered this doublet as the first-line treatment for their metastatic disease. Radiographic responses were noted in 53% of patients, with 3 complete responses detected. Grade 3 to 4 toxicities were noted in 6 of 18 patients, with the most common toxicity being neutropenia (N = 4). Median overall survival in this cohort was approximately 12 months.
Other series have examined the use of paclitaxel as a single agent following progression on frontline cisplatin/5-fluorouracil. One report detailed the use of paclitaxel at a dose of 175 mg/m 2 every 3 weeks in 5 patients, 2 of whom were noted to be HIV-positive. Disease control (defined as either radiographic response or stable disease) was observed in 3 of these 5 patients. In a separate report of 7 patients with metastatic SCCA who were treated with single-agent paclitaxel at a single institution, partial responses were observed in 4 patients, and stable disease was observed in 1 additional patient. Again, the role of taxanes in the management of metastatic SCCA, whether with or without carboplatin, remains unclear at present. These series should be interpreted with caution given the small number of patients who were included in the analyses.
Integrating both of these approaches, other small cohorts reported results for patients with metastatic SCCA using a triple combination of paclitaxel, carboplatin, and 5-fluorouracil. A prospective phase II trial of these 3 agents for patients with advanced squamous cell cancers of multiple primary sites included 7 patients with metastatic anal cancer. Four patients had radiographic responses, 2 of which were complete radiographic responses. A different series of 8 patients with metastatic SCCA treated with the same 3 cytotoxic chemotherapeutic agents revealed complete responses in 4 patients and progressive disease in the remaining patients. Overall, these 8 patients demonstrated acceptable toxicity from the triple combination of docetaxel, cisplatin, and 5-fluorouracil.
To date, the largest retrospective series for metastatic SCCA percent was reported from cohort of patients treated at M.D. Anderson. Here, 77 patients were examined, with 42 patients (55%) administered 5-fluorouracil/cisplatin, and 24 patients (31%) receiving carboplatin/paclitaxel. Response rates were nominally better with 5-fluorouracil/cisplatin (57%) relative to carboplatin/paclitaxel (33%), although no definitive conclusions can be made from these findings given their noncontrolled and retrospective nature.
As there is no accepted standard of care for the treatment in the front-line setting of metastatic SCCA, a prospective International Rare Cancer Initiative (IRCI)/Eastern Cooperative Oncology Group (ECOG) – American College of Radiology Imaging Network (ACRIN) randomized, phase II trial (EA2133/InterACCT) is ongoing to compare the combinations of cisplatin/5-fluorouracil and carboplatin/paclitaxel for patients with SCCA who have never received any prior systemic chemotherapy for distant metastatic disease. The primary end point for this study is response rate, and the goal is to identify the best chemotherapeutic backbone upon which additional biologic and/or immunotherapeutic agents can be added in future studies, with the goal of improving survival outcomes for patients with metastatic SCCA.
Role of biologic agents in the treatment of metastatic squamous cell carcinoma of the anal canal
To date, the use of targeted therapies in the management of metastatic SCCA has been limited by a lack of understanding regarding the genomic profiling patterns that drive tumor development. Despite mutations in KRAS and NRAS being prevalent in tumors arising from the adjacent colorectum, multiple series analyzing anal tumors have failed to detect RAS mutations in SCCA. In addition, anal tumors have been frequently reported to express epidermal growth factor receptor (EGFR) at high levels on the surface of the cancer cell. Based on these findings, multiple series have examined the role of anti-EGFR monoclonal antibodies like cetuximab, which targets EGFR signaling extracellularly.
One series from M.D. Anderson reported results from 17 patients who received cetuximab, either as a single agent or in combination with systemic chemotherapy, following progression on at least 1 prior line of systemic therapy for metastatic disease. Radiographic responses were noted in 6 of 17 patients (response rate 35%), and anti–EGFR therapy was overall well tolerated in this group of patients. Another group reported outcomes of 5 patients with a RAS wild-type metastatic SCCA who received cetuximab with or without irinotecan. Partial responses were noted in 3 of these patients. These results provide optimism that anti–EGFR therapy can be utilized safely in the management of metastatic SCCA. However, to date, no prospective trials comparing cytotoxic chemotherapy with or without anti-EGFR therapy have been performed, and so the added benefit of agents like cetuximab in this setting remains unclear.
Vascular endothelial growth factor (VEGF) is an important mediator for angiogenesis in the development of new tumors. Bevacizumab is a monoclonal antibody that targets VEGF. Recent results of a large prospective trial in patients with metastatic cervical cancer, another solid tumor strongly associated with coinfection by HPV, compared traditional cytotoxic chemotherapy regimens with or without bevacizumab. Strikingly, patients with advanced cervical cancer who received chemotherapy in combination with bevacizumab demonstrated improved overall survival as well as higher response rates to treatment. This drug also has activity as monotherapy for patients with metastatic cancer of the cervix. Together, these results provide important rationale toward extension of these findings to the management of metastatic anal cancer. Further studies are warranted to investigate the role of anti-VEGF therapies in incurable SCCA.
Role of surgery and radiation in the management of distant metastases
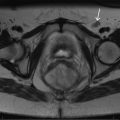
In the previously mentioned retrospective series of 77 patients at M.D. Anderson with metastatic SCCA, 2 distinct cohorts of patients were noted: patients with oligometastatic disease amenable to multimodality therapy and patients with diffuse, disseminated disease who were candidates for systemic chemotherapy only. Here, 33 patients had oligometastatic disease that was amenable to locoregional therapy, 19 with surgical resection and 14 with chemoradiation to their limited sites of distant metastases. The most frequent sites of surgical resection included liver, lung, and distant lymph nodes. Comparison of patients with metastatic SCCA here who were and were not able to proceed toward surgery and/or chemoradiation for distant tumor involvement revealed a strong survival benefit for those patients who were able to receive multidisciplinary treatment (53 months vs 17 months, P <.001). Importantly, these findings suggest heterogeneity within the population of patients with metastatic SCCA and that identifying patients with oligometastatic disease who may be amenable to surgery and/or chemoradiation is important given the possibility of improving survival outcomes with treatment approaches other than systemic chemotherapy. The authors recommend referral of such patients to major academic centers with extensive experience in the treatment of metastatic SCCA for evaluation of multimodality therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree