and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Introduction
In the 21st century, women with sickle cell disease (SCD) should expect to have successful pregnancies and healthy babies. This requires management by a multidisciplinary team which has shared knowledge, experience and expertise in managing high-risk pregnancies. The team usually includes the obstetrician, obstetric anesthetist, midwife, hematologist and sickle cell nurse specialist. If this resource is not available in a local hospital, we recommend that the pregnancy is jointly managed with a regional specialist center.
The reported rates of maternal and fetal complications vary considerably between studies, but there is no doubt that they are significantly higher than in a normal pregnancy (Table 16.1). This applies to all genotypes of SCD, although women with HbSS are most at risk. Earlier series emphasized a very high rate of maternal mortality, but this is not the case nowadays, especially in large specialized centers. The frequency and severity of acute painful crises requiring hospitalization is high, particularly in the later stages of pregnancy, and this also applies to women with a mild phenotype.
Table 16.1
Maternal and fetal complications
Maternal complications | Fetal complications |
|---|---|
Acute painful crisis and acute chest syndrome | Miscarriage (throughout pregnancy) Premature labour Perinatal morbidity and mortality Stillbirth Fetal growth restriction |
Infection (especially UTI) | |
Thromboembolism | |
Pre-eclampsia and pregnancy induced hypertension | |
Increased rate of Cesarean section | |
Hospitalization during pregnancy | |
Maternal mortality |
Figure 16.1 illustrates the expected abnormality on the maternal side of the circulation and the normal appearance on the fetal side of the placental circulation.
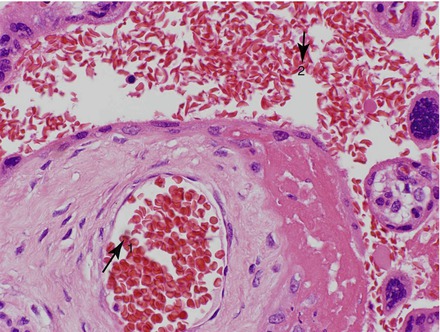
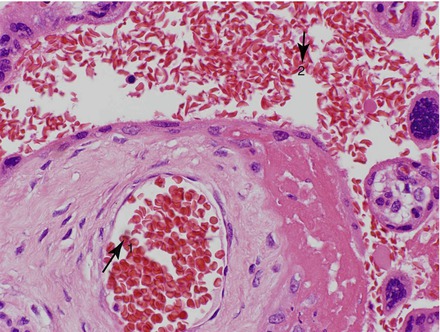
Figure 16.1
Placental histology in HbSS. The fetal blood vessel contains normal red cells (1) and the maternal blood vessel contains sickled red cells (2)
Preconceptual Care
Although pregnancies are sometimes unplanned, prior discussion and planning enables optimization of maternal health, and enables a pre-conceptual risk assessment. Knowledge of the father’s hemoglobinopathy status is obviously essential for counselling about the risk of SCD for the baby. If mother has pre-existing red cell alloantibodies arising from transfusion or previous pregnancies, there may be a risk of hemolytic disease of the newborn (HDN). Some medications (for instance hydroxyurea, iron chelating agents) are contraindicated in pregnancy as they may cause damage to the developing fetus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree