Fig. 13.1
(a) Lymph node groups in the neck. From Fialkowski EA, Moley JF. Current approaches to medullary thyroid carcinoma, sporadic, and familial. (b) Specimen from a patient following central and bilateral neck dissection. Level II nodes are from the high jugular nodes; level III, mid-jugular nodes; level IV, low jugular nodes; level V, posterior triangle nodes; level VI, paratracheal nodes; level VII, superior mediastinal nodes
Frequency of Node Involvement
In patients with thyroid cancer, lymph nodes in the central compartment (levels VI) are most often involved, followed by levels III and IV on the ipsilateral, and frequently the contralateral, side (Fig. 13.1). Involvement of levels II, V, and VII may also occur. Regional lymph node metastases are present in the majority of patients with palpable primary tumors. Ipsilateral neck dissection, also called “functional” or “modified radical” neck dissection, in which all or portions of levels II, III, IV, and V lymph nodes are removed, should be considered in patients suspected to have locally advanced disease based on clinical exam and imaging.
In most studies that have addressed the issue, the frequency of cervical lymph node metastases in papillary thyroid carcinoma has been reported to be high. Frazell and Foote reported that lymph node metastases were present in 71% of 385 patients with differentiated thyroid cancer [9]. Cody and Shah [13] reported that 22 of 23 patients with locally invasive well-differentiated papillary thyroid carcinoma were found to have metastatic disease in lymph nodes at the time of thyroidectomy and neck dissection. Mizuno and colleagues [14] found lymph node metastases in 89% of 71 patients with papillary thyroid carcinoma treated by thyroidectomy and routine neck dissection. They noted a high incidence of metastases to pretracheal and peritracheal lymph nodes. Sugino and colleagues [15] reported a series of 746 patients with papillary thyroid carcinoma treated by thyroidectomy and modified radical neck dissection. Though it is not possible to calculate the exact incidence of nodal metastases in this series from the data provided, they reported that lymph node metastases were more frequent in younger patients and that distant metastases were more common in older patients. Tisell [16] reported node metastases in 70% of men and 45% of women in his series of operations for papillary thyroid carcinoma (overall incidence of 51% of a total of 195 cases). It is clear, therefore, that lymph node metastases are extremely common in papillary thyroid carcinoma and that, if one routinely performs a lymph node dissection at the time of thyroidectomy for this disease, lymph node metastases will be found on pathological examination.
The pattern of metastatic spread in differentiated thyroid cancer is similar to that seen in medullary thyroid cancer (MTC) [5]. In patients with palpable unilateral intrathyroidal MTC tumors, we found lymph node metastases in 81% in central level VI, in 81% in ipsilateral levels II through V, and in 44% in contralateral levels II through V lymph node groups. In patients with bilateral intrathyroidal tumors, lymph node metastases were present in 78% of central level VI lymph node groups, in 71% of level II through level V lymph nodes ipsilateral to the largest intrathyroidal tumor, and in 49% of level II through level V lymph nodes contralateral to the largest intrathyroidal tumor. This is an alarmingly high incidence of lymph node involvement. In this same series, we found that intraoperative lymph node assessment by the surgeon had a low sensitivity (64%) and specificity (71%) for detecting positive lymph nodes. Therefore, reliance on intraoperative assessment will miss clinically involved lymph nodes up to one-third of the time. These findings can be applied to differentiated thyroid cancer, which spreads in the same manner. Small deposits of differentiated thyroid cancer, however, are effectively treated by radioactive iodine and thyroid hormone suppression; therefore, surgical removal of all nodal metastatic disease is not as important as in medullary thyroid cancer [8].
Prediction of Involvement of Adjacent Compartments
The burden of lymph node metastasis in the central compartment can help predict lateral compartment involvement. In one retrospective analysis of medullary thyroid cancer, the absence of positive central lymph nodes correlated with a 10% risk of metastatic involvement of ipsilateral level II to V lymph nodes. However, the risk of lateral compartment involvement increased to 77% with 1–3 positive central lymph nodes and to 98% with ≥4 positive central lymph nodes [17, 18]. Contralateral level II–V metastases were observed in 4.9% of cases when no central lymph nodes were positive, in 28% when 1–9 central lymph nodes were positive, and in 77% of cases when ≥10 central lymph nodes were positive. Therefore, the decision to perform lateral neck dissection can be influenced by the extent of central compartment lymph node involvement. If extensive central lymph node metastases are present, even with negative preoperative imaging, serious consideration should be given to performing an ipsilateral functional neck dissection given the high likelihood of lateral lymph node involvement.
Nomenclature of Operations
There are several names for systematic lymph node dissections described in patients with papillary thyroid carcinoma. The standard “radical” neck dissection includes removal of lymph nodes from levels II, III, IV, and V and sometimes level I en bloc with the sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve. In the past, this operation was performed in conjunction with thyroid lobectomy or subtotal thyroidectomy for differentiated thyroid cancer. Routine removal of paratracheal (level VI) and upper mediastinal nodes (level VII) was often not discussed. In a modified radical neck dissection, the lymph nodes are removed from levels II, III, IV, and V with sparing of muscle, vein, and accessory nerve. The term “functional neck dissection” generally refers to a modified radical neck dissection, but the nodal groups removed are specified. For example, occasionally surgeons do not remove level II or level V nodes during a lateral neck dissection, in which case, the operation could be specified as “functional neck dissection with removal of level III and level IV lymph nodes.”
Impact of Lymph Node Dissection on Outcome in PTC
Until recently, most studies have suggested that, although the presence of lymph node metastases in papillary thyroid carcinoma is associated with higher recurrence rates, their presence does not affect survival. Studies of survival in papillary thyroid carcinoma are difficult, because of the indolence of the tumor and because few patients die from the disease. Woolner et al. [19] reported only 18 deaths in 656 patients with papillary thyroid carcinoma who were followed for 40 years. Many studies have reported no influence of lymph node metastases on outcome in patients with papillary thyroid carcinoma. Mazzaferri et al. [20] reported that, although recurrences were more frequent in patients with lymph node metastases, patient survival was not adversely affected. In his study of 576 patients with papillary thyroid carcinoma, there were no statistically significant differences in recurrence or death comparing patients who underwent simple excision of palpable cervical node metastases with those who had systematic modified radical or radical neck dissection for excision of nodal metastases. Samaan and colleagues [21] compared 340 patients with apparent gland-confined differentiated thyroid carcinoma to 333 patients with lymph node metastases and found no difference in survival. These results were verified by numerous other studies. McHenry and colleagues [22], however, noted higher recurrence rates in patients with lymph node metastases from papillary thyroid carcinoma and recommended routine cervical lymph node sampling with modified radical neck dissection in patients with metastatic carcinoma evident on frozen section. Other authors have advocated a routine aggressive “microdissection” or “compartment dissection” in patients with papillary thyroid carcinoma. Tisell and colleagues, [23] using an approach similar to the microdissection they applied to reoperation for MTC, reported 195 patients treated for papillary thyroid carcinoma. Dissection of the central compartment with excision of pretracheal and paratracheal lymph nodes was routinely performed, and lateral dissection, with removal of levels II, III, IV, and IV nodes, was performed in 25 patients because macroscopically positive lateral nodes were identified. The average operative time was 3.9 h. Radioiodine therapy was given to only seven patients, three because of pulmonary metastases and four because of locally invasive stage III tumors. Only three (1.6%) patients died of thyroid cancer, all of whom had survived for more than 17 years after surgery. One patient (0.5%) had a permanent recurrent nerve injury, and six patients (3.1%) had permanent hypoparathyroidism. These are excellent results and compare favorably with survival rates from other reported series. In Mazzaferri’s series, the 10-year mortality following operation for thyroid carcinoma was 0.6% after total thyroidectomy, 1.5% after subtotal thyroidectomy, 1.7% after simple excision of lymph node metastases, and 0.7% after neck dissection. In many other reported series, it is difficult to extrapolate disease-specific mortality rates as a function of the operative procedure performed. In a retrospective series from Japan, Mizuno and coworkers [14] described the routine performance of bilateral cervical lymph node dissection for non-advanced papillary thyroid carcinoma in 71 patients. In an additional 33 patients, sternotomy with mediastinal dissection was performed. The authors found pretracheal and tracheoesophageal lymph node metastases in 51% of the former group and in 48% of the latter. They concluded that such operations would prevent the morbidity of central recurrence with airway or vascular invasion. Scheumann and colleagues [24] reported their experience with routine compartment-oriented node dissection for papillary thyroid carcinoma. They reviewed their institution’s experience with this disease and found a significant correlation between lymph node status and recurrence and survival. Their approach in all patients with papillary thyroid carcinoma is to perform a systematic total thyroidectomy and compartment-oriented microdissection of the central neck (levels VI and VII). In patients with macroscopically involved lateral or mediastinal nodes, lateral dissection or median sternotomy with mediastinal node dissection is performed. The authors reported an improvement in recurrence and survival rates, though statistical validation of this conclusion was not provided. In an invited commentary of that study, Blake Cady indicated that the experience of the authors was at odds with almost all recent reports in the world’s literature which indicated no influence of lymph node metastases on outcome of surgery for differentiated thyroid carcinoma. He also stated that the findings may be explained by the fact that these patients come from an iodine-deficient area, in which thyroid cancers are known to be more aggressive. Our group has shown that even for patients with persistent cervical lymph node disease after surgery, as seen on posttreatment radioactive iodine scanning, postoperative radioactive iodine therapy results in very high disease-free survival rates [8].
Prophylactic Central Neck Dissection in Differentiated Thyroid Cancer
Surgery, radioactive iodine, and thyroid hormone suppression are the mainstays of treatment for thyroid cancer. Due to the lack of prospective randomized trials, many of the current guidelines for treatment of well-differentiated thyroid carcinoma remain controversial, including the extent of surgery and management of cervical lymph nodes. The central neck lymph node compartment is defined as tissue between the carotid arteries extending from the vascular pedicle superiorly to the sternal notch and subclavian artery inferiorly [5, 12, 25, 26]. These nodes have been found to frequently harbor metastases. The current National Cancer Comprehensive Network (NCCN) guidelines suggest that if cervical lymph nodes in well-differentiated thyroid cancer are clinically negative for disease, prophylactic central neck dissection can be considered but is not required [27]. Current American Thyroid Association (ATA) guidelines state “prophylactic central compartment neck dissection (ipsilateral or bilateral) may be performed in patients with papillary thyroid carcinoma with clinically uninvolved central lymph nodes, especially for advanced primary tumors (T3 or T4)” [26]. This is a grade C recommendation of expert opinion, and currently no randomized data is available to support that central node dissection impacts survival or recurrence rates in differentiated thyroid cancer. At a recent NIH meeting of thyroid cancer specialists, an informal poll of surgeons indicated that half of those present performed prophylactic central neck dissection routinely, while half did not.
Proponents of prophylactic central node dissection argue that the procedure may decrease recurrence and mortality rates, improves the accuracy of staging, decreases postoperative thyroglobulin levels, and may avoid reoperative surgery [24, 28–30]. Thyroglobulin levels were shown to be improved in patients treated with routine prophylactic central neck dissection [31]. The reported recurrence rates range up to 34% of patients, and among patients with local recurrence, 8% eventually die of thyroid cancer; with distant metastases, 50% die of thyroid cancer. They argue that removing the central neck lymph nodes provides data upon which to base decisions regarding whether or not to treat with radioactive iodine and removes potential sites of recurrence that may require reoperations that have higher complication rates [31].
Several retrospective studies, however, have shown that the presence of central lymph node metastases has little impact on predicting recurrence or survival. A recent meta-analysis of retrospective studies concluded that the addition of a central node dissection to total thyroidectomy has no effect on locoregional recurrence [32, 33]. Also, thyroglobulin levels are unreliable indicators of disease status after treatment and may continue to decline for years after therapy [34, 35]. Our group has shown that even for patients with persistent cervical lymph node disease after surgery, as seen on post treatment radioactive iodine scanning, postoperative radioactive iodine therapy results in very high disease free survival rates [8]. These data argue against the utility of exposing patients to additional surgical prophylactic procedures. Based upon data from randomized clinical trials, prophylactic lymph node dissection has been abandoned in breast cancer [36, 37] and malignant melanoma [38].
Published Guidelines for Treatment of Thyroid Cancer
Guidelines have been developed, published, and updated for most commonly treated cancers including thyroid cancer. The most widely used and cited guidelines for thyroid cancer are those published by the NCCN and the ATA [26, 27]. Published guidelines from high-level professional and government-supported organizations are an increasingly important source of information and guidance for clinicians treating thyroid and other cancer. These guidelines also summarize the current state of knowledge and point out deficiencies in data used to guide clinical decisions. The content of published guidelines is based upon data from published studies that have been vetted and discussed by experts who then compose the text of the guidelines. Current NCCN and ATA guidelines are vague regarding the routine use of prophylactic central neck dissection in early-stage thyroid cancer, because there are no data from prospective clinical trials. The guidelines suggest that the procedure be “considered” or “may be performed.”
Technique of Neck Dissection for Thyroid Carcinoma
Preoperative Workup
If the patient is hoarse or if it is a large tumor, awake laryngoscopy should be done to observe cord motion and document abnormalities. If the patient has a vocal cord palsy on one side, special care must be taken with the functioning nerve, because bilateral palsies (even transient ones) often require tracheostomy. Tracheostomy in a patient after a thyroidectomy and central neck dissection is especially dangerous because the tube is adjacent to the innominate artery with no intervening central fat, nodes, and thymus to protect the artery. Innominate blowout may occur. If the patient has a vocal cord palsy on one side, consideration should be given to leaving tissue to cover the innominate artery or to do a unilateral procedure, in which the functioning nerve is not manipulated.
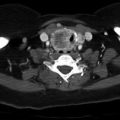
CT of the neck and chest should be done if there is evidence of significant cervical nodal involvement [39]. The presence of distant metastatic disease may influence the surgeon’s choice of operation. If distant metastatic disease is detected, removal of the entire thyroid and all disease in the cervical nodes should be done to allow for optimal antitumor effectiveness of radioactive iodine.
Most surgeons in North America rely heavily on preoperative ultrasound imaging to map the extent of lymph node involvement and determine the extent of surgery based on imaging results [40]. Ultrasound with marking of involved lymph nodes should be performed preoperatively. Lymph nodes with metastatic thyroid cancer may have an abnormal appearance, including abnormal overall morphology, loss of fatty hilum, and calcifications. The involved lymph nodes may be marked on the overlying skin, and the surgeon should review the ultrasound (or perform it himself or herself, if able) with the radiologist to be familiar with the findings. A permanent marker should be used and care taken not to wash the marks off in the process of sterile prepping.
Central Neck Dissection
Positioning and Incision
In the operating room, after the induction of general endotracheal anesthesia (which may be done with a nerve-monitoring tube), the patient is placed in a mild relax or “beach-chair” position with the head in mild hyperextension and the arms placed on the lower abdomen with the hands on the anterior superior iliac spines or pubis. This requires pulling the draw sheet around the patient and fastening it together in the midline, creating a “papoose” (Fig. 13.2). Foam padding is placed around the arms to protect from nerve compression. This positioning is necessary because if the arms are tucked at the patient’s sides, there may be too much stretch on the brachial plexus, which can cause temporary or permanent numbness and weakness of the hands and arms.
Fig. 13.2
Standard positioning for thyroidectomy, neck dissection
The patient is prepped from the chin to upper chest and draped. The incision is made in a low collar position, ideally overlying the thyroid isthmus, using a preexisting skin crease if one is available (Fig. 13.3). Generally, this operation can be done with a 5–8 cm low collar incision or smaller, if the surgeon is experienced. If a lateral dissection is anticipated, a longer incision should be made, and the incision may be carried up along the posterior border of the sternocleidomastoid muscle. Alternatively, a cosmetically superior approach for lateral dissection is a laddered second incision made in a preexisting skin crease superior and lateral to the low collar incision.
Fig. 13.3
(a) Preoperative ultrasound-guided markings of metastatic PTC. (b) Same patient 2 weeks post-op showing healed laddered incisions in skin creases (MacFee incision)
Initial Dissection
Subplatysmal flaps are created in the standard fashion and a self-retaining retractor placed. The strap muscles are then divided in the midline, and on the side of the thyroid tumor, the sternohyoid muscle is separated from the sternothyroid muscle. On the side of the tumor, the sternothyroid muscle is left attached to the underlying thyroid (to provide an additional margin), and the superior and inferior attachments of this muscle are divided (at the thyroid cartilage and the sternum).
Thyroidectomy and Tumor Specimen Mobilization
Superior pole vessels are divided after mobilization medial to lateral to avoid injury to the superior laryngeal nerve which may be visualized during this process. Once the superior pole is taken down, the thyroid is rolled medially and anteriorly. At this point, the procedure departs from what is done in a standard thyroidectomy. The objective is to sweep up the thyroid lobe with surrounding soft tissue and nodal tissue, leaving only the recurrent nerve behind (Fig. 13.4). Attempts may be made to preserve the blood supply to the upper parathyroid, but I usually remove both ipsilateral parathyroids with the specimen and then dissect them out of the specimen if possible, mince them into 1 × 1 mm fragments, and transplant them into individual muscle pockets. Because I am not attempting to preserve the parathyroid blood supply on the side of the tumor, I divide the tissue on the anterior surface of the carotid artery and sweep everything medially. This requires less dissection and fewer vessels to control, but one must be able to identify and transplant the normal parathyroids.
Fig. 13.4
Left and right views of thyroidectomy/central neck dissection after mobilization of the specimen. Upper parathyroids are preserved. Lower parathyroids are removed and autotransplanted. Right RLN is partially encased by tumor. Patient’s head is to the right
Dissection is carried out on the anterior surface of the carotid artery. If one stays directly on the anterior surface of the carotid, the dissection is quite safe, because the only structures one will encounter are the middle thyroid veins coming off the internal jugular vein, which should be divided. Inferiorly, as the carotid becomes the innominate, the surgeon encounters the thymic horns and associated veins overlying the trachea, which must be divided and swept into the specimen. On the right, the dissection is done to the level of the innominate artery, and on the left the dissection is done to the level of the clavicle, at a point equivalent to the innominate takeoff on the right [41]. Once the central compartment contents are thus mobilized, including the thyroid, parathyroids, central neck nodes, fat, and thymus, dissection is carried out superior to inferior. I find this easiest if done with the (right-handed) surgeon on the left side, using the right hand to perform dissection from above and to cross toward the midline along the innominate artery. The thyroid is mobilized from top down, leaving the sternothyroid muscle attached. In the process, the recurrent laryngeal nerve is identified and preserved, and the upper and lower parathyroids are identified. Soft tissue and vascular attachments to the thyroid are divided, including middle veins and inferior thyroid artery and veins. The nodal packet is swept up off of the recurrent laryngeal nerve and the esophagus to the trachea. It is dissected off of the trachea, leaving only the bare trachea, esophagus, and recurrent nerve centrally (Fig. 13.4). Inferiorly the specimen is swept off of the recurrent laryngeal nerve to the trachea, and the thymic horns are divided with the nodal packet at the level of the innominate artery. Importantly, it is also necessary to mobilize and remove the nodes that reside in the hollow behind the right recurrent laryngeal nerve.
Contralateral Thyroidectomy and Node Dissection
Once the tumor side is completely mobilized, attention is turned to the contralateral side. If this side has no tumor involvement, both sternothyroid and sternohyoid strap muscles may be mobilized off of the thyroid lobe and reflected laterally. The undersurface of the inner strap muscle is carefully cleaned off so that all fat, nodal tissue, and the thymus are incorporated in the specimen. Again the thyroid superior pole is mobilized and the carotid artery is dissected on its anterior surface inferiorly, and the central compartment containing the thyroid, parthyroids, nodes, and thymus is exposed. If the surgeon prefers to preserve the parathyroids on this side, then a standard parathyroid-preserving thyroid lobectomy should be carried out, leaving the upper parathyroid on an intact vascular pedicle and the lower parathyroid on an intact pedicle in the thyro-thymic ligament. Tissue medial and anterior to the thyro-thymic ligament may be swept medially with the thyroid to join the contralateral dissection. The inferior extent of this packet is transected with cautery or a hemostatic device such as the harmonic scalpel, with care to ligate large veins. The entire packet including the thyroid and central neck contents is then oriented with sutures and submitted to pathology, after carefully removing any parathyroids from the tumor-bearing side of the specimen for autotransplantation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree