Management of Hypersensitivity Reactions and Extravasation
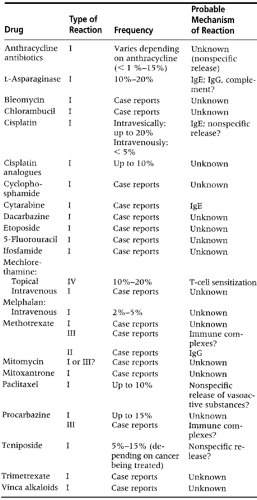
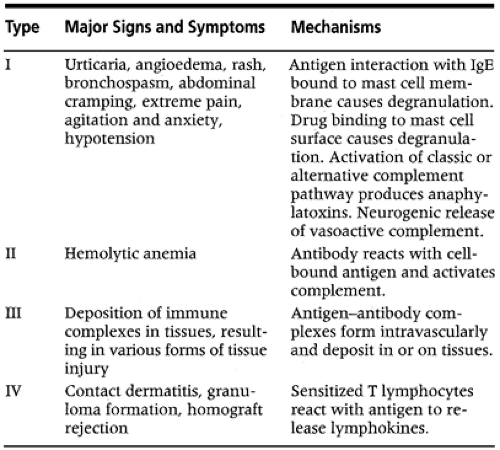
Hypersensitivity reactions (HSRs) are common in patients receiving chemotherapy. These reactions, which may be local or systemic, are believed to be immunologically mediated (Weiss, 1992a; 1992b); however, there are other mechanisms that may explain their occurrence (Table 6-1). An HSR can involve any of the four types of reactions defined by Gell and Coombs (1975; Table 6-2).
When a patient develops an HSR to a chemotherapeutic agent, most likely the drug will be stopped. The decision to use it again depends on the severity of the reaction, the treatment plan, and the availability of alternative agents.
Although it may be difficult to pinpoint the cause of the HSR, it is important to understand the reaction and its relation to the drug administered, as well as to distinguish the reaction from an immunologically mediated response. It can be difficult for the clinician to ascertain a true HSR, because some reactions mimic immunologic reactivity by direct release of mediators. Other drugs being administered concurrently, the drug formulation, and the diluents used can be contributing factors; these factors should be ruled out before diagnosing an HSR. Drugs such as cytarabine preserved in
benzyl alcohol have been reported to produce HSRs (Wilson et al., 1986).
benzyl alcohol have been reported to produce HSRs (Wilson et al., 1986).
Clinicians who administer these agents should know the clinical manifestations of an HSR so they can anticipate the symptoms and manage them quickly, whether they relate to a localized reaction or to a severe anaphylaxis reaction, which can be very alarming to the patient. The clinical manifestations are as follows:
Urticaria
Lightheadedness or dizziness
Generalized or localized itching
Abdominal cramping
Nausea
Restlessness
Periorbital or facial edema
Shortness of breath with or without wheezing
Hypotension
Chills
Chest tightness
NURSING MANAGEMENT
Obtain the patient’s allergy profile.
Inform the patient of the potential for an HSR. Instruct the patient to notify the nurse if he or she experiences any of the HSR symptoms.
Perform a scratch test or a skin test or administer a test dose for drugs with known hypersensitivity potential, such as bleomycin.
Administer premedications as ordered.
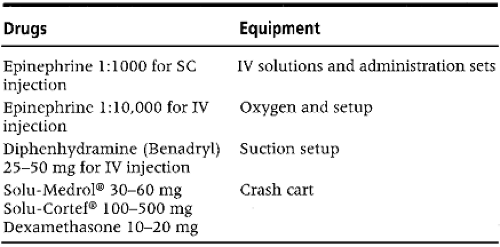
Have emergency equipment and medications ready (Table 6-3).
Obtain a physician’s orders for emergency medications before initiating the drug (Brown & Hogan, 1990).
Obtain baseline vital signs and monitor the patient closely during treatment.
Ensure that a physician is in attendance during the first 15 minutes of the initial drug dosing.
If an HSR occurs, stop the drug. Maintain an IV line for emergency drugs and stay with the patient.
If a localized HSR occurs:
Monitor and evaluate symptoms (urticaria, localized erythema, wheals).
Administer diphenhydramine, corticosteroids, or both in accordance with the physician’s order.
Monitor vital signs every 15 minutes for the first hour.
Avoid using the drug; if the clinician wants to use it again, the patient should be premedicated with anti-histamines, corticosteroids, or both.
If the reaction is an anthracycline flare, stop the drug and flush the vein with saline. If the flare reaction resolves, continue the infusion slowly. Monitor for repeated flare reactions; it may be necessary to change the infusion site if this happens.
If a generalized HSR occurs (usually within the first 15 minutes of the drug infusion):
Stay with the patient; reassure the patient and family.
Discontinue the infusion immediately.
Maintain an IV infusion of normal saline solution.
Administer emergency drugs as ordered.
Maintain a patent airway and be ready to give cardiopulmonary resuscitation if necessary.
Notify the physician.
Monitor vital signs as needed.
Document the occurrence, the measures undertaken, and the patient’s responses.
Tell the patient to inform the clinician, on subsequent dosing, about the history of HSRs and measures undertaken that were effective.
If the clinician deems it necessary to use the drug again, the following precautions should be undertaken:
Physician-guided desensitization
Premedication with antihistamines, corticosteroids, or both
A longer infusion time
Increased volume of the solution used for dilution
Substitution of a similar drug, such as Erwinia L-asparaginase instead of the Escherichia coli form (Weiss, 1992).
Extravasation is the accidental infiltration of chemotherapeutic drugs into subcutaneous tissues. An unfortunate side effect of chemotherapy administration, it is not unusual in cancer patients because their thin, fragile, and mobile veins have experienced multiple punctures. The degree of extravasation varies from mild erythema to severe tissue damage with involvement of deeper structures such as tendons and joints (Fig. 6-1).
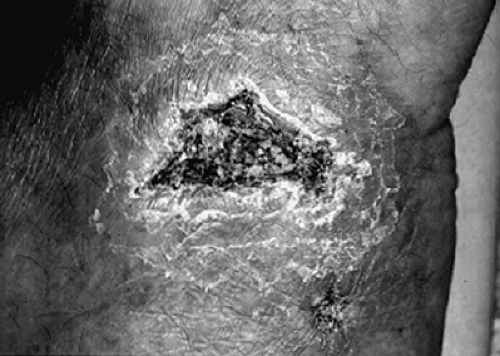 Fig. 6-1. Progressive necrosis and ulceration noted in an extravasation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|