Table 33.1 Clinical aspects of male infertility
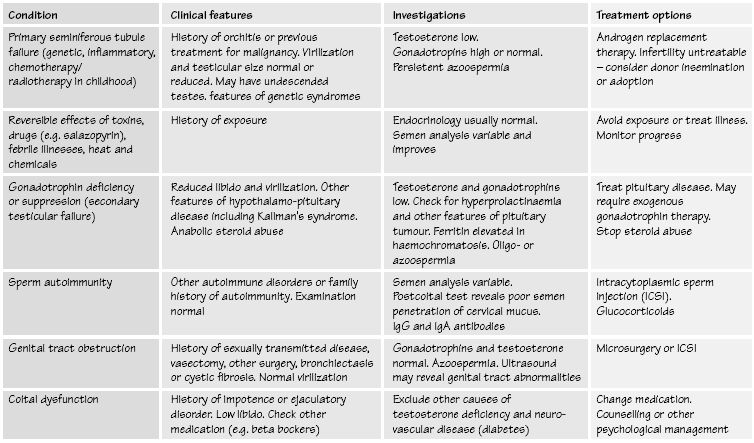
(adapted from Baker HWG. Management of male infertility. Ballieres Clinical Endocrinology and Metabolism 2000; 14(3): 409–422)
Male infertility has a large number of causes, both endocrine and non-endocrine in origin and few are specifically treatable. In the majority of cases an exact diagnosis is not reached despite investigation and the condition may result from previous testicular damage, varicocoele or non-specific inflammation. All patients should be assessed with their partner in a specialist fertility unit and in the undiagnosed group the use of intracytoplasmic sperm injection may offer the best chance of fertility. The clinical features of male infertility are shown in Table 33.1.
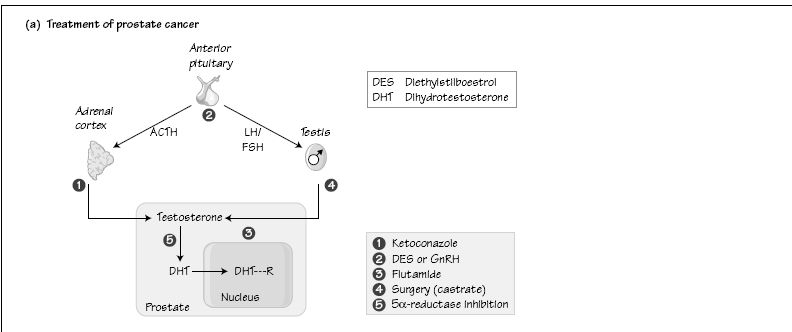
Male reproductive pathophysiology
Hypogonadism is the failure of the testes to function, that is to produce testosterone and spermatozoa, and can be due to genetic defects (see Chapter 23). Primary hypogonadism refers to abnormalities within the gonad, for example Leydig cell agenesis (non-development), or failure of Leydig cells in adult life. Leydig cell failure can occur after mumps. Secondary hypogonadism refers to gonadotrophin deficiency or failure to secrete gonadotrophin-releasing hormone (GnRH), and is also called hypogonadotrophic hypogonadism.
Hypergonadism means the excess activity of the gonad, which can be virilizing due to androgen-secreting Leydig cell tumours, or feminizing
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree