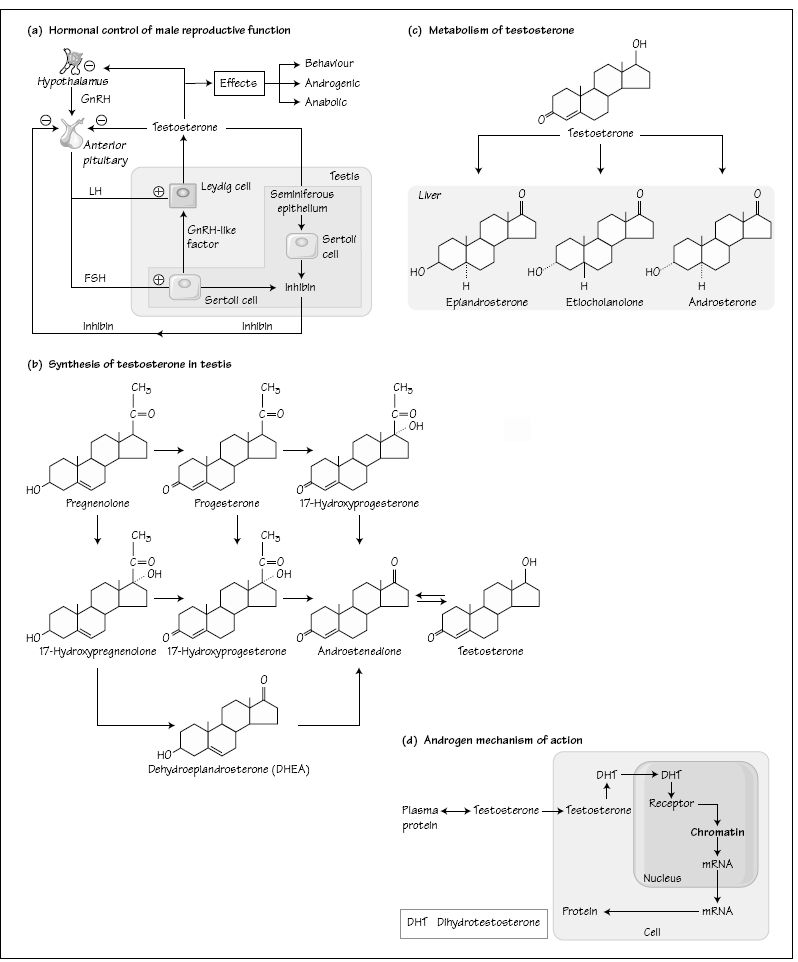
Normal fertility in the male is produced by a complex interaction between genetic, autocrine, paracrine and endocrine function. The endocrine control of reproductive function in the male depends upon an intact hypothalamo–pituitary–testicular axis. The testis has a dual role–the production of spermatozoa and the synthesis and secretion of testosterone needed for the development and maintenance of secondary sexual characteristics and essential for maintaining spermatogenesis. These functions in turn depend upon the pituitary gonadotrophin hormones: luteinizing hormone (LH; required to stimulate testicular Leydig cells to produce testosterone); and follicle stimulating hormone (FSH; required for the development of the immature testis and a possible role in adult spermatogenesis). Gonadotrophin production occurs in response to stimulation by hypothalamic GnRH. Testosterone exerts a negative feedback on the secretion of LH and FSH and the hormone inhibin-β, also synthesized by the testis, has a specific regulatory role for FSH. Thus in primary seminiferous tubular failure, low testosterone concentrations are associated with elevated gonadotrophins whereas in the presence of hypothalamic pituitary disease the gonadotrophin concentrations are low (secondary testicular failure).
Spermatogenesis is dependent upon testosterone availability. In primary seminiferous tubular failure androgen deficiency has a number of causes including: genetic defects in the Y chromosome and gonadotrophin receptor genes, previous testicular inflammation such as mumps orchitis and chemotherapy or radiotherapy for malignant disease. Patients exhibit signs of androgen deficiency and the azoospermia is associated with elevated gonadotrophin levels (hypergonadotrophic hypogonadism). Treatment requires androgen replacement therapy with assessment and management in a specialist fertility treatment centre.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree