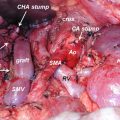
Fig. 17.1
The superior mesenteric artery (SMA) and superior mesenteric vein (SMV) are identified at the infracolic mesentery. The middle colic artery is usually divided if cancer invasion is severe
Fig. 17.2
The origins of the inferior pancreaticoduodenal artery (IPDA) and the first jejunal artery are identified by dissection of the connective tissues around the SMA from the left side
The appropriate dissection of the nerve plexus of the SMA, which means circumferential dissection, semicircle dissection, or no dissection, is controversial. The nerve plexus dissection of the SMA could cause postoperative severe diarrhea and may delay the start of the adjuvant therapy [36, 37]. Furthermore, it is reported that the semicircle dissection of the nerve plexus of the SMA could not improve the survival for the patients with resectable pancreatic cancer [36]. Therefore, the nerve plexus of the SMA may not be necessary for pancreatic cancer without invasion to the nerve plexus around the SMA. However, borderline resectable pancreatic cancer sometimes needs semicircle or circumferential dissection of the SMA to obtain the negative margins (R0). If the nerve dissection is necessary, the nerve plexus of the SMA is also dissected outside of the SMA adventitial during dissection of the connective tissues around the SMA (Fig. 17.3).
Fig. 17.3
The left side of nerve plexus of the SMA is preserved to prevent postoperative severe diarrhea
The connective tissues around the SMV also are dissected, and the inferior pancreaticoduodenal vein, first jejunal vein, Henle’s gastrocolic trunk, and middle colic vein (if necessary) are ligated and divided. Mesenteric approach is finished at the time of completion of dissection around the SMA and SMV (Fig. 17.4).
Fig. 17.4
Mesenteric approach is finished at the time of completion of dissection around the SMA and SMV
Conclusion
“Mesenteric approach” is a feasible “artery-first approach” technique during pancreaticoduodenectomy. Recent some retrospective reports described the superiority of “artery-first approach” to standard pancreaticoduodenectomy. However, further prospective studies are necessary to confirm the superiority of “mesenteric approach” pancreaticoduodenectomy.
Disclosure of Financial Interests and Potential Conflicts of Interest
We have no financial interests and potential conflicts of interest.
References
1.
2.
National Comprehensive Cancer Network. NCCN practice guideline for pancreatic cancer, version 2. 2015. Available at: http://www.nccn.org/professionals/physician_gls/PDF/pancreatic.pdf.
3.
4.
Abrams RA, Lowy AM, O’Reilly EM, et al. Combined modality treatment of resectable and borderline resectable pancreatic cancer: expert consensus statement. Am Surg Oncol. 2009;16:1751–6.CrossRef
5.
6.
7.
Gockel I, Domeyer M, Wolloscheck T, et al. Resection of the mesopancreas (RMP): a new surgical classification of a known anatomical space. World J Surg Oncol. 2007;5:44.CrossRefPubMedPubMedCentral
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree