Figure 5.1
Sestamibi scan showing persistent uptake of the radionuclide by an intrathoracic parathyroid adenoma (arrow)
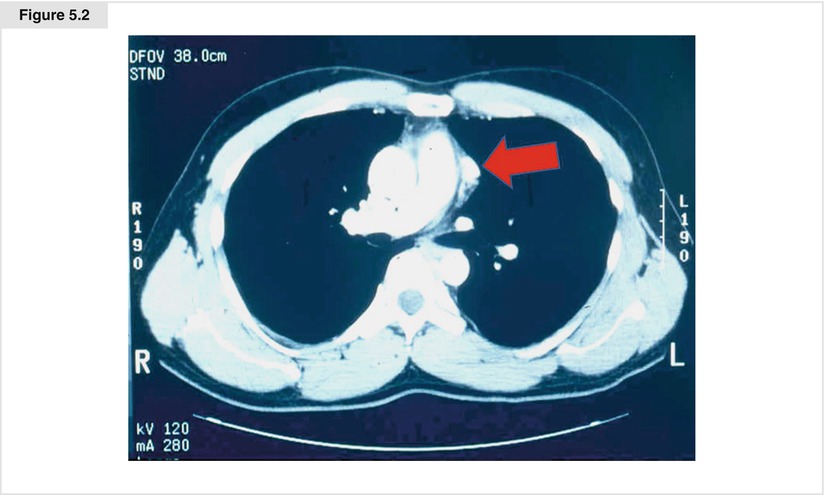
Figure 5.2
CT scan confirming the presence of a parathyroid adenoma in the mediastinum (arrow)
5.3 Intraoperative Localization and PTH Monitoring
The intraoperative use of a gamma probe may aid in localizing the parathyroid adenoma within the mediastinum. Abnormal parathyroid tissue takes up 99mTc-sestamibi more intensely and has a more delayed washout than surrounding tissue, enabling the use of the gamma probe for localization. Ex vivo radioactivity counts of greater than 20% of background may be used to confirm the presence of parathyroid tissue in the specimen [19]. Use of the gamma probe may reduce unnecessary dissection and shorten operating times [20].
Intraoperative PTH monitoring is recommended for all operations for primary hyperparathyroidism, regardless of the approach. We use the criteria for a curative resection of at least a 50% drop and a return to a normal PTH level at 5, 10, or 15 min after resection. If the PTH fails to drop, and frozen section pathologic examination of the specimen confirms the presence of parathyroid tissue, then additional hyperplastic glands must be sought in the neck or the mediastinum. In a retrospective study of 33 patients undergoing mediastinal parathyroidectomy, 7 patients (21%) presented with multiglandular disease that was only discovered because of intraoperative PTH monitoring [21].
5.4 Mediastinal Anatomy
The boundaries of the mediastinum are the parietal pleura laterally, the thoracic inlet superiorly, the superior surface of the diaphragm inferiorly, the sternum anteriorly, and the anterior longitudinal spinal ligaments posteriorly. The anterior mediastinal compartment is bounded posteriorly by a plane along the anterior surface of the great vessels and the pericardium. The contents of the anterior mediastinal compartment include the thymus, anterior mediastinal lymph nodes, fat, and on occasion a retrosternal thyroid or ectopic parathyroid gland. The middle (visceral) compartment contains the trachea, proximal main stem bronchi, esophagus, pericardium, heart and great vessels, lymph nodes, thoracic duct, and the phrenic, vagus, and sympathetic nerves. The posterior compartment shares the same lateral, superior, and inferior boundaries as the anterior compartment. It begins at the vertebral bodies and extends to the transverse vertebral processes. The posterior compartment contains the peripheral intercostal nerves and sympathetic and parasympathetic ganglia.
5.5 Parathyroidectomy Using Video-Assisted Thoracoscopic Surgery (VATS)
Thoracoscopy is performed with the patient under general anesthesia, using a double-lumen endotracheal tube. Arterial lines are only placed selectively. A Foley catheter may be inserted to monitor urine output, as procedures will vary in length and may take longer than anticipated. Baseline circulating PTH levels should be drawn prior to incision.
The lateral decubitus position offers the best exposure for middle and posterior mediastinal ectopic glands (Fig. 5.3). Either a left or right approach may be used for mediastinal parathyroidectomy, depending on the exact location of the aberrant gland. For ectopic glands located in the anterior or anterior superior mediastinum, a modified lateral decubitus position with an angle 45 to 60 degrees from the supine will assist with exposure by allowing gravity to drop the collapsed lung away from the anterior mediastinum. Alternatively, the patient may be left supine with a rolled blanket beneath the back on the operative side, as done for thoracoscopic thymectomy (Fig. 5.4). Port placement and instrumentation will vary from patient to patient, based on the location of the aberrant gland. For ectopic glands in the middle and posterior mediastinum, a 5-mm port is placed in the 5th or 6th intercostal space posteriorly, after infiltration with 0.5% bupivacaine with epinephrine. A 5-mm, 30° scope is placed through the 5-mm port site and the pleural space is explored for any adhesions, effusion, or other abnormality. Next, a thoracic port is placed between the midaxillary and posterior axillary lines, between the 7th and 8th intercostal spaces, based on visualizing the best location for optimal viewing of the planned operative site with the camera. Prior to insertion of the port, an intercostal block with 2–3 mL of 0.5% bupivacaine with epinephrine is performed beneath the insertion site. A 12-mm thoracic port is inserted, and a 10-mm thoracoscope is placed though it. Both 0° and 30° thoracoscopes are acceptable and provide good visualization (we most often use a 30° scope). Next, a 12-mm thoracic port is placed in the 4th or 5th intercostal space in the anterior axillary line after an intercostal block has been administered with 2–3 mL of 0.5% bupivacaine with epinephrine. This triangulated approach with the camera most inferior and between the other two port sites provides excellent visualization of the middle and posterior mediastinum and reduces “sword-fighting” between the instrument sites and the camera.
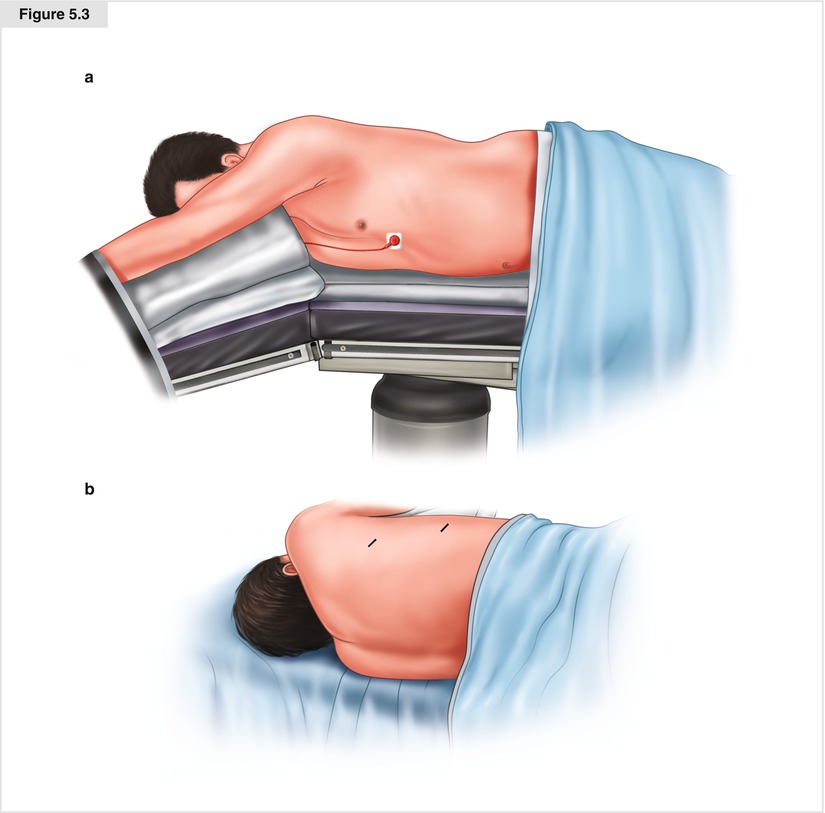
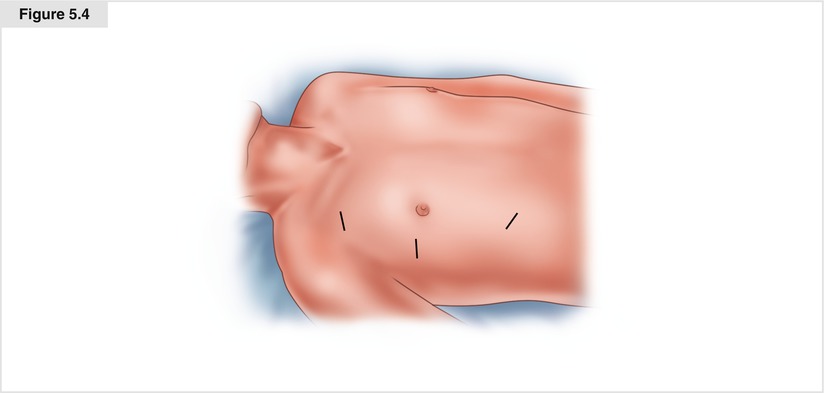
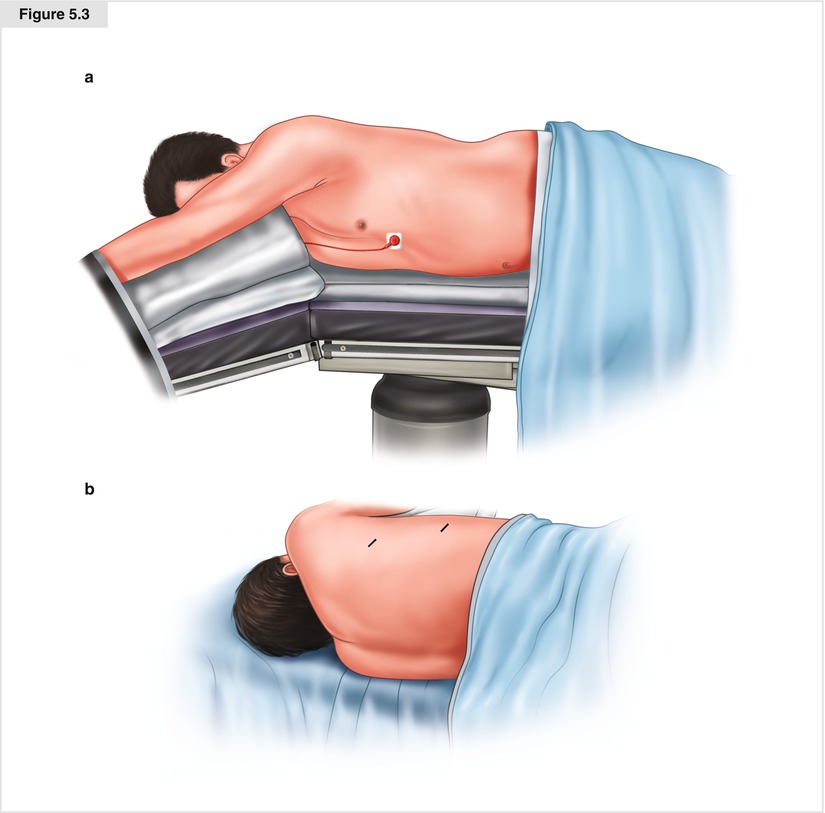
Figure 5.3
The patient is placed in a lateral decubitus position with a gel roll placed in the axilla. (a) Shows the right lateral decubitus position; (b) shows the left lateral decubitus position. The inked lines show portions of the first two port sites
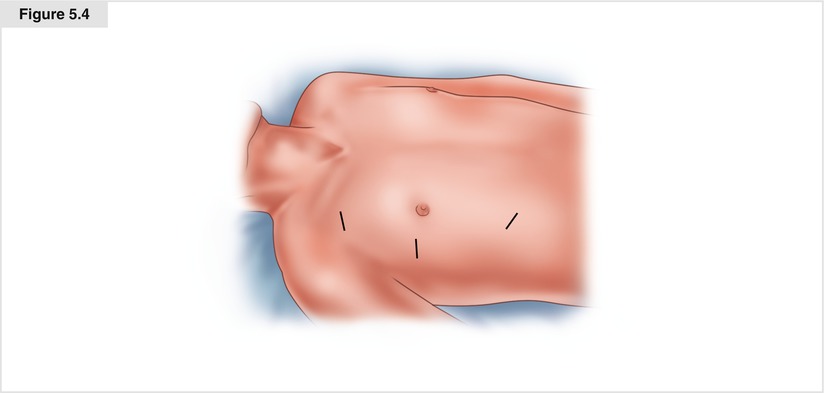
Figure 5.4
A supine position with a roll placed beneath the back on the operative side for 10°–15° elevation also can be used. The inked lines denote port placement
For ectopic glands in the anterior or anterior superior mediastinum, the first port is typically placed in the 5th intercostal space in the midaxillary line after infiltration with 0.5% bupivacaine with epinephrine. A 12-mm thoracic port is inserted and a 10-mm thoracoscope is placed though it. Both 0° and 30° thoracoscopes are acceptable and provide good visualization; we most often use a 30° scope. For lesions best approached through the left chest, the ports are placed in the left chest. Likewise, for lesions best approached through the right chest, the ports are placed in the right chest. The lung on the operative side is isolated by the anesthesia service, allowing the lung to deflate. We utilize CO2 insufflation at a pressure of 6 to 8 mm Hg to assist in exposure and collapse of the lung. If necessary, the lung is retracted away from the operative field. Additional ports should be added after visual exploration of the chest; their optimal location is determined on a procedure-by-procedure basis. Depending on the location of the lesion, the thoracoscope and all other ports should be placed within a 180° arc, which will reduce mirror imaging and instrument overlap. For anterior masses, the ports are placed more anteriorly. The second port (5 mm) is placed at the anterior axillary line in the 2nd or 3rd intercostal space. The third port (12 mm) is placed in the 7th or 8th intercostal space in the anterior axillary line. Three ports (one 5 mm and two 12 mm) are sufficient for nearly all patients.
The gland should be sought in the location determined by preoperative imaging. For glands located in the anterior superior mediastinum, the mediastinal pleura behind the sternum is incised medial to the internal thoracic artery and vein (Fig. 5.5). This incision can be extended superiorly (to the level where the internal thoracic vein turns posteriorly to join the innominate vein on either the right or left side) and inferiorly (down to the diaphragm). This dissection will allow the mediastinum to fall away from the sternum, providing additional working space (Fig. 5.6). Next, the mediastinal pleura adjacent to the pericardium is incised to allow mobilization of the anterior mediastinal fat and thymus. Both visual examination and use of the gamma probe can be used to locate the gland (Fig. 5.7). Long probes can be placed through the inferior 12-mm port to assist in localization of smaller glands. The area of dissection should be based on the preoperative localization. In other words, this procedure is not an exploration but a targeted resection. Dissection can be performed bluntly and/or with hemostatic devices such as a protected-tip cautery, harmonic scalpel, or LigaSure™ (Covidien, Dublin). Larger glands are often visible and are removed with a 2-cm rim of surrounding mediastinal fat, if they are located in the anterior mediastinum (Fig. 5.8). If the glands are not readily visible, all anterior mediastinal fat from the level of the innominate vein down to the diaphragm is removed, and the search for the gland can occur on a back table. Ectopic glands in the middle or posterior mediastinum are typically directly visible and are dissected out with the technique used for complete lymph node dissection. Care should be taken to avoid rupture of the parathyroid capsule, which can lead to seeding and recurrent hyperparathyroidism or parathyromatosis. The vascular pedicle of the gland may be ligated and divided with clips, but most often it is readily controlled with a hemostatic device. The specimen should be placed in a plastic retrieval bag and withdrawn through the most inferior port, as this is usually the widest intercostal space. A chest tube is placed to the apex of the pleural space through the most inferior port site. This tube can be removed 24 h later or when clinically indicated. The two 12-mm port sites are closed in three layers with absorbable sutures. We use a 2-0 Vicryl costal suture, a 3-0 Vicryl subcutaneous suture, and a 4-0 Monocryl subcuticular stitch, and then we seal the sites with glue. The 5-mm port site is closed with a 3-0 Vicryl subcutaneous layer and a 4-0 Monocryl subcuticular suture and is sealed with glue.