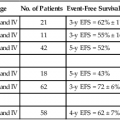
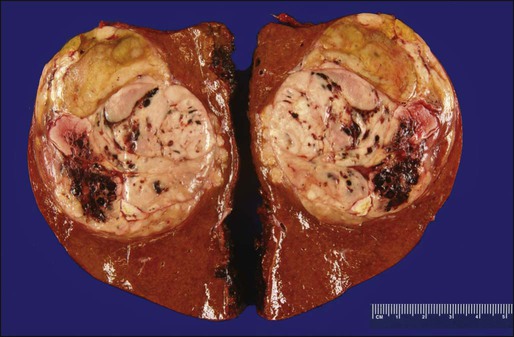
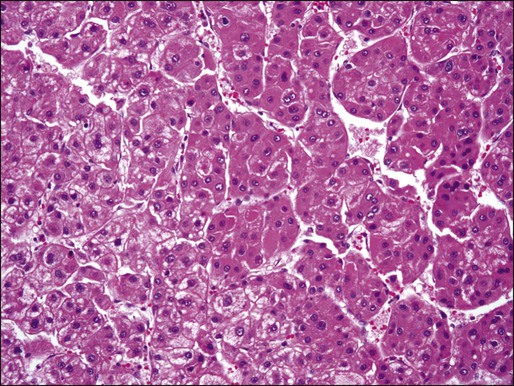
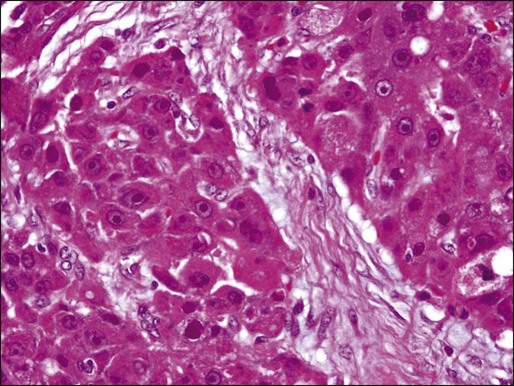
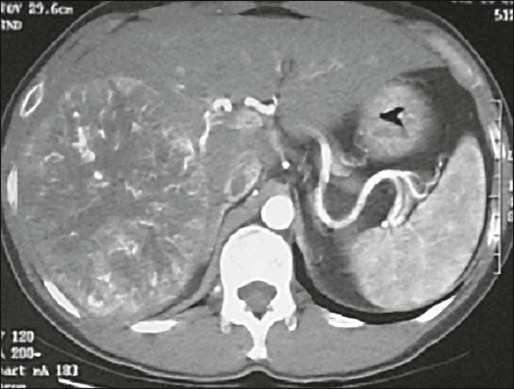
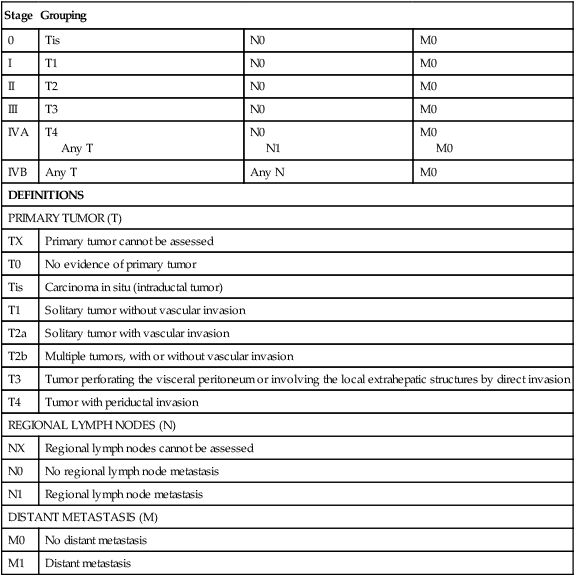
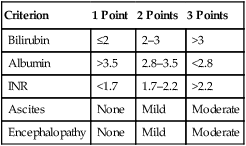
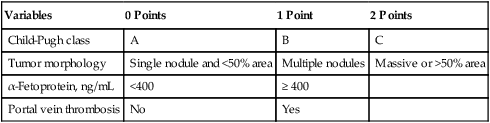
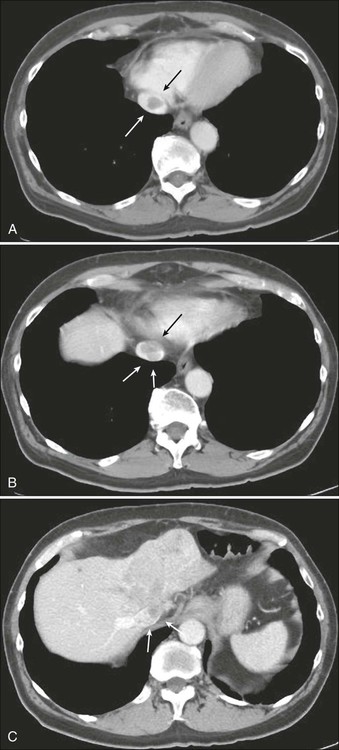
80 Ghassan K. Abou-Alfa, William Jarnagin, Maeve Lowery, Michael D’Angelica, Karen Brown, Emmy Ludwig, Anne Covey, Nancy Kemeny, Karyn A. Goodman, Jinru Shia and Eileen M. O’Reilly • There is a continued rise of hepatocellular carcinoma (HCC) incidence especially in the Western hemisphere. • HCC main risk factors are hepatitis B, hepatitis C, alcohol, and nonalcoholic steatohepatitis. • Screening programs continue to evolve, but depend mainly on ultrasound and α-fetoprotein (AFP) evaluations. • Staging of HCC depends on evaluating the two aspects of the disease: the cancer itself, and the commonly associated cirrhosis. • Pathology evaluation may help distinguish variants or combined HCC and cholangiocarcinoma. • Patterns of spread are hematogenous, and may involve lung and bones. • Surgery, liver transplantation, and radiofrequency ablation (RFA), are the sole proven curative therapies for HCC. • Locally advanced disease is generally treated with different forms of local therapies, including but not limited to, transarterial chemoembolization, bland embolization, radioembolization, and radiation therapy. • Sorafenib is the sole drug approved for the treatment of advanced HCC, based on an improvement in survival compared with placebo. • Future developments are likely to be dependent on the evaluation of combination therapies and/or the development of new targets. • Future studies are most likely to entail enriched patient populations based on biology, risk factors, and/or etiology. • The majority of biliary tumors are adenocarcinomas. • Despite their similarities, biliary tumors are now better understood as three different diseases: gallbladder cancer, extrahepatic, and intrahepatic biliary tumors, with different clinical and biological characteristics. • Gallbladder resection may require resection of segments IVA and V of the liver plus a locoregional lymph node dissection for better tumor control and staging. • Preoperative considerations for extrahepatic biliary tumors include percutaneous transhepatic biliary drainage. • Surgical therapy for distal extrahepatic cholangiocarcinoma is a pancreaticoduodenectomy, as for all periampullary malignancies. • No adjuvant therapy has been proven effective for biliary tumors. • The standard of care for advanced disease consists of gemcitabine plus cisplatin based on the ABC-02 study. HCC is the sixth most common malignancy in the world, and is responsible for 600,000 deaths annually.1 Approximately 82% of cases arise in developing countries, with 55% in China alone, caused by hepatitis B virus (HBV). Transmission of HBV occurs both vertically and horizontally. In the United States, HCC incidence and mortality continues to rise. According to the American Cancer Society and the Surveillance, Epidemiology and End Results (SEER) database, 28,720 new diagnoses of primary liver cancer and intrahepatic cholangiocarcinoma, and 20,550 deaths from these diseases were expected to occur in 2012.2 Southern European countries in the Mediterranean basin have a high incidence of HCC mainly due to hepatitis C virus (HCV) and alcohol use.1 Egypt represents a particular and very concerning example where HCC incidence continues to increase exponentially and is a leading cause of cancer morbidity and mortality.3 Egypt has one of the highest prevalences of HCV in the world, ranging between 6% and 40% in different regions. This is partly the result of a national treatment program against schistosomiasis, another known risk factor for HCC, in which the use of nondisposable needles potentially served as a conduit for transmission and a continuing epidemic.4 Worldwide, HCC is more common among men than women, with a ratio that ranges from 1.5 : 1 to 11 : 1. The male-to-female ratio is further increased in high-risk areas.5 This disparity is a consequence of the differential effects of androgens and estrogens on hepatocytes.6 Temporal age variations are also noted, reflecting different patterns of exposure to etiologic factors. In high-risk areas, the age-specific incidence rates begin to increase after the age of 20 years, reflecting the importance of vertical transmission of HBV or acquisition of HBV infection in early childhood, and stabilizes at age 50 years and older.5 In low-risk areas, the incidence rate steadily increases with age, reflecting the later acquisition of viral infection or the impact of other factors, such as alcohol-related cirrhosis. Fibrolamellar carcinoma, which is considered a variant of HCC, is an extremely rare disease, comprising less than 1% of all primary liver cancers. Fibrolamellar carcinoma-HCC occurs equally in younger individuals, with a median age of 27 years, with a slight preponderance in women and without any underlying liver disease. It also tends to occur more frequently in whites.7 Viral hepatitides, mainly HBV and HCV, are the leading risk factors for HCC in Asian and Western populations, respectively. HBV is a DNA virus that can disrupt key regulatory oncogenes of the host genome by insertional mutagenesis. Chronic inflammation because of the host immune response may also destabilize the genome, permitting the accumulation of transforming mutations leading to HCC.9 In the case of HCV, a RNA virus, hepatocarcinogenesis is driven by oxidative DNA damage and inflammation, which gives rise to cirrhosis and, eventually, HCC, in a process that may take 10 to 30 years to develop in 5% of those patients who were infected with HCV at some point.10 Morbid obesity, diabetes mellitus, and resultant nonalcoholic steatohepatitis are all independent risk factors for hepatocarcinogenesis.12 The metabolic syndrome is associated with peripheral insulin resistance and upregulation of the insulin/insulin-like growth factor–1 receptor (IGF1IGF–1R).13 Hereditary hemochromatosis is a common hereditary metabolic disorder in Northern European countries with a 20- to 220-fold higher risk of developing HCC.14 Other metabolic disorders associated with the development of HCC include α1-antitrypsin deficiency,15 plus several others. Aflatoxin, produced by the Aspergillus fungus that contaminates grain product,16 is a recognized risk factor for developing HCC in sub-Saharan Africa, and southeast Asia. Carcinogenesis occurs as a result of p53 tumor suppressor mutations as a consequence of the transversion of glycine (G) to threonine (T) at codon 249.17,18 Betel quid consumption is a popular practice in several Asian countries. The major carcinogenic ingredient in betel quid is the arecoline alkaloid.19 Mouse models have shown that toxicity occurs through immunosuppression, structural hepatocyte injury, and suppression of antioxidants. Contaminated water in parts of rural China with microcystins, a blue-green algal hepatotoxin, can cause HCC by increased oxidative DNA damage20 and induction of apoptosis by increasing expression of p53 and Bax while suppressing expression of Bcl-2.21 Measurement of serum α-fetoprotein (AFP) is the most widely employed screening test for HCC in an at-risk population.22 One prospective study in an HBV carriers’ population randomized 5581 men to undergo either AFP testing every 6 months or no screening.23 Overall survival was not different between the screened and unscreened populations. On the other hand, in a larger trial, 18,816 patients with HBV were randomized to screening with serum AFP levels and liver ultrasonography biannually compared to no screening. Among individuals assigned to the screening arm, HCC mortality was reduced by 37%.24 AFP screening continues to be a subject of debate, although most physicians elect to continue using it in practice. The role of other serologic tests such as assays for des-γ-carboxy prothrombin, Lens culinaris agglutinin-reactive fraction (AFP-L3), and insulin-like growth factor–1 (IGF1) remains unclear.25 Adjunctive screening with ultrasonography on an every 6 month basis also is recommended by published guidelines.22 The sensitivity and specificity of screening ultrasound in high-risk patients are 71% and 93%, respectively.26 Ultrasound examination is cheap and safe but has low sensitivity for detection of small nodules, and its usefulness in this regard is particularly operator-dependent. Newer techniques, such as helical computed tomography (CT) and contrast-enhanced magnetic resonance imaging (MRI), including the newer gadoxetate acid-enhanced MRI, remain unclear in regard to any impact on mortality rates in at-risk populations.27 And, of course, the issue of cost and affordability are critical in defining early detection strategies. HCC is a malignant neoplasm derived from the hepatocytes. Grossly, HCCs associated with liver cirrhosis often present as expansile tumors with a fibrous capsule and intratumoral septa; in contrast, tumors arising in noncirrhotic livers tend to grow to massive size and may be nonencapsulated (Fig. 80-1). All HCCs have a strong propensity for invasion of vascular channels, and large vein invasion may be seen grossly. Histologically, HCCs assume a wide spectrum of morphologic alterations (Fig. 80-2). Well-differentiated HCCs recapitulate the cellular and architectural characteristics of benign hepatocytes to such extent that a histologic diagnosis of malignancy can be a challenge, especially in small biopsy samples. On the other hand, poorly differentiated tumors may lose almost all histologic hallmarks of hepatocytes. A variety of histologic patterns have been described, including trabecular, acinar, solid, and scirrhous. The prognostic significance of these patterns, however, is yet to be determined. Approximately 5% of all primary liver tumors are combined hepatocellular-cholangiocarcinoma.6,8 The WHO defines such tumors as having unequivocal, intimately mixed elements of both HCC and cholangiocarcinoma. The hepatic component is defined by the presence of bile production, bile canaliculi, and a trabecular pattern of growth. The glandular component is defined by the presence of true gland formation. A distinctive clinicopathological variant of HCC is the fibrolamellar carcinoma, which occurs in young adults and has no association with cirrhosis or other known risk factors. This variant tends to present as well circumscribed, nodular, yellow-to-brown tumors with extensive fibrosis grossly. Some tumors may present with a “central scar.” Histologically, this variant is characterized by the presence of dense bands of lamellar fibrous tissue separating the tumor cells that are typically polygonal and exhibit large nuclei with prominent nucleoli (Fig. 80-3). Immunohistochemical studies may aid in the diagnosis of hepatocellular neoplasms. Characteristic hepatocellular markers include the hepatocyte antibody, also known as HepPar-1, glypican-3, an oncofetal protein elevated in the sera of many patients with HCC, polyclonal carcinoembryonic antigen (CEA) and CD10, which both label hepatocytes in a canalicular pattern, and AFP. Fibrolamellar carcinomas tend to express CK7 and epithelial membrane antigen, two markers that are typically not expressed in conventional HCC, which can help to differentiate between fibrolamellar carcinoma and HCC.28 HCC characteristically invades the portal vein and its branches, and vascular invasion is the main route for intrahepatic tumor spread. Tumor invasion into the major bile ducts is infrequent clinically, but may be seen histologically. Intraorgan spread of HCC is considered under the T category, not M, in the American Joint Committee on Cancer (AJCC) TNM staging system.29 Extrahepatic tumor spread is common, and is mainly via hematogenous dissemination and targets the lung most commonly, followed by bone and other sites such as the adrenal glands.30 In recent years, bone metastases from HCC have increased in incidence.31 In a retrospective evaluation over 5 years at Memorial Sloan-Kettering Cancer Center, almost 10% of HCC patients were found to have bone metastases at presentation (unpublished data). This increasing potential for metastatic disease is mainly explained by the improved survival of HCC patients across the board. It is thus imperative that patients with HCC receive appropriate staging that includes a whole body radiologic evaluation including the chest. Bone scans should be done in case of symptoms or suspicious radiologic or laboratory findings. Lymph node metastasis is more commonly seen in fibrolamellar carcinoma. In a recent retrospective analysis of 95 cases of fibrolamellar carcinoma from three institutions, lymph node metastases were present in 50% of the cases.32 Although a majority of patients present with locoregional disease, many patients present initially with stage IV disease or develop metastases at a later time. Recurrences after surgery are either intrahepatic or extrahepatic, with the most common sites of extrahepatic metastasis being lung, retroperitoneal lymph nodes, and bone. Clinical manifestations may include malaise, anorexia, abdominal pain, abdominal fullness because of ascites or mass effect, or weight loss. Acute abdominal pain and distention caused by the spontaneous rupture of a superficial tumor with resulting hemoperitoneum is a common presentation of HCC in high-prevalence areas.33 This potentially fatal event is a medical emergency that warrants early recognition and management. All patients with suspected HCC also should undergo hepatitis serologic studies, including testing for hepatitis B surface antigen, hepatitis B core antibody, and hepatitis C antibody. Where applicable, a polymerase chain reaction quantitative assay should be performed. Depending on the degree of underlying liver damage from fibrosis, results on liver function testing and the prothrombin time may be abnormal. An assessment of liver function should be performed; the most commonly used assessment with the most widespread availability is the Child-Pugh score. Although there are guidelines to help diagnose HCC using imaging and AFP levels, these are applicable for screening and surveillance situations.34–37 Their application, of course, will depend on a faithful application of the criteria, which include a diagnosis of cirrhosis (which remains ill defined). Newer technology may help improve the noninvasive diagnosis of HCC. Gadoxetate disodium is a new gadolinium-based contrast agent indicated for intravenous use in T1-weighted MRI of the liver to detect and characterize lesions in adults with known or suspected focal liver disease.38 Cholangiocarcinoma is commonly identified in what was thought to be HCC.39,40 In the setting of advanced disease, and especially if systemic therapy is considered, a biopsy is very valuable. As described in the pathology section, diagnosis of HCC may include variants, as well as possible combined cholangiocarcinoma plus HCC, the treatment of which will differ from that of HCC. Translational research using tissue specimens have been pivotal in the elucidation of key signaling pathways that may be targeted with novel therapies. Liver biopsy is a comparatively safe and well-tolerated procedure. Although it is true that it carries a risk of bleeding and tumor seeding, these complications are rare with hemorrhage reported in 0.4% of cases and tumor seeding in 1.6% of cases.41,42 Dynamic CT has replaced ultrasonography in assessing HCC. In the early phase, the tumor is hyperdense because of its increased vascularity (Fig. 80-4). In the later phase, the tumor is hypodense, as a result of washout of contrast from the more “porous” lesion. On MRI, HCC is of low signal intensity on T1-weighted images and of intermediate signal intensity on T2-weighted images. Because of the propensity of this tumor for extension into and along major vessels, contrast-enhanced triple-phase CT or MRI is particularly useful for imaging the portal and hepatic veins. In addition, contrast-enhanced images provide critical information about multifocality, resectability, and presence of extrahepatic disease. Although positron emission tomography using fluorine 18-labeled fluorodeoxyglucose (18FDG) has been found to be useful to image a variety of tumors, its use in HCC has yielded disappointing results, with significantly lower standardized uptake values for HCC compared with metastatic tumors or other primary liver tumors.42 The seventh edition of the AJCC staging classification uses size, presence of vascular invasion, lymph node status, and metastatic disease as prognosticators of outcome (Table 80-1). The main features of this revised system included a separate staging systems for HCC and intrahepatic cholangiocarcinoma, a split of the T3 category to reflect the different prognoses of large multifocal lesions versus the presence of macrovascular invasion, a redefined the N1 category, and a classification of lymph node metastases as stage IV disease.29 Table 80-1 American Joint Commission on Cancer Staging System for Hepatocellular Carcinoma Including Intrahepatic Bile Ducts: Tumor-Node-Metastasis (TNM) Classification From Edge SB, Byrd DR, Compton CC, et al., editors. AJCC cancer staging manual. 7th ed. New York: Springer; 2010. The prognosis of HCC depends not only on an anatomic assessment of the tumor, but also on the extent of underlying liver cirrhosis. The Child-Pugh scoring system remains the most commonly used tool for assessing cirrhosis.45–45 It remains the most common scoring system used in HCC clinical trials. It consists of five parameters: serum bilirubin, serum albumin, prothrombin time, clinical ascites, and clinical encephalopathy. The severity of each parameter is graded from 1 to 3 (Table 80-2), and the total make up the score that is defined as A to C. Table 80-2 Modified Child-Pugh Classification for Assessing Degree of Liver Impairment INR, International normalized ratio. From Child CG, editor. The liver and portal hypertension. Philadelphia: Saunders; 1964. p. 50. The limitations of both the TNM and Child-Pugh systems was first overcome by the Okuda staging system,46 which includes parameters related to the cirrhosis and factors related to the cancer itself. The Okuda scoring system was considered by many as unsatisfactory and several scoring systems followed, many of which were prospectively validated. These include, but are not limited to, the Cancer of the Liver Italian Program (CLIP),47 the Chinese University Prognostic Index (CUPI) scoring system,48 the Groupe d’Etude et de Traitement du Carcinoma Hepatocellulaire (GETCH) staging system,49 the Japan Integrated Staging (JIS),50 and the Barcelona Clinic Liver Cancer (BCLC) classification system.51 The BCLC couples prognosis with treatment assignment; however, it has been found to be less valuable in the setting of more advanced disease, defined as BCLC category C.52,53 It was found that the CLIP (Table 80-3), CUPI, and GETCH scoring systems were the most informative regarding the outcome of this specific patient population, while the BCLC classification system had limited discriminatory abilities in this population, and its use is not recommended for patients with advanced disease. Table 80-3 Cancer of the Liver Italian Program (CLIP) Scoring System From the Cancer of the Liver Italian Program (CLIP) Investigators. Prospective validation of the CLIP score: a new prognostic system for patients with cirrhosis and hepatocellular carcinoma. Hepatology 2000;31:840-845. In patients with limited disease and no underlying liver parenchymal disease, the outcome after resection can be reasonably good. The operation can be performed with an operative mortality rate of less than 5% in high volume centers, and 5-year survival may exceed 30%.54–58 This subgroup represents, however, a small minority of all patients with HCC, as the vast majority have at least some degree of underlying liver disease or frank cirrhosis. The adverse influence of cirrhosis on surgical outcome is well documented, with very high perioperative mortality rates, up to 10% in some series from high-volume centers.55–59 From the same series, cirrhotic patients who survive the operation may enjoy a reasonable 5-year survival rate, approximately 30%. Recent series, albeit small, have shown further improvements in outcome, with perioperative mortality of at least 1.4% and 5-year survival rate of 77%.60,61 These patients are at very high risk, not only for recurrent disease, but also the development of new sites of malignancy in the diseased liver remnant and deterioration of liver function resulting in hepatic failure. Indeed, the presence or extent of cirrhosis has been shown to be an independent predictor of reduced survival.58,60 Thus, when assessing patients for surgery, careful evaluation of the hepatic functional reserve is equally as important as the disease extent and feasibility of a complete resection. The single most reliable method of assessing hepatic function is the Child-Pugh classification (see Table 80-2),44,45 which remains the most useful and most widely used in Western series, although the indocyanine green retention rate commonly is used in Asia. A more sensitive assessment of hepatic function is the hepatic vein wedge pressure, a technique that may be particularly useful for identifying patients with Child-Pugh A cirrhosis with occult portal hypertension.62 The invasive nature and special radiologic expertise required for this study have limited its use. Most surgeons will consider resection only for patients with Child-Pugh A cirrhosis and in selected patients in the Child-Pugh B category; with major resections only considered in the former group. Few surgeons are willing to perform hepatic resection for patients with Child-Pugh C, considering a high operative mortality rate of 30%. Nonetheless, some studies have reported reasonable long-term survival even when a larger tumor size required extended hepatectomy, rather than more limited resection.63,64 In general, though, these patients are better served with transplantation if they meet accepted criteria. HCC has a great propensity for vascular extension, and the presence of tumor thrombus within the main portal vein or vena cava (E-Figure 80-1 and Fig. 80-5) is an ominous sign that, in general, is a contraindication to resection because of the very high risk of occult disseminated disease. Liver resections accompanied by portal venous tumor thrombectomies are unlikely to yield long-term survival. Multiple lesions do not necessarily preclude surgical resection or ablation (or both).55,57,65 Five-year survival rates can still be expected to be between 20% and 30%.55,57 Nonetheless, the presence of multiple tumors is associated with reduced survival after resection compared to resection of solitary tumors.60 Furthermore, tumor size is a well-known predictor of disease recurrence and survival.58,66 One strategy that may improve outcome after resection is preoperative portal vein embolization. This technique involves occlusion of the portal vein supplying the portion of the liver targeted for resection, typically the right hemiliver. This procedure results in atrophy of the liver to be resected and hypertrophy of the future liver remnant, and theoretically should result in a lower risk of postoperative liver failure. Indeed, a recent prospective study demonstrated the usefulness of preoperative portal vein embolization in patients undergoing resection of HCC, with significant reductions in postoperative liver failure, overall morbidity, and hospital length of stay.67 The “Milan criteria” have become the standard guidelines for hepatic transplantation in patients with hepatic cirrhosis: single tumor less than 5 cm in size or no more than 3 tumors all less than 3 cm in diameter, after transplantation demonstrated an actuarial 4-year survival rate of 75%.68 This report refocused attention on liver transplantation for HCC, which was verified in several subsequent reports.69 Using these criteria, several series have found excellent 5-year survival rates of 70% or greater, with a 15% chance for recurrence.61,70–73
Liver and Bile Duct Cancer
Liver Cancer
Epidemiology
Viral Hepatitis
Metabolic Disorders
Environmental Exposures
Prevention and Early Detection
Pathology and Pathways of Spread
Clinical Manifestations, Patient Evaluation, and Staging
Clinical Manifestations
Patient Evaluation
Staging
Stage
Grouping
0
Tis
N0
M0
I
T1
N0
M0
II
T2
N0
M0
III
T3
N0
M0
IVA
T4
Any T
N0
N1
M0
M0
IVB
Any T
Any N
M0
DEFINITIONS
PRIMARY TUMOR (T)
TX
Primary tumor cannot be assessed
T0
No evidence of primary tumor
Tis
Carcinoma in situ (intraductal tumor)
T1
Solitary tumor without vascular invasion
T2a
Solitary tumor with vascular invasion
T2b
Multiple tumors, with or without vascular invasion
T3
Tumor perforating the visceral peritoneum or involving the local extrahepatic structures by direct invasion
T4
Tumor with periductal invasion
REGIONAL LYMPH NODES (N)
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
N1
Regional lymph node metastasis
DISTANT METASTASIS (M)
M0
No distant metastasis
M1
Distant metastasis
Criterion
1 Point
2 Points
3 Points
Bilirubin
≤2
2–3
>3
Albumin
>3.5
2.8–3.5
<2.8
INR
<1.7
1.7–2.2
>2.2
Ascites
None
Mild
Moderate
Encephalopathy
None
Mild
Moderate
Variables
0 Points
1 Point
2 Points
Child-Pugh class
A
B
C
Tumor morphology
Single nodule and <50% area
Multiple nodules
Massive or >50% area
α-Fetoprotein, ng/mL
<400
≥ 400
Portal vein thrombosis
No
Yes
Primary Treatment and Adjuvant Therapy
Primary Therapy
Resection
Partial Hepatectomy

Total Hepatectomy and Transplantation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Liver and Bile Duct Cancer