Management of Toxic Effects of Chemotherapy
Chemotherapy, like any medication, has the potential to cause side effects. Unique to these agents, however, are the nature and extent of the injury they are capable of inflicting. Chemotherapeutic agents are highly toxic and have narrow therapeutic indices. Although these agents exhibit a certain degree of specificity for malignant cells, they cannot discriminate effectively between normal and malignant cells. Consequently, other rapidly proliferating cells, such as the bone marrow cells, the spermatogonia, and the gastrointestinal crypt epithelium cells, are very vulnerable. Cytotoxic agents can induce virtually every type of pathology on the organ systems. The clinical manifestations can vary in onset from acute to chronic and in severity from mild to severe. Most of these symptoms are reversible; some are cumulative and life-threatening.
The need to curb the growth of cancer cells most often outweighs the disadvantages produced by these side effects; patients and prescribers often choose to accept these expected but undesirable and often life-threatening side effects to curtail malignant cell growth, reduce the tumor burden, and increase the potential for cure.
New and improved drugs have entered the market at a rapid rate in the past 3 years. The “fast-track” approach by the Food and Drug Administration has allowed speedier approval of promising experimental drugs for cancer patients. More successful outcomes with this wide spectrum of cytotoxic agents have been achieved because barriers to high-dose
chemotherapy and combination modalities can be minimized with the use of growth factors. The use of chemopro-tectants has been favorable, and more sophisticated technology abounds. All of these factors contribute to better treatment options for oncology patients. However, with these benefits come attendant risks.
chemotherapy and combination modalities can be minimized with the use of growth factors. The use of chemopro-tectants has been favorable, and more sophisticated technology abounds. All of these factors contribute to better treatment options for oncology patients. However, with these benefits come attendant risks.
Chemotherapy-induced toxicities have important consequences for the clinician and the patient. Serious concern about the myriad adverse effects can limit the use of potentially effective drugs as primary agents or adjuvants for certain malignancies and as retreatment agents after primary use. Risks and quality-of-life issues can deter patients from complying with the treatment plan or seeking more aggressive regimens. The physical and psychological assault from the chemotherapy experience on an already burdened host can be extremely difficult. Therefore, astute management of these toxicities is of paramount importance so that the goals of cancer treatment will not be delayed. By understanding the pathophysiology of these toxicities, the nurse can develop strategies to minimize the distressing and sometimes life-threatening consequences of chemotherapy.
This chapter focuses on the more common chemotherapy-induced toxicities on the various body systems, their management, and patient education considerations. Oncology nurses play a pivotal role in managing these toxicities and in teaching the patient to implement self-care interventions at home.
Bone marrow transplantation and the use of colony-stimulating factors are hematologic strategies used in the treatment of cancer, enabling dose intensification. These techniques increase the sensitivity of myocardial cells to chemotherapy, causing an increased potential for acute, chronic, and possibly irreversible cardiac damage. Adverse effects to the cardiac system are mostly associated with an-thracycline therapy, particularly doxorubicin and daunorubicin. Cardiac alterations may be acute or chronic, and manifestations may vary from subtle ECG changes to life-threatening cardiomyopathies such as arrhythmias, congestive
heart failure, and ischemia. Cardiotoxicity may be potentiated by concomitant mediastinal radiation and the use of other potentially cardiotoxic drugs, such as high-dose cyclophosphamide. Other risk factors are age (children and adults older than 50 years are more affected), preexisting cardiac disease, smoking, malnutrition, renal and hepatic impairment, and a history of hypertension.
heart failure, and ischemia. Cardiotoxicity may be potentiated by concomitant mediastinal radiation and the use of other potentially cardiotoxic drugs, such as high-dose cyclophosphamide. Other risk factors are age (children and adults older than 50 years are more affected), preexisting cardiac disease, smoking, malnutrition, renal and hepatic impairment, and a history of hypertension.
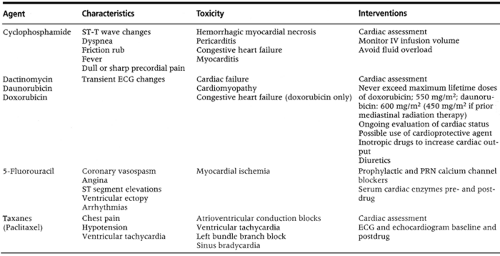
The clinical presentation of cardiotoxicity resembles that of congestive heart failure. The patient has dyspnea and a non-productive cough. Other manifestations are distended neck veins, ankle edema, tachycardia, and cardiomegaly. The use of the new cardiac protectant, dexrazoxane, in doxorubicin therapy for metastatic breast cancer may help diminish the incidence of cardiac toxicity. In severe cases, the chemotherapeutic agents should be discontinued and supportive measures provided (Table 5-1).
MANAGEMENT AND PATIENT EDUCATION
Monitor the patient’s cardiac function by obtaining cardiac enzymes, multigated radionuclide angiography, and electrocardiograms before and throughout treatment.
Obtain baseline assessments of the peripheral and apical pulse, blood pressure, the presence of edema, and difficulty with breathing or chest pain.
Teach the patient to report signs and symptoms indicative of early cardiac problems, such as tachycardia, dyspnea, and dizziness.
Stress the importance of a low-salt diet, fluid restriction to 1 L/day, and rest periods if the patient develops congestive heart failure.
Administer cardioprotectants such as dexrazoxane if ordered.
Limit the cumulative chemotherapy dose according to guidelines, with dose reductions if the patient is receiving concomitant irradiation.
Instruct the patient about the importance of taking digoxin and diuretics and the associated side effects if these medications are ordered.
Teach the patient to avoid alcohol and tobacco because of their stimulant effect on the heart muscle.
Assess the patient’s activity and exercise levels and develop an appropriate plan.
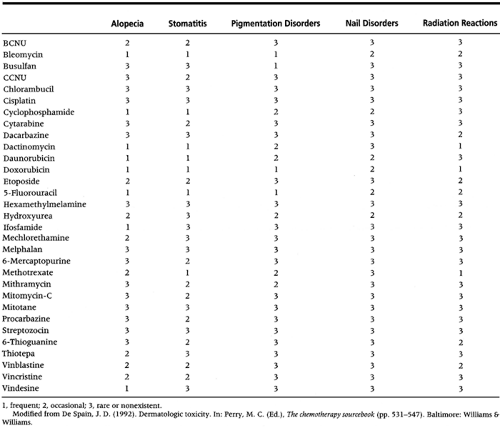
Chemotherapy can induce alterations of the integumentary system. These may be generalized or localized reactions and are often manifested on the skin, its appendages, and mucosal surfaces. Cutaneous reactions vary in site, onset, severity, and duration depending on the kind of cytotoxic agent used (Table 5-2). Cutaneous toxicity is generally transient because the skin regenerates its epidermal layer in 30 days. Unless the cutaneous reactions are severe, involving tissue necrosis, cutaneous toxicities eventually resolve. However, cutaneous reactions should be carefully evaluated because they can severely affect the patient’s physical and mental health. Cutaneous toxicity can alter the skin’s ability to protect the body against fluid loss, can alter temperature regulation, and can diminish sensations of pain and touch. Because most cutaneous manifestations are visible, they can have a tremendous impact on the patient’s self-image and how others perceive him or her. Other than the use of cytotoxic agents, especially at high doses, potential causes for cutaneous symptoms are infection, cutaneous malignancy, metastatic spread, graft-host interaction, nutritional disorders, and other drugs, such as antibiotics and analgesics.
The chemotherapy cutaneous reactions include the following:
Alopecia
Acral erythema
Hyperpigmentation
Nail changes
Photosensitivity
Radiation enhancement and recall
Extravasation, hypersensitivity reactions, and mucositis, which are the acute and most serious of the cutaneous reactions, are discussed in another section.
ALOPECIA
Of all the complications of chemotherapy, the most devastating is hair loss. It is a visible and constant reminder of cancer.
The noticeable hair loss has a negative impact on one’s body image. To a woman who has had a mastectomy or hysterectomy, alopecia represents an added threat to her femininity. To a young adolescent, the premature “baldness” can damage his or her relationships with peers. In addition to the scalp hair, the eyebrows, beard, pubic hair, and axillary hair can also be lost.
There are approximately 100,000 hair follicles in the body. These hair follicles undergo the phases of anagen (growth), catagen (transition), and telogen (dormancy). About 85% to 90% of hair follicles are in the anagen phase; the remainder are in the telogen phase or in a brief transitional state (Jacubovic & Ackerman, 1985). When a hair follicle enters the anagen phase, the upward growth of the new hair causes the dormant hair to shed. As a result of this growth and dormancy cycle, a normal person usually sheds 100 scalp hairs daily. The active hair bulbs duplicate every 12 to 24 hours, resulting in a daily growth of the hair shaft of 0.37 mm (Crounse & Van Scott, 1960). With high-dose chemotherapy, the hair follicles that are in the anagen phase atrophy, causing the hair to fall out spontaneously. Alopecia can also occur from the narrowing of the hair shaft, which causes defective and weak hair that is prone to breakage. This leads to thinning of the hair in various degrees and usually occurs with standard-dose chemotherapy.
The degree of alopecia may be minimal (less than 25% hair loss), moderate (25% to 50%), or severe (more than 50%). The degree depends on the drug or combination of drugs used, the dose, the serum half-life of the agent, and the duration of the infusion time. Hair loss is usually experienced within 2 weeks after chemotherapy administration, and hair regrowth may take 3 to 5 months after chemotherapy.
Management and Patient Education
Prepare the patient for the degree of possible hair loss and the time frame for regrowth.
Allow the patient to verbalize, acknowledge the meaning and impact of the hair loss on his or her body image and lifestyle, and plan ways to deal with the potential hair loss.
Do not recommend the use of a scalp tourniquet and hypothermia: these procedures may produce sanctuary sites or a refuge for circulating tumor cells.
Emphasize adequate nutrition. The use of vitamin E or gelatin supplements has not been proven to be of benefit.
Implement anticipatory interventions such as early referrals to a wig specialist. Wigs are tax-deductible and are covered by medical insurance. Encourage the patient to see a wig specialist during the early phase of chemotherapy so that the specialist can determine the natural color and style.
Refer the patient to the American Cancer Society’s “Look Good, Feel Better” program and other support groups.
Assure the patient that alopecia is reversible and that regrowth will occur when chemotherapy is stopped. Review time frames. Provide emotional support, because the process can be slow and new growth may not be appreciable until after a few months.
Teach proper techniques for hair care, such as:
Use mild shampoos; avoid perming, peroxide coloring, or chemical treatments.
Minimize the use of heat, rollers, and vigorous brushing. Teach the patient to “finger-comb” the hair instead of using a hair brush.
Wear attractive turbans, scarves, and hats.
Consider cutting the hair to a shorter length.
ACRAL ERYTHEMA (HAND-FOOT SYNDROME)
The agent most implicated in this condition is high-dose cy-tarabine; other neoplastic agents can also produce this syndrome when given at high doses (methotrexate, 5-fluor-ouracil, hydroxyurea, capecitabine, and etoposide). The initial reactions are burning, swelling, tingling, and sharply demarcated erythema of the palm, the fingers, and the soles of the feet, which progress to blistering and desquamation of the affected areas. The scalp and chest can also be affected. Patients complain of tingling in the hands and feet progressing to flank pain when handling objects or walking.
HYPERPIGMENTATION
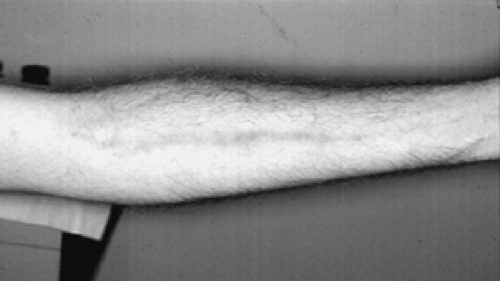
The pathogenesis of altered pigmentation is poorly understood. It is believed to be due to a deviation in the amount and distribution of melanin and the direct stimulation of the melanocyte (Fitzpatrick & Hood, 1988). There is an increased incidence of hyperpigmentation in dark-skinned persons. It is usually manifested on the skin, but other areas, such as the nails, hair, and oral mucous membranes, have also been reported. Hyperpigmentation disappears with time, and the changes are rarely permanent. One of the cutaneous complications associated with 5-fluorouracil is serpiginous hyper-pigmented streaks overlying the veins used for administration in the absence of the usual warning signs of phlebitis (Fig. 5-1). 5-fluorouracil is thought to produce endothelial fragility, which allows the drug to escape into the tissues, resulting in hyperpigmentation of the overlying skin (Hrushesky, 1980). A similar reaction of hyperpigmented linear streaks of the veins has also been reported with bleomycin (de Bast et al., 1971). Among African Americans, hyperpigmentation of the oral mucosa and the tongue has been noted after administration of doxorubicin, busulfan, and cyclophosphamide (Dunagin, 1982).
Management and Patient Education
Assess the patient’s baseline skin condition and evaluate his or her skin care regimen.
Assure the patient that hyperpigmentation will resolve in time.
Ask the patient about concomitant medications that may influence skin reactions.
Instruct the patient to use sunscreen.
Monitor the infusion site when administering 5-fluorouracil; discontinue the infusion at the first sign of irritation and restart a new line.
NAIL CHANGES
Certain chemotherapeutic agents can cause alterations to the nails. Not as significant and distressing as the other cutaneous reactions, these changes include brittleness, banding, and hyperpigmentation of the matrix of the nails. They are temporary and resolve when chemotherapy is completed. Hyperpigmentation of the nail is due to the deposition of melanin in the nail plate. Blue discoloration of the nail plate has also been observed after the administration of 5-fluorouracil and doxorubicin. Transverse banding—multiple white horizontal lines along the fingernails—has also been reported. Another abnormality in the nail consists of thin transverse grooves across the nail plate, called Beau’s lines. This is also seen in patients with myocardial infarction and may involve all 20 nails. Onycholysis (partial separation of the nail from the nail bed) has been noted in patients receiving 5-fluorouracil, doxorubicin, and bleomycin (De Spain, 1992).
Management and Patient Education
Assess the patient’s nails before chemotherapy administration.
Advise the patient of potential changes in the nails and ask him or her to report any changes. These usually occur 5 to 10 weeks after chemotherapy.
Reassure the patient that the changes are usually temporary.
Cover nails with nail polish.
Encourage the patient to wear gloves if he or she is embarrassed about the appearance of the nails.
Teach the patient about good nail care:
Avoid cutting cuticles.
Apply oil to nails.
Do not cut the nails too close to the nail bed.
PHOTOSENSITIVITY
Photosensitivity is caused by cytotoxic agents that have radiosensitizing properties. The cutaneous reaction is thought to occur by means of a phototoxic mechanism involving UVB light (De Spain, 1992). Photosensitivity is manifested as an exaggerated sunburn accompanied by urticaria and stinging; it resolves with hyperpigmentation.
Management and Patient Education
Review medications that are associated with photosensitivity.
Instruct the patient to take the following precautions:
Avoid exposure to direct, indirect, and artificial sunlight.
Use protective sunblocks (SPF 30 or greater), applied at least 15–30 minutes before sun exposure.
Wear protective clothing, wide-brimmed hats, and long-sleeved shirts.
RADIATION ENHANCEMENT AND RECALL
Cutaneous reactions may occur as a result of the synergistic effect of irradiation and cytotoxic agents on both normal and target cancer tissues. Enhancement reactions occur if chemotherapy is administered within a week of irradiation. Recall reactions may happen within weeks or months to even years after radiation; however, they appear more frequently with shorter time intervals and high-dose chemotherapy. These reactions can occur in the skin, lung, heart, and gastrointestinal tract. They are manifested by erythema, blisters, hyperpigmentation, edema, vesicle formation, exfoliation, and sometimes ulcers. The management of radiation recall and enhancement effects is similar.
Management and Patient Education
Consider longer intervals between the chemotherapy administration and the radiation therapy, if possible.
Perform a thorough skin assessment; note color, moisture, and turgor. Instruct the patient to report any changes in the skin.
Teach the patient to avoid trauma or irritation to the affected areas.
Instruct the patient on good skin care to maintain skin integrity:
Wash the skin with mild soap (e.g., Dove, Ivory) or cleanser (Cetaphil) and tepid water.
Use a soft cloth, avoid rubbing, and use a gentle patting motion to cleanse and dry the area.
Use sunscreen (SPF 30 or greater).
Wear loose and nonconstrictive clothing; avoid materials that might irritate the skin.
Use mild detergents when laundering clothes.
Avoid extremes in temperature.
Do not use adhesives or occlusive dressings over affected skin. Expose the area to air. h.If shaving is necessary, use an electric razor.
Do not use any skin care product unless it is prescribed by the nurse or doctor.
If the area gets infected, gentle débridement might be necessary. An antimicrobial ointment can be used to keep the area moist. Cover with a nonadherent dressing.
Chemotherapy can profoundly affect the gastrointestinal (GI) tract. Ninety percent of the GI crypt epithelium is composed of undifferentiated cells and goblet cells found in the small intestines. These are mitotically active cells and as such are vulnerable to cytotoxic attack. Because the GI tract functions as the major site of nutritional intake, and because malnutrition, anorexia, and cachexia are associated with cancer, any further insult to the functioning of the GI tract can severely compromise the host.
The common chemotherapy-induced toxicities to the GI system are nausea and vomiting, anorexia, mucositis, constipation, and diarrhea.
NAUSEA AND VOMITING
Among all the symptoms that are dreaded by patients receiving chemotherapy, nausea and vomiting are considered to be at the top of the list. It is thought that 70% to 80% of patients
receiving chemotherapy have some degree of nausea and vomiting. Nausea often precedes vomiting and is an unpleasant feeling of the need to vomit. It is a separate event from vomiting and may or may not result in vomiting. Retching, also known as dry heaves, is another phenomenon that may or may not accompany emesis. It is caused by the rhythmic contraction of the abdominal and respiratory muscles. Vomiting is the forceful expulsion of the gastric contents through the mouth. It is accompanied by weakness, pallor, tachycardia, decreased blood pressure, and increased respiration.
receiving chemotherapy have some degree of nausea and vomiting. Nausea often precedes vomiting and is an unpleasant feeling of the need to vomit. It is a separate event from vomiting and may or may not result in vomiting. Retching, also known as dry heaves, is another phenomenon that may or may not accompany emesis. It is caused by the rhythmic contraction of the abdominal and respiratory muscles. Vomiting is the forceful expulsion of the gastric contents through the mouth. It is accompanied by weakness, pallor, tachycardia, decreased blood pressure, and increased respiration.
The exact mechanism of chemotherapy-induced emesis is not completely understood. It is postulated that emesis is induced by stimulation of the true vomiting center (TVC), the nucleus tractus solitarius, located in the general area of the lateral reticular formulation of the fourth ventricle. The physiologic stimulation of the TVC is mediated by neurotransmitters, including serotonin (5-HT3), dopamine, norepinephrine, and histamine. The receptor sites for these transmitters are located in the chemoreceptor trigger zone (CTZ) and the GI tract. The TVC receives afferent impulses from four sources (Borison & Wang, 1953):
The CTZ, located in the area postrema in the brain stem, responds directly to chemical toxins (chemotherapy) in the blood and the cerebrospinal fluid.
The GI tract at the level of the small intestine is the primary location of the serotonin receptor, which when stimulated sends impulses by sympathetic and afferent pathways.
The higher cortical centers transmit psychogenic stimuli.
The vestibular apparatus of the middle ear (motion sickness) is also involved.
When impulses from any of these four trigger points exceed the threshold, vomiting occurs.
Patient characteristics and prognostic factors that affect the incidence of nausea and vomiting include:
Age: Younger patients experience more nausea and vomiting than older patients.
Gender: A higher incidence in women is believed to be due to the more highly emetogenic drugs given to women and lesser alcohol intake.
Alcohol intake: High alcohol intake has a positive effect on control of emesis.
History of motion sickness or severe emesis during
pregnancy: These patients are more susceptible to chemotherapy-induced nausea and vomiting.
Anxiety, expectations of severe side effects, and previous chemotherapy experience are other predisposing factors.
Food intake, change in taste sensations, and the amount of sleep before chemotherapy can affect the incidence of nausea and vomiting.
Patterns of chemotherapy-induced emesis are anticipatory, acute, delayed, and refractory.
Anticipatory Emesis
Anticipatory emesis is a conditioned or learned aversion to chemotherapy-related cues. Any stimulus (sight, smell, place) elicits a classic pavlovian reflex, even in the absence of cyto-toxic drug administration. Approximately 10% to 44% of chemotherapy patients experience anticipatory nausea and vomiting (Morrow et al., 1991). The following risk factors are associated with anticipatory nausea and vomiting:
Severe posttreatment side effects
Age younger than 50 years
History of motion sickness
Anxiety and depression
Tastes and odors
Schedule and number of chemotherapy cycles
The best intervention for this type of emesis is prevention—that is, giving the patient the best antiemetic regimen during the initial drug cycle to avoid any untoward associations. Behavioral techniques such as guided imagery, relaxation, hypnosis, and distraction have also been proven to be beneficial. Antiemetics are ineffective for acute emesis.
Acute Emesis
Acute emesis is the most common and most studied emetic syndrome. It may happen minutes after drug exposure but usually occurs 2 to 6 hours after treatment. Most of the research in antiemetic therapy has been conducted to determine the best regimen for this type of emesis.
Delayed Emesis
The mechanism for delayed emesis is unclear. It persists for 1 to 4 days after chemotherapy administration. It is usually associated with high-dose regimens of cisplatin and combination regimens of cyclophosphamide and an anthracycline. Although
it is not as distressing as acute emesis, it may severely affect the patient’s food intake and prolong the hospital stay.
it is not as distressing as acute emesis, it may severely affect the patient’s food intake and prolong the hospital stay.
Refractory Emesis
Refractory emesis refers to emesis that does not respond to antiemetic therapy. Patients with this type of emesis usually respond if an anxiolytic agent is added to the regimen.
Management and Patient Education
PHARMACOLOGIC APPROACHES
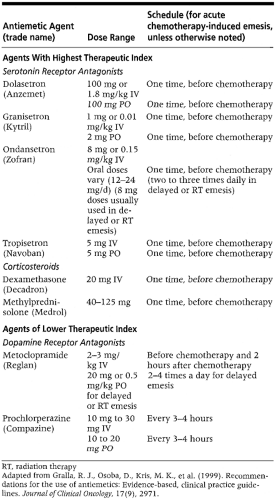
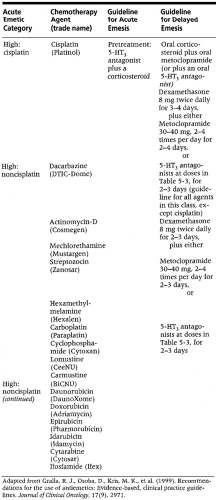
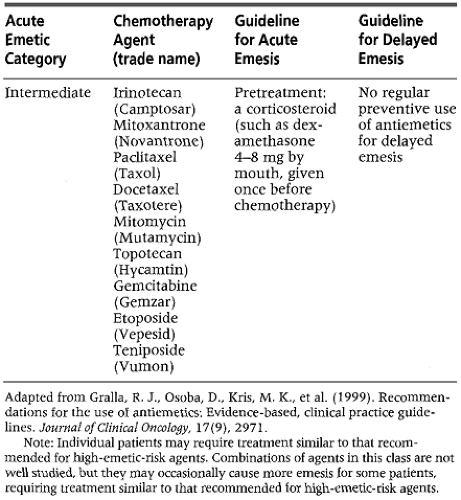
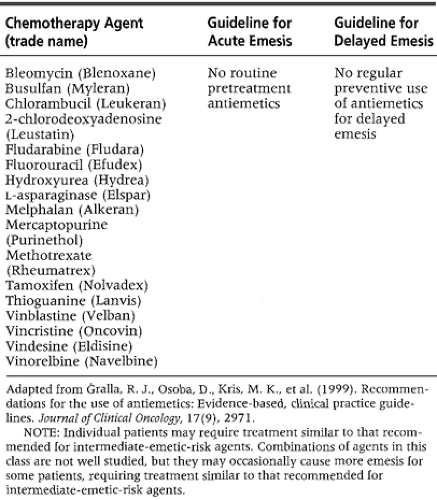
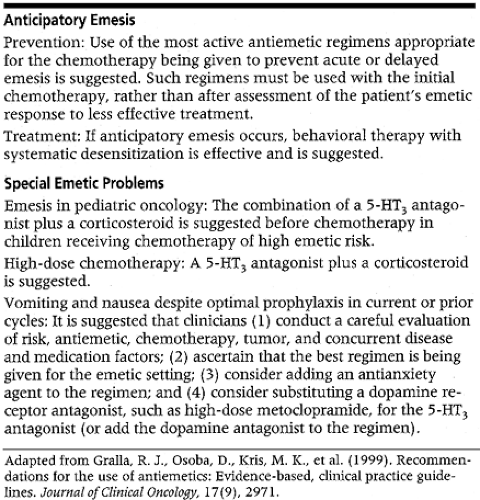
The degree and incidence of emesis depend on the emeto-genic potential of the drug, the dose, and the administration schedule. Recent advances in antiemetic therapy have provided regimens that have lessened the incidence and degree of nausea and vomiting, allowing better and more affordable control of treatment-related emesis. In 1999, the American Society of Clinical Oncology’s panel of experts developed clinical practice guidelines for antiemetic therapy (Gralla et al., 1999). Table 5-3, Table 5-4, Table 5-5, Table 5-6 and Table 5-7 give the evidence-based recommendations of this group.
Serotonin receptor antagonists are an important class of antiemetic drugs that have provided effective emetic control with minimal side effects. These agents include dolasetron, granisetron, ondansetron, and tropisetron. All of these agents are equally effective and act in a similar fashion as antagonists of the 5-HT3 receptor. They are preferable to metoclopramide because of the absence of central nervous system effects, extrapyramidal reactions, and sedation. This mild side effect profile is particularly attractive for younger patients. The side effects noted with the serotonin antagonists are slight headache, mild asymptomatic transaminase elevation, and constipation (most common adverse effect).
Corticosteroids are valuable and have a high therapeutic index, especially in acute emesis control. They are frequently prescribed with single-agent use in low-risk settings but are also effective when combined with serotonin receptor antagonists for patients receiving highly emetogenic chemotherapy.
Metoclopramide works as a serotonin antagonist but is also thought to have substantial activity by the dopamine receptor pathway, which explains the extrapyramidal reactions. It is less expensive than the serotonin antagonists but as effective at higher doses. Its side effects are acute dystonic reactions, akathisia, and sedation.
The other antiemetic agents—phenothiazines (prochlor-perazine, thiethylperazine), butyrophenones (haloperidol, droperidol), and cannabinoids (dronabinol, nabilone, levo-nantradol)—are considered to be substantially lower in efficacy. They have more side effects; phenothiazines cause orthostatic hypotension.
Adjunctive medications such as benzodiazepines (lorazepam) and antihistamines (diphenhydramine, hydroxyzine, benz-tropine) may be added to an antiemetic regimen but should not be used alone as antiemetic agents. Diphenhydramine is more commonly used to prevent extrapyramidal reactions.
NONPHARMACOLOGIC APPROACHES
Try the following dietary interventions
Eat foods cold or at room temperature; smells from hot foods might induce nausea or vomiting.
Try eating frequent light meals throughout the day. Rinse the mouth to remove the unpleasant taste and smell of emesis.
Avoid foods that are spicy, greasy, or sweet and have strong odors.
Eat bland or sour foods.
Drink clear, cold liquids such as apple juice, ginger tea, lemonade, Gatorade, or cola. Sip the liquids slowly.
Avoid food intake 1 to 2 hours before and after chemotherapy.
Get enough rest in a quiet and comfortable environment.
Minimize stimuli that might precipitate an emetic response, such as strong and unpleasant odors or the sight and sounds of other patients vomiting.
Use behavioral techniques such as relaxation, guided imagery, hypnosis, or acupuncture.
Use distraction, such as listening to music, reading, watching favorite TV programs or movies, and having pleasant conversations.
Use strategies that have worked in dealing with past emetic episodes (chemotherapy-related or not).
Try the newly approved, over-the-counter, drug-free devices, such as the ReliefBand®. This device, worn like a wristband, is believed to relieve nausea and vomiting by delivering gentle electrical signals that stimulate the underside of the wrist, carrying impulses to the nervous system and affecting areas that produce nausea and vomiting.
ANOREXIA
Alterations in the cancer patient’s nutritional status can be induced by chemotherapy. These symptoms of anorexia and cachexia can severely compromise the patient’s nutritional status, which can be irreversible and fatal. Anorexia is the lack of desire to eat, accompanied by decreased food intake. It is multifactorial, caused by the abnormally increased synthesis of serotonins, which stimulates a feeling of satiety; alterations in taste and smell; cancer treatments; aversion to certain foods; and an inability to digest nutrients (Robuck & Fleetwood, 1992). In cancer, the tumor cells compete for nutrients with the normal cells. As the tumor grows, body mass decreases and the patient loses weight.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree