SEER (NCI)
15–29-year-old
Adolescent and young Adult Oncology Progress Review Group
15–39-year-old
NCCN
15–39-year-old
15.3 Cancer in AYAs Worldwide Including Ovarian Cancer
In the United States, 70,000 AYAs are diagnosed with cancer every year, which is seven times more than the number of cancer patients aged under 15 years [4]. In 2014, there were 5330 cancer diagnoses and 610 cancer deaths among adolescents [5]. Keegan et al. used the SEER 13 registry data from 2002 to 2006 to report the 5-year survival rates for various cancers in 45,232 children, AYAs, and older adults [2]. According to that study, the most common cancers among AYAs were breast carcinoma (14.4%), thyroid carcinoma (12.1%), and melanoma (11.2%). The cancers with the best 5-year survival rates were thyroid carcinoma (99.7%), testicular cancer (96.1%), and melanoma (95.5%). Those with the worst 5-year survival rates were hepatic carcinoma (22.8%), gastric carcinoma (26.3%), and pancreatic carcinoma (33.0%), while the other forms of cancer for which the 5-year survival rates were under 50% included high-grade astrocytoma, lung carcinoma, rhabdomyosarcoma, and acute myeloid leukemia. Ovarian cancer occurred in 919 AYAs of the 45,232 included in the study (2.0%), with a 5-year survival rate of 79.5%, which is a much better outcome than the 41.4% 5-year survival rate for older adults aged over 40 years. Thus, survival rate for ovarian cancer in AYAs is not lower than that for other cancers and is higher than that in older adult women. This high survival rate in AYAs suggests that the choice of treatment method should prioritize improving the quality of life (QOL) of the patients.
15.4 Incidence of Ovarian Cancer in AYAs in Japan
As shown in Table 15.2 the Gynecological Cancer Committee carried out a study on 2832 ovarian cancer patients who had started treatment in 2009 at 182 institutions according to clinical statistics. Patients who underwent preoperative chemotherapy and those whose stage was unknown were excluded. Included patients were classified into one of three age groups (under 19, 20–39, and over 40 years), and their ovarian cancer stage was compared. Of the total 2832 patients with ovarian cancer, 25 (0.88%) were aged under 19 years, 283 (10.0%) were aged 20–39 years, and 2524 (89.1%) were aged over 40 years, with the latter accounting for over 90% of the cases. Proportion of patients aged under 39 years with ovarian cancer was 10.88%, and those aged under 19 years was only 0.88%, indicating that this disease is extremely rare in the latter age group. An investigation of the characteristics of ovarian cancer by age group found that of the 2524 patients aged over 40 years, 1152 (45.6%) had Stage I, 275 (10.9%) had Stage II, 884 (35.0%) had Stage III, and 213 (8.5%) had Stage IV cancers. Stages I and III were the most common cancer stages, which is also similar to the general statistics for ovarian cancer, with little difference between the proportions of Stage I and Stage III patients. Of the 308 patients aged under 39 years, 204 (66.2%) had Stage I, 27 (8.8%) had Stage II, 66 (21.4%) had Stage III, and 11 (3.6%) had Stage IV cancers. For the patients aged over 40 years, most cancers were discovered at either Stage I or III, but among those aged under 39 years, a higher proportion was discovered at Stage I. In terms of the substaging of Stage I ovarian cancers among those aged under 39 years, 84 patients (27.2%) had Stage IA, 2 (0.6%) had Stage IB, and 118 (38.3%) had Stage IC cancers, with Stage IC tending to be more common. Further, an investigation of those aged under 19 years (25 patients) found that 18 (72%) had Stage I, 0 (0%) had Stage II, 5 (20%) had Stage III, and 2 (8%) had Stage IV cancers, with a higher proportion of Stage I cancers compared with the other two age groups.
Table 15.2
Characteristics of ovarian cancer stage by age group (Data of JSOG)
 | Age | ~19 | 20 ~ 39 | 40~ | Total | |||
FIGO stage |  | case | % | case | % | case | % | |
I | A | 8 | 32 | 76 | 26.8 | 446 | 17.6 | 530 |
B | 1 | 4 | 1 | 0.4 | 24 | 1.0 | 26 | |
C(b) | 4 | 16 | 68 | 24.0 | 381 | 15.1 | 453 | |
C (1) | 0 | 0 | 5 | 1.8 | 27 | 1.1 | 32 | |
C (2) | 1 | 4 | 13 | 4.6 | 116 | 4.6 | 130 | |
C(a) | 4 | 16 | 23 | 8.1 | 158 | 6.3 | 185 | |
II | A | 0 | 0 | 3 | 1.1 | 28 | 1.1 | 31 |
B | 0 | 0 | 4 | 1.4 | 29 | 1.1 | 33 | |
C(b) | 0 | 0 | 11 | 3.9 | 62 | 2.5 | 73 | |
C (1) | 0 | 0 | 0 | 0 | 7 | 0.3 | 7 | |
C (2) | 0 | 0 | 3 | 1.1 | 59 | 2.3 | 62 | |
C(a) | 0 | 0 | 6 | 2.1 | 90 | 3.6 | 96 | |
III | A | 1 | 4 | 5 | 1.8 | 50 | 2.0 | 56 |
B | 0 | 0 | 10 | 3.5 | 97 | 3.8 | 107 | |
C | 4 | 16 | 46 | 16.2 | 737 | 29.2 | 787 | |
IV | 2 | 8 | 9 | 3.2 | 213 | 8.4 | 224 | |
total | 25 | 283 | 2524 | 2832 | ||||
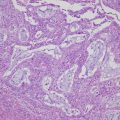
Figure 15.1 shows a summary of the yearly numbers of ovarian cancer patients reported by the Gynecological Cancer Committee of the JSOG (2003–2014) [6, 7]. An investigation on the 49,513 ovarian cancer patients registered in these annual patient reports found that 4895 (9.9%) were AYAs (this statistic included those aged under 15 years as AYAs). These 4895 AYA patients were then classified according to whether their tumor was epithelial, sex cord-stromal, germ cell, or others, and the results were plotted on a graph by age group (Fig. 15.1). As shown in Fig. 15.1, there were 363 ovarian cancer patients aged under 19 years, accounting for 7.4% of AYA ovarian cancer patients. Germ cell tumors were present in 285 cases (78.5%), followed by epithelial tumors in 64 cases (17.6%). There were 1128 ovarian cancer patients aged 20–29 years, accounting for 23.0% of AYA ovarian cancer patients. Epithelial tumors were present in 639 cases (56.6%), followed by germ cell tumors in 471 cases (41.6%). There were 3404 ovarian cancer patients aged 30–39 years, accounting for 69.5% of AYA ovarian cancer patients. Epithelial tumors were present in 2995 cases (88.0%), followed by germ cell tumors in 354 cases (10.4%). Bringing together all the AYA ovarian cancer patient data available to date, AYAs account for approximately 9.9% of all ovarian cancer patients, with the highest proportion aged 30–39 years (69.5%), followed by those aged 20–29 years (23.0%) and under 19 years (7.4%). Almost all cancer tumors in AYA ovarian cancer patients were either epithelial tumors or germ cell tumors. Epithelial tumors accounted for the great majority of cancers among those aged 30–39 years, which is similar to ovarian cancer patients aged over 40 years. For those aged 20–29 years, epithelial tumors and germ cell tumors accounted for around half of the cases each. Those aged under 19 years, however, exhibited different characteristics from those aged 20–29 years, with germ cell tumors accounting for 78.5% of the cases.
Fig. 15.1
Pathological characteristics of ovarian cancer in AYAs (Data of JSOG)
15.5 Treatment of AYA Ovarian Cancer Patients
From the perspective of improving survivorship, the most important point in the treatment of AYA ovarian cancer patients is to spare their fertility. AYAs are generally defined as those aged between 15 and 39 years, and as members of this age group who may either be considering pregnancy in the future or already want to have children, treatment methods must always be chosen with the conservation of fertility in mind.
The recommended basic fertility-sparing surgical technique for ovarian cancer patients is the ipsilateral salpingo-oophorectomy with omentectomy and laparoscopic cytology. Ipsilateral ovarian biopsy with para-aortic lymph node or pelvic lymph node dissection or biopsy and intraperitoneal biopsy may also be performed as staging laparotomy [8, 9]. Because most AYA ovarian cancer cases are known to comprise either epithelial tumors or germ cell tumors, we will provide an overview of the fertility-sparing surgery for patients with these two types of cancer tumors.
15.5.1 Treatment of Epithelial Tumors
The Japan Clinical Oncology Group (JCOG) reported data from a joint study carried out in 30 institutions in 2010 [10]. Their analysis covered 211 Stage IA or Stage IC ovarian cancer patients who underwent fertility-sparing treatments. They found that fertility-sparing surgeries are recommended for ovarian cancer patients with highly differentiated (G1) or moderately differentiated (G2) Stage IA non-clear cell carcinoma [10]. They also reported that fertility can be spared in cases of Stage IA ovarian clear cell carcinoma or G1/G2 Stage IC non-clear cell carcinoma with ipsilateral lesions as long as an adjuvant chemotherapy is performed [10]. However, the fertility-sparing surgeries are not recommended for G3 Stage I non-clear cell carcinoma and Stage IC clear cell carcinoma patients [10, 11]. Although it may be possible to preserve fertility by carrying out an adjuvant chemotherapy, this may be assumed to deplete the ovarian reserve, depending on the patient’s age. Ovarian toxicity of anticancer agents will be discussed below.
15.5.2 Treatment of Germ Cell Tumors
Germ cell tumors are rare tumors that account for less than 5% of all malignant ovarian cancers [11, 12]. However, as these tend to occur in the younger age group (10–29 years) [11, 13], are highly sensitive to chemotherapy, and are ipsilateral in over 95% of the cases [11, 14], they do not frequently provide opportunities to consider the issue of conserving the fertility of AYA ovarian cancer patients. When sparing fertility, detailed peritoneal investigation in addition to ipsilateral salpingo-oophorectomy with omentectomy and laparoscopic cytology is recommended. Some experts consider that tumor debulking is useful for patients with Stage III or IV advanced cancers, but organ damage and combined resection must be avoided and chemotherapy must be started as soon as possible. Fertility-sparing surgeries are not believed to affect the prognosis of patients with advanced cancers [15], and for younger individuals such as AYAs, a procedure that preserves ovarian function and fertility should be chosen. If the patient does not wish to conserve her fertility, the procedure for the initial surgery for ovarian carcinoma should be followed. Germ cell tumors grow rapidly; therefore, it is important that they be diagnosed early and their treatment be started rapidly.
BEP (bleomycin, etoposide and cisplatin) therapy with bleomycin, etoposide, and cisplatin is strongly recommended as a postoperative adjuvant chemotherapy [11, 16–19]. A study of malignant ovarian germ cell tumors in the early 1970s, before the development of the current chemotherapy, found that the cure rate for patients with advanced cancers who underwent surgery alone was almost 0% and that for those with Stage I cancer, it was only 5–20% [20]. Subsequent clinical trials of BEP therapy for testicular germ cell tumors, which are ten times more common than ovarian germ cell tumors, resulted in its establishment as the standard treatment for ovarian germ cell tumors as well. The reported cure rate of BEP therapy for ovarian germ cell tumors is almost 100% for early-stage tumors and over 75% even in advanced cases [18], making it highly effective as postoperative adjuvant chemotherapy. Although there are some concerns about the ovarian toxicity of chemotherapy, BEP therapy does not include any drugs that are severely toxic to the ovaries [21]. Chemotherapy can be omitted for Stage IA undifferentiated germ cell tumors and G1 Stage I immature teratomas [15, 22]. In such cases, prognosis is reportedly good if a treatment strategy of rigorous monitoring and the use of BEP therapy in the event of recurrence is followed [20]. Thus, fertility-sparing surgeries are the treatment of choice for such germ cell tumors in AYAs, and the use of BEP therapy as a postoperative adjuvant chemotherapy or recurrence therapy is recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree