The intermediate between random and regular network architecture explains the small-world phenomenon. As mentioned above: ‘C’ and ‘L’ are the two crucial measures for the classification of a network on the continuum of regular to random. Interestingly, small-world properties already occur when p is only slightly higher than 0: now ‘L’ drops sharply, but ‘C’ hardly changes (Fig. 21.2). This means that a regular network in which only a few connections are randomly rewired, suddenly combines high clustering with short path length, the small-world phenomenon. The combination of the parameters C and L makes it possible to define an index of ‘small-worldness’ [22]. All complex networks, varying from railway networks to the World Wide Web and from social to neural networks, show some degree of small-worldness.
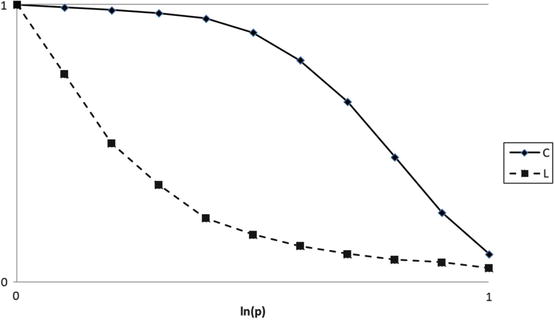
Fig. 21.2
Graph illustrating different types of networks according to graph theory. When p = 0, the network is completely regular with high C and high L. When p is only slightly higher than 0 (which is the case when only a few edges are randomly rewired), the path length L drops sharply, while C hardly changes. At the other end of the graph the network is completely random (p = 1, low C, low L)
In 28 healthy volunteers, the correlation between resting-state small-world network topology (measured with MEG) and cognitive performance was studied [23]. A higher ‘small-world index’, defined as the ratio between normalized clustering and path length, in the theta and lower gamma bands appeared to be related to a better cognitive performance. The clustering coefficient in the delta and theta bands was also positively correlated to global cognitive functioning. Moreover, the study showed that there was a gender difference in network topology: the female brain had a shorter average path length than the male brain, which indicates that the female brain has more efficient network architecture.
Modularity is another possibly relevant feature of the brain network; it quantifies to what extent a network can be optimally divided in internally correlated subnetworks or modules [24]. Furthermore, hubs are nodes crucial for information flow throughout the network. They can be defined in several ways, the simplest being determining which nodes have the highest number of connections. Conversely, the number of shortest paths passing a specific node reflects betweenness centrality as a measure of hubness. From a modularity viewpoint, connector hubs link different modules together, while provincial hubs only have high connectivity to nodes within their own module [25].
In an already mentioned study, we found significant differences in modularity between LGG patients and both healthy controls and HGG patients [19]. LGG patients displayed the most extensive modular disturbances, with more modular organization of their brain networks, and a decrease in integration between different modules, as compared to controls and HGG patients. But how do these alterations in the brain network relate to patients’ functional status?
21.6 Correlation Between Network Disturbances and Clinical Functioning in Low-Grade Glioma Patients
We investigated network topology in relation to cognitive functioning in low-grade glioma patients [26]. Our hypothesis was that changes in the functional brain network are the intermediate between the impact of the tumor and the anti-tumor and anti-epileptic treatment on the one hand (this could be defined as ‘input’), and cognitive performance (defined as ‘output’), on the other hand. Seventeen LGG patients were selected for participation in the study. The patients had shown no radiological or clinical signs of tumor progression during the previous 6 months. The mean time between diagnosis and this study was 8 years, with a range of one to 19 years. Seven patients had been treated with radiotherapy, and two patients had received prior chemotherapy (the combination of procarbazine, lomustine, and vincristine). Sixteen of 17 patients used anti-epileptic drugs (AEDs), and of these, six were free of seizures. We also included healthy controls (relatives of the participating patients or staff members of our hospital) to allow for comparisons. The patient group did not differ from the control group with respect to age, gender and educational level.
Cognitive performance was measured by an extensive standard testing battery, containing tests that reflect a wide variety of cognitive abilities, such as psychomotor function, executive (frontal) function, (selective) attention, mental processing speed, mental control, verbal learning, organization, memory, mental concentration, information processing and flexibility of verbal thought processes. It took between 60 and 120 min to complete this assessment. The data that were collected in this way were reduced to six cognitive domains (which are commonly used in neuropsychological research): (1) information processing speed, (2) psychomotor functioning, (3) attention, (4) verbal memory, (5) working memory, and (6) executive functioning.
We performed MEG recording during a no-task, eyes-closed resting-state (see Fig. 21.3). Magnetic field frequencies between 0, 5 and 80 Hz were recorded. From the entire recording of 10 min, four artifact-free samples of 13 s were selected by visual analysis. The SL was used as a measure of statistical interdependency between time series from all MEG sensors, and its values were calculated for every possible pairwise combination of MEG sensors for all frequency bands. MEG sensors were grouped according to their location in central, frontal, occipital, parietal, and temporal areas. Subsequently, three types of SL averages were calculated: (1) five interhemispheric between-area SLs, (2) eight (four per hemisphere) long-distance intrahemispheric SLs (frontotemporal, frontoparietal, parieto-occipital, and temporo-occipital), and (3) ten (five per hemisphere) within-area local SLs. The latter were a measure for short-distance connectivity, while the first two SL-types can be regarded as a measure for long-distance connectivity.
Fig. 21.3
(a, b) The MEG system as used in the department of Clinical Neurophysiology of the VU Medical Center
Regarding cognitive functioning, we found—as could be expected from the results of one of our previous studies [13]—that patients performed poorer than control subjects. This was the case for the overall measure of cognition as well as for psychomotor function, working memory, information processing speed, and attention. There were no significant differences for the domains of verbal memory and executive functioning. Regarding functional connectivity, long-distance functional connectivity was abnormally increased in the low frequencies in the patient group in comparison to the controls, corroborating our previous findings [11, 14]. Significantly decreased long-distance connectivity in patients was observed for intertemporal connectivity in the delta band and for interoccipital connectivity in the lower alpha band.
Obviously, the most important question was whether there was an association between cognitive performance and functional connectivity patterns. With regard to the previously mentioned disturbed cognitive domains, post-hoc regression analysis showed that increased long-distance and short-distance connectivity in the delta, theta and gamma bands was associated with decreased working memory, attentional functioning and information processing speed. It therefore seems clear that diminished cognitive performance is associated with pathologically increased connectivity, above all in the lower frequency bands (although the same was observed in the lower and upper gamma bands), for a number of long-distance connections. Again, it could be speculated that these changes indicate a compensatory mechanism in LGG patients: they might need an increase of synchronization in order to compensate for their diminished cognitive performance. However, this association may also indicate pathological ‘disinhibition’: local inhibitory connections are disrupted and this leads to slowing down and higher amplitude of oscillations and subsequently to increase of cortico-cortical connections. Anyhow, these findings strongly suggest that changes in resting-state connectivity are not simply an epiphenomenon, but may be relevant for the observed cognitive impairments in LGG patients, although the causal relation of the association remains unclear.
It must be stressed that the findings of this study regarding functional connectivity are not completely consistent with the findings of our earlier study [14], which is cited above. In that study we reported an increase in the low-frequency bands for the short-distance connections and a decrease in high-frequency bands for the long-distance connections. In that same study a decrease in the lower alpha band and an increase in the lower gamma band were found. It is—again—not clear how these conflicting results should be explained, but the different patient populations (LGG patients versus patients with a mixture of primary intracranial tumors) may lie at the root of these divergent findings.
Another study explored further details of network architecture and cognitive functioning in that same LGG patient group [27]. The PLI, which was also used in the aforementioned study [18], was used to generate connectivity matrices that could be converted into graphs. As mentioned before, the main advantage of the use of PLI in this type of research is that it is less sensitive to volume conduction than other parameters of functional connectivity and it therefore measures ‘true interactions’. Our hypothesis was that functional connectivity in LGG patients is diminished in comparison to healthy controls. Secondly, we expected to find a loss of small-world characteristics (by computing the clustering coefficient (C), the path length (L), and the ‘small-world-ness’ (S) which is based on the trade off between high local clustering and short path length) in the neural network of LGG patients, hypothetically combined with decreased cognitive performance.
Again, higher connectivity was present in the theta frequency band for short-distance connections and for interhemispheric connectivity. In the theta band, the clustering coefficient was significantly higher in the patient group than in the control group. In the beta band, the opposite was the case. Moreover, the patient group showed a loss of small-worldness compared to the control group.
In the delta and lower alpha bands, interactions between network characteristics and cognitive functioning (attentional tasks and executive functioning) were observed. In the delta band, a longer path length was associated with poorer executive and attentional functioning, whereas a higher degree correlation (which indicates to what extent the degree of a vertex is influenced by the degree of the vertices to which it is connected) was associated with better attentional functioning. In the lower alpha band, an interaction existed between network characteristics and verbal memory: increases in clustering coefficient and path length were associated with diminished verbal memory. Summarizing the results of this study, we showed that there was higher functional connectivity in the theta frequency band in LGG patients in comparison to controls and that there were differences in network organization. Moreover, these changes appeared to be associated with cognitive performance.
In the same vein, i.e. loss of overall integrity of the brain network being related to poorer cognitive functioning, we have also shown that increased modularity, i.e. possible disconnection between the modular subsystems of the brain, relates to poorer cognitive functioning in brain tumor patients [19]. Furthermore, using slightly different analysis methods, changes in functional connectivity within two resting-state modules were explored before and after resection in LGG patients, and related to changes in cognitive functioning [28] increased within the DMN and FPN after surgery. More importantly, these increases were related to better postoperative cognitive functioning in the domain of attention and executive functioning. Thus, tumor resection might normalize functional brain networks and improve patients’ clinical outcome with respect to cognition.
Summarizing these results, it appears obvious that network configuration and functional connectivity are related to cognitive performance in (low-grade) glioma patients, as we recently posited in a review article [29]. Both increased and decreased connectivity within the various frequency bands may be demonstrated in the same patient, and these findings may again differ for long-distance and short-distance connections. Possibly, these nuances inform us about the clinical status of the individual patients, and may be used for clinical purposes in the future.
21.7 Assessment of Functional Connectivity and Clinical Applications
The aforementioned studies were primarily aimed at the investigation of general network disruption by glioma. A more direct approach to the use of MEG in glioma neurosurgical practice is also possible [30]. In this study, MEG was preoperatively used to identify the sensorimotor cortex. The MEG results were superimposed onto a three-dimensional MRI. The term ‘magnetic source imaging’ was used for this technique and a total of 50 patients with a variety of intracranial tumors, all located in the central region were examined and operated upon. The authors were able to distinguish sensory evoked fields and motor evoked fields in all patients. Sensory evoked fields were monitored by applying tactile stimuli to the thumb, the index finger and the little finger on the side contralateral to the lesion. For the registration of motor evoked fields, patients were asked to perform repetitive tapping with the contralateral index finger. Subsequently, the calculated cortical fields were used for image fusion with MRI. The procedure in which preoperative MEG findings are used for the optimization of neurosurgery is referred to as ‘functional neuronavigation’. The main advantage of this procedure is that it allows preoperative assessment of the relation of the tumor with the sensorimotor cortex and thus makes it possible to predict the type of surgery needed in an individual case.
The quantitative comparison between preoperative magnetic source (MS) imaging and intraoperative sensory and motor mapping has been studied [31]. These authors found an MS imaging source localization accuracy of 12.5 mm and considered this to be “ … a reasonable starting point in the preoperative planning of surgical approaches, resection strategies, and treatment options”. MS imaging is considered as an aid to intra-operative cortical mapping in patients with intra-axial brain tumors.
An MEG-based approach to scope lesion localization with resting-state functional connectivity was used in 15 patients with unilateral lesions, one patient with bilateral lesions and 14 healthy control subjects [32]. Detailed analyses of connectivity were focused on the alpha frequency band. Significantly lower connectivity values were found in brain areas that were non-functional in comparison to contralateral tissue. This decrease was only observed in regions corresponding to a clinically functional deficit, rather than in the entire area of the tumor extension. These regions with diminished functional connectivity could reliably be resected. Moreover, patients in whom no connectivity deficit could be demonstrated or patients with increased connectivity in the tumor area suffered from transient or permanent neurological deficits after the resection. It is interesting to note that all patients, in comparison to control subjects, showed areas of scattered or diffuse decreased connectivity, but these were unrelated to tumor location, tumor volume or clinical deficits. This is in accordance with our own findings [11].
In a more recent study, this resting-state functional connectivity concept for use in clinical practice was further explored [33]. In 57 patients with a brain tumor near or within motor, sensory, or language areas, resting-state MEG recordings were performed. Functional connectivity was estimated by means of ‘imaginary coherence’. This is a measure that reduces the risk of overestimating the magnitude of connectivity as a consequence of crosstalk between voxels or common references. This method, like the PLI, makes use of the fact that phase similarities between time series that arise from a common reference or that result from volume conduction occur with zero time delay. The mean imaginary coherence between voxels in and around brain tumors, and the rest of the brain was compared to the mean imaginary coherence between contralateral voxels and the rest of the brain. A second comparison was made between the local cortical connectivity pattern in the tumor area and the results of intra-operative electrical stimulation. A very important finding of this study was that the cortical maps that were obtained with MEG showing decreased resting-state connectivity (this was the case in 7 out of 57 patients) had a negative predictive value of 100% for the absence of functioning eloquent cortex. On the other hand, if the functional connectivity in the tumor area was increased (which was the case in 42 out of 57 patients), a positive predictive value of 64% for the identification of language, motor or sensory cortex by means of intraoperative electrical stimulation was calculated. These results are encouraging and have stimulated further research on clinical applications of functional connectivity.
The potential clinical significance of these findings is obvious, but also limited at this point in time. Based on preoperative MEG findings, individual risk profiles may in the future be calculated before operation and this may have consequences for the planning of the surgical procedure, but this type of personalized medicine is not ready for the clinic yet. The extent of resection of low-grade gliomas still depends mainly on the results of intraoperative functional mapping, which includes also the stimulation of subcortical (white matter) structures [34, 35].
21.8 Epilepsy and Brain Networks in Low-Grade Gliomas
Epilepsy is the most common symptom in LGG patients and it accounts for a significant negative attribution to quality of life, especially when seizure freedom is not achieved with AEDs [12]. Tumor resection may contribute to seizure control; in a review on 773 patients from 20 studies, gross total tumor resection (compared to partial resection) appeared to be the variable that was most predictive of seizure freedom [36]. Another variable that indicated a favorable outcome in terms of seizure control was short duration of seizures (less than 1 year). The presence of medically refractory epilepsy before surgery, as well as the presence of simple partial seizures, was associated with poorer outcome. Consequences of these observations and the study described previously [3] are obvious: surgery should be aimed, whenever possible, at gross total resection, and operation should be performed as early as possible.
There is accumulating evidence that, apart from the ictal onset zone, the neural networks surrounding this zone and parts of the network even lying further remote are pivotal in the initiation, and particularly in the propagation of seizures [37, 38]. It is hypothesized that a loss of small-world network characteristics renders the brain more prone to seizures. Also, the presence of essential clusters of (pathological) connections in the network (‘hubs’) may play a role in the initiation and propagation of seizures [39]. The question then arises whether assessment of functional connectivity and neural network architecture with MEG may contribute to the planning of the surgical procedure of patients with LGG who also suffer from epilepsy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree