The presence of nodal metastases is the most important prognostic indicator in breast cancer, making accurate assessment of the axillary nodal basin critical to delivering optimal therapy in breast cancer. Clinically node-negative women can be reliably staged in a minimally invasive manner using sentinel lymph node dissection (SLND). In node-negative patients receiving neoadjuvant chemotherapy, SLND can be performed after chemotherapy, allowing for a single surgical procedure and a decreased probability of requiring axillary lymph node dissection (ALND). Clinically node-positive patients are currently recommended to undergo ALND, although these recommendations may change with emerging trial data.
Key points
- •
Accurate staging of the axillary lymph nodes is critical to defining prognosis and for planning therapy.
- •
In patients with clinically negative axillary lymph nodes, sentinel lymph node dissection (SLND) is the standard approach to surgically staging the axillary nodes and has been shown to be technically feasible and accurate in multi-institutional randomized studies.
- •
The ACOSOG Z0011 trial demonstrated that carefully selected clinically node-negative women undergoing breast conservation therapy who have 1 or 2 positive sentinel lymph nodes may safely omit axillary lymph node dissection (ALND) without impact on oncologic outcomes.
- •
SLND can be performed successfully after neoadjuvant chemotherapy in clinically node-negative patients and allows for a single surgical procedure for patients as well as a lower proportion of patients requiring ALND.
- •
ALND remains the standard approach for clinically node-positive patients who undergo neoadjuvant chemotherapy. Emerging data from trials such as the ACOSOG Z1071 study may soon change this practice.
Introduction
The presence of axillary lymph node metastases is the most significant predictor of cancer outcomes in breast cancer, and remains an important aspect of diagnosis and management of these patients. Nodal status is often the key determinant of extent of surgery as well as systemic therapy and radiation. In the past, women diagnosed with breast cancer underwent axillary lymph node dissection (ALND) in order to stage the axilla. The introduction of sentinel lymph node dissection (SLND) as a validated staging procedure allowed clinicians to gain the same information while minimizing morbidity with no difference in oncologic outcomes. Although all patients with positive lymph nodes underwent ALND in the past, recent data have changed this approach, and have allowed for highly selected women to omit ALND. Emerging data will potentially broaden this approach in growing populations of patients. Therefore, surgeons must be able to accurately assess the axillary nodes for the presence of metastases, delineate the extent of nodal disease, and understand the impact on oncologic outcomes in order to design operations that are effective but also minimize morbidity.
Introduction
The presence of axillary lymph node metastases is the most significant predictor of cancer outcomes in breast cancer, and remains an important aspect of diagnosis and management of these patients. Nodal status is often the key determinant of extent of surgery as well as systemic therapy and radiation. In the past, women diagnosed with breast cancer underwent axillary lymph node dissection (ALND) in order to stage the axilla. The introduction of sentinel lymph node dissection (SLND) as a validated staging procedure allowed clinicians to gain the same information while minimizing morbidity with no difference in oncologic outcomes. Although all patients with positive lymph nodes underwent ALND in the past, recent data have changed this approach, and have allowed for highly selected women to omit ALND. Emerging data will potentially broaden this approach in growing populations of patients. Therefore, surgeons must be able to accurately assess the axillary nodes for the presence of metastases, delineate the extent of nodal disease, and understand the impact on oncologic outcomes in order to design operations that are effective but also minimize morbidity.
Staging of axillary nodal region
Physical examination of breast cancer patients should always include specific attention to the regional nodal basins such as the axillary, infraclavicular, and supraclavicular regions. When axillary adenopathy is noted, clinicians should record the size of the palpable lymph node as well as whether the nodes feel matted together. Unfortunately, physical examination is not sensitive or specific, as involved nodes may not be palpable, and palpable nodes may actually be reactive, especially after breast biopsies. The false-negative rate for physical examination is as high as 45% in some series. For this reason, clinical examination is complemented by nodal ultrasonography. Axillary lymph nodes can be assessed for features associated with malignancy such as enlarged size, thickened or eccentric cortex, or compression of the fatty hilum. Suspicious nodes routinely undergo fine needle aspiration (FNA) or core biopsy to provide pathologic confirmation of involvement with a subsequent sensitivity of 86% to 89% and specificity as high as 100%. This information can then be used in designing a treatment plan.
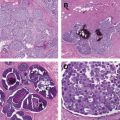
The American Join Committee on Cancer (AJCC) staging classification has different parameters for nodal staging based on clinical versus pathologic evaluation. Clinically identified axillary lymph nodes (either by examination or imaging studies) are designated as N1 if they are in the ipsilateral nodal basin and are mobile, or N2 if they are fixed or matted to each other or other structures. Contralateral axillary metastases are classified as distant metastases. The pathologic staging system has more variation. Metastases that are less than or equal to 0.2 mm are classified as isolated tumor cells and are designated at pN0(i+). Metastases in 1 to 3 axillary lymph nodes are categorized as N1, with a designation of “mi” if the metastases are micrometastases (>0.2 mm but ≤2 mm). Involvement of 4 to 9 axillary lymph nodes is staged as pN2, and at least 10 involved nodes are defined as pN3.
Clinically node-negative patient
SLND Technique
SLND is based on the concept that the breast has an orderly pattern of lymphatic drainage, with specific lymph nodes, or sentinel nodes, that drain the breast first, followed by drainage to the remaining nodal basin. This idea was first reported by Braithwaite over 100 years ago after observing the lymphatic drainage pattern of a gangrenous appendix. The first clinical applications were presented in the 1970s for penile cancer, although the technique did not become widely used because of its difficulty. In the early 1990s, a more feasible technique was created for melanoma that allowed for widespread implementation into practice. Before this point, women standardly underwent ALND for staging of axillary nodes, with the associated morbidities of the procedure including functional deficits, chronic pain, and development of lymphedema. Unfortunately, many of these patients had no nodal metastases and thus suffered the morbidities without an oncologic benefit. Thus there was tremendous interest in applying the technique to breast cancer patients. SLND was quickly validated as an accurate technique for staging nodal basins in breast cancer patients with increased sensitivity and decreased risks.
In clinically node-negative patients who undergoing surgery as the first component of their breast cancer treatment, SLND is the standard surgical approach to axillary staging. Multiple studies have demonstrated that an SLN can be identified in 93% to 99% of patients, with a false-negative rate (ie, number of patients with axillary metastases in which no cancer is seen in the SLN) of 5% to 11%. If the SLN is negative for metastases, then no further axillary surgery is required, and the remaining lymph nodes can be left in place.
Sentinel Node-Positive Patients
With the development of SLND, pathologists began to perform more detailed evaluation, because fewer lymph nodes were removed, leading to increased sensitivity and a growing population of women identified with micrometastatic (<0.2 mm) or low-volume nodal metastases. Although the American Society of Clinical Oncology and the National Comprehensive Cancer Network guidelines recommended completion of ALND for any patient with a positive SLN, regardless of size, many clinicians questioned this paradigm, pointing to data that only 20% of patients with micrometastases and 12% of those with isolated tumor cells (ITCs) had additional positive non-SLNs. An analysis of the Surveillance, Epidemiology, and End Results (SEER) data from 1998 to 2004 showed that 16% of SLN-positive patients did not undergo completion ALND. This proportion rose to 38% in those with micrometastases. A similar study of national patterns using the National Cancer Data Base (NCDB) showed that 20.8% of patients with a positive SLN between 1998 and 2005 did not undergo ALND. There were no differences in the incidence of axillary recurrence or in overall survival (OS) between patients who underwent ALND compared with those who did not, although selection bias must be considered in these retrospective accounts. However, these studies showed that clinicians believed that ALND could be omitted in select SLN-positive patients, although there were no prospective data to support this.
Several phase 3, multicenter trials have been reported in the last 5 years designed to answer this question; all have slight variations in trial design and eligibility criteria. The American College of Surgeons Oncology Group (ACOSOG) Z0011 trial was a multi-institutional, prospective trial with a noninferiority design. It enrolled clinically node-negative patients with T1 or T2 tumors who were treated with breast conservation therapy (BCT) and adjuvant radiotherapy who were found to have 1 or 2 positive SLN on standard pathologic examination with hematoxylin and eosin (H&E) staining. Patients were randomized to completion ALND versus SLN alone and followed for evidence of disease recurrence and for overall survival. After opening in 1999 with a planned accrual of 1900 patients, the trial closed early in 2004 with 891 enrolled patients secondary to slow accrual and a low event rate. In an intent-to-treat analysis, there were 420 patients in the ALND arm and 436 in the SLND alone arm, with similar clinicopathologic features between the 2 groups. At median follow-up of 6.3 years, local recurrence was seen in 3.6% of the ALND group versus 1.8% of the SLND alone group ( P = .11). Axillary recurrences were also similar between the 2 groups (0.5% in ALND cohort vs 0.9% in ALND alone, P = .45). There were no differences in 5-year overall survival (91.9% in ALND vs 92.5% in SLND alone, P = .24) or disease-free survival (82.2% vs 83.8%, P = .13). The investigators concluded that ALND could be safely omitted in clinically node-negative patients with T1 or T2 tumors undergoing BCT with 1 or 2 positive lymph nodes. Twenty-seven percent of the ALND group was found to have metastases in non-SLN. Of the patients with micrometastases in the SLN, only 10% had additional positive non-SLN. The study design in depicted in Fig. 1 .
A similar European trial, the EORTC 10981-22023 AMAROS (After Mapping of the Axilla, Radiotherapy or Surgery?) trial was also a multi-institutional trial enrolling clinically node-negative patients with T1 or T2 tumors with a positive SLN. In contrast to the ACOSOG Z0011 trial, patients were randomized to ALND or axillary radiotherapy (the Z0011 trial did not allow third field nodal irradiation). The results were reported at the 2013 American Society of Clinical Oncology (ASCO) Annual meeting describing 744 subjects in the ALND arm and 681 in the axillary radiation arm. At median 6.1 years follow-up, the axillary recurrence rates were 0.54% (4 cases of 744) in the ALND group and 1.03% (7 of 681) in the axillary radiation group. In comparison, they also followed 3131 patients with a negative SLN and found an axillary recurrence rate of 0.8%. There were no statistical differences in 5-year overall survival (93.3% ALND vs 92.5% axillary radiation, P = .3386) or disease-free survival (86.9% ALND vs 82.7% axillary radiation, P = .1788).
Finally, the IBCSG 23-01 trial corroborates the findings that patients with small-volume nodal disease do not need completion ALND. This phase 3 noninferiority trial randomized clinically node-negative patients with T1 or T2 tumors who had only micrometastases identified in SLNs. Unlike the Z0011 trial, subjects could undergo mastectomy or BCT and could have any number of positive SLNs as long as all metastases were no more than 2 mm (micrometastases were seen in 37.5% of the ALND cohort and 44.8% of the SLND cohort in the Z0011 trial). Radiation fields were not defined in the trial design so patients had heterogeneous radiation administration. Only 9% of patients in each group underwent mastectomy; none received adjuvant radiation. In the remaining 91% of patients who underwent BCT, 19% of both groups received intraoperative radiotherapy alone, and 70% received standard adjuvant whole breast radiation therapy (WBRT). Nine percent of the ALND group and 8% of the no ALND group received a combination of intraoperative and WBRT, while 2% to 3% of the groups did not receive adjuvant WBRT. Locoregional recurrences were seen in 2.4% (11 of 464) of the ALND group versus 2.8% (13 of 467) of patients without ALND. Five-year disease-free survival was 84.4% in the ALND cohort compared with 87.8% in the group without ALND ( P = .16). Once again, the authors concluded that patients with nodal disease limited to micrometastases might safely omit ALND without compromising oncologic outcomes.
These trials have been widely discussed in the breast cancer community and have led to a change in practice patterns in the United States. Investigators from MD Anderson Cancer Center reviewed the practice patterns in patients meeting the Z0011 inclusion criteria treated in the year before the release of the Z0011 results compared with those treated the year after an institutional multidisciplinary meeting discussing the results. Before Z011, 85% (53 of 62) of SLN-positive patients underwent ALND compared with 24% (10 of 42) treated after Z0011. In addition, surgeons were less likely to perform intraoperative nodal assessment after Z0011 (26% vs 69%, P <.001) and had a decrease in mean operative time to 79 minutes compared with 92 minutes before Z0011 ( P <.001), representing possible cost-saving results. The potential for cost savings was estimated by 1 group to be a 64% reduction in in-patient hospital stays and an 18% reduction in perioperative costs when Z0011 criteria were applied to SLN-positive patients undergoing BCT. On the national scale, a survey of 849 American Society of Breast Surgeons members reported that 57% would not routinely perform ALND in sentinel node-positive patients meeting the Z0011 criteria.
Management of Isolated Tumor Cells
As pathologic analysis of SLNs has evolved, the addition of immunohistochemical (IHC) staining has allowed for characterization of isolated tumor cells (ITCs), defined as clusters of cells no more than 0.2 mm, single tumor cells, or clusters of less than 200 cells in a single cross-section. The discovery of these occult metastases that were previously unrecognized when only standard H&E evaluation was performed left clinicians wondering what, if any, effect this extremely small amount of metastasis has on clinical outcomes. The ACOSOG Z0010 trial was a prospective observation trial enrolling women who underwent BCT who had a negative SLND by routine H&E staining. IHC staining was then performed on the SLN blocks at a central laboratory with the treating clinicians blinded to the results (thus they treated all patients based on the negative H&E result). Of 3326 specimens reported to be negative by H&E staining, 10.5% (349) had metastases identified by IHC. Five-year OS was similar between IHC-negative (95.7%) and IHC-positive (95.1%) patients ( P = .64), validating the practice of treating these patients as node negative. Additionally, in a subgroup analysis of the NSABP B-32 trial, occult metastases were identified by IHC in 15.9% of patients with negative H&E results. Similar to the Z0010 trial, treating clinicians were blinded to the IHC results and thus considered the patients node negative when making therapeutic decisions. In contrast to the ACOSOG Z0010 trial, they did show a small, but statistically significant difference in 5-year OS (94.6% in the IHC-positive patients compared with 95.8% in IHC-negative patients, P = .03). However, the authors concluded that an absolute survival difference of 1.2% did not warrant a change in adjuvant therapy based on the IHC results alone.
The exception to this may be patients with tumors with lobular histology. Lobular cancer cells grow in noncohesive patterns, and are more likely to be seen as widely dispersed isolated tumor cells in lymph nodes. Not only are patients with lobular tumors more likely to have ITCs, they are also more likely to have additional positive lymph nodes when ITCs are identified. In a study from MD Anderson Cancer Center, 17% of patients with lobular tumors had additional positive lymph nodes when ITCs were seen in the SLN. Based on these data, many surgeons still recommend ALND when ITCs are seen in patients with lobular tumors.
Timing of SLND in Patients Undergoing Neoadjuvant Chemotherapy
Neoadjuvant chemotherapy (NCT) is increasingly used in breast cancer patients with the benefits of allowing for in situ assessment of tumor response, as well as downsizing the tumor, which may facilitate breast conservation therapy. Another benefit of NCT is that 40% to 75% of patients presenting with clinically involved lymph nodes will convert to pathologic lymph node negative. Thus, SLND can lead to different results (and resulting adjuvant therapies) depending on whether it is performed before or after NCT. Some clinicians have advocated for upfront SLND before initiating chemotherapy, arguing that SLN identification is more successful before chemotherapy and the knowledge of nodal status is important to treatment planning. However, this approach commits all women, even if the SLN is negative, to 2 surgical procedures. It also commits women with small-volume nodal disease that would have been easily eradicated with chemotherapy to ALND. Data from MD Anderson Cancer institution have demonstrated that the SLN identification rate is not altered by NCT (98.7% if surgery first vs 97.4% if SLN was performed after NCT) with similar false-negative rates (4.1% in surgery first cohort vs 5.8% in NCT). After stratification for tumor size, the number of positive SLNs was lower if performed after NCT as opposed to before chemotherapy, which resulted in fewer ALNDs. In addition to sparing patients, performing SLND after NCT prioritizes the nodal status after NCT, which is a better prognostic indicator than the identification of occult nodal metastases before NCT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree