Liposarcoma is one of the most common sarcoma subtypes with a heterogeneous biology and clinical behavior. This article gives a comprehensive overview on clinically relevant aspects of pathology and imaging. Prognostic factors and treatment strategies are discussed for different clinical situations and histologic subtypes. This information will be of value to clinicians and interdisciplinary sarcoma teams.
Key points
- •
Liposarcoma (LPS) is a heterogeneous disease with distinct subentities presenting with differential clinical behavior.
- •
From a clinical perspective, grading of liposarcomas is of greatest importance for decision making in localized tumors, as it greatly determines prognosis and aggressiveness of local treatment.
- •
Patients suspected of LPS should be managed by a multidisciplinary team with expertise in treating sarcomas.
- •
For the treatment of locally advanced liposarcomas, several neoadjuvant or definitive treatment modalities can be used to achieve local tumor control.
- •
Although important oncogenic events in well-differentiated and dedifferentiated LPS (MDM2/CDK4 amplifications) have been known for many years, targeted approaches have been hampered by the lack of drugs for clinical use. Recently, a multitude of compounds targeting CDK4 and MDM2 have entered clinical development and may soon change the landscape of systemic treatment for LPS.
Introduction
Liposarcomas (LPSs) represent one of the most common soft tissue sarcoma subtypes. In the National Cancer Institute’s Surveillance, Epidemiology, and End Results study, LPSs account for approximately 12.8% of all sarcomas. LPSs represent 24% of all extremity and 45% of all retroperitoneal soft tissue sarcomas and the annual incidence is estimated to be 2.5 per 1 million inhabitants in population-based studies.
LPS is defined as a malignant mesenchymal neoplasm that is composed of lipogenic tissue with a varying degree of cellular atypia, possibly including nonlipogenic sarcoma cells.
However, LPS is a heterogeneous disease with distinct subentities presenting with differential clinical behavior. LPS can be subdivided into 4 important histologic subtypes:
- •
well-differentiated LPS (WDLPS)/atypical lipomatous tumor (ALT; 40%–45% of all LPS)
- •
dedifferentiated LPS (DDLPS) (5% respectively of all LPS)
- •
myxoid LPS (MLPS)/round-cell LPS (RCLPS) (30%–35% of all LPS)
- •
pleomorphic LPS (PLPS) (<15% of all LPS)
From a conceptual standpoint, WDLPS and DDLPS should be grouped together, as DDLPS usually arises from WDLPS. Exact classification of the LPS subtypes is crucial for decision making in patients, as the aggressiveness of local and systemic treatment modalities may vary substantially ( Table 1 ).
| Subtype | Pathology | Molecular Characteristics/“Actionable” Targets | MRI/CT Appearance |
|---|---|---|---|
| ALT/WDLPS | Low grade, positive IHC for MDM2, CDK4, p16 | MDM2 and CDK4 amplifications | Large encapsulated lipomatous mass (high signal intensity both in T1-weighted and T2-weighted MRI) with thick internal septations; Signal loss on fat-saturated T1-weighted images, and focal nodules (>1 cm is suggestive of a DDLPS) |
| DDLPS | High grade, positive IHC for MDM2, CDK4, p16 | MDM2 and CDK4 amplifications | |
| MLPS and RCLPS | Low grade (percentage of round cells important for grading) | FUS-CHOP fusion gene, PI3K mutations (∼20%) | Pathognomonically low signal intensity in T1-weighted and marked signal intensity in T2-weighted MRI |
| PLPS | High grade, pleomorphic, cellular sarcoma | Complex structural rearrangements | Nonspecific soft tissue mass, often including areas of necrosis and hemorrhage |
Pathology and Molecular Pathology
In differentiated LPS, the lipogenic origin can typically be seen with lipoblasts paired with atypical stromal cells in the context of mature fat. With increasing dedifferentiation, LPSs develop greater similarity to other pleomorphic high-grade sarcomas, such as undifferentiated pleomorphic sarcomas, and may not even display adipocytic components. Benign lipomas, in contrast, consist only of mature adipocytes and usually occur subcutaneously, whereas LPSs are generally deep seated. Given this anatomic difference and the underlying biology, LPS and lipoma are classified as 2 distinct entities with an independent evolution.
From a clinical perspective, grading of LPSs is of greatest importance for decision making in localized tumors, as it greatly determines prognosis and aggressiveness of local treatment. WDLPS and pure MLPS are considered low grade. These tumors have very little to no metastatic potential and their prognosis is mostly favorable: 11% of all patients with WDLPS and MLPS die of their disease. DDLPS, RCLPS, and PLPS usually are classified as high-grade tumors with a disease-related mortality of 28% for DDLPS, 21% for myxoid-round cell, and 35% to 50% for PLPS. Histologic subtype plays a prominent role in MLPS, as these are highly sensitive to radiotherapy and often substantially shrink to neoadjuvant treatment.
WDLPS/DDLPS
The most common subtype of LPS is WDLPS. According to the most recent World Health Organization classification, ALT has replaced the term of WDLPS, as these tumors show no potential for metastases unless they undergo dedifferentiation. Biologically, ALT and WDLPS are the same, but tumors are named differently for patient reassurance: ALT should be used for resectable well-differentiated LPSs of the extremities, as local relapse is usually manageable and the term is more reflective of the benign course of disease. In contrast, WDLPSs in the retroperitoneum or mediastinum are biologically the same as ALT, but wide margins are difficult to achieve, and patients are more likely to die of local relapse. Karyotypically, WDLPSs are characterized by giant marker and ring chromosomes. This neochromosome contains an amplification of genes regularly based on chromosome 12q13–15. This set of genes includes oncogenes, such as MDM2 and CDK4. Nearly all WDLPSs and DDLPSs overexpress MDM2 and CDK4, making it the most important marker to differentiate from lipomas or other high-grade sarcomas. DDLPSs have been defined as “ALT that shows progression in a tumor with variable histologic grade.” Both, MDM2 and CDK4 have recently been identified as relevant therapeutic targets in LPS. Biologically, WDLPS and DDLPS represent a continuum, they share the same underlying genetic alterations and clinical features are similar. However, DDLPSs tend to grow more aggressively and are mostly found in the retroperitoneum.
MLPS/RCLPS
The second most common subtype is MLPS/RCLPS (20% of all LPSs), which more often occurs in younger patients. MLPS is even the most common LPS in children and adolescents. High histologic grade is often defined as greater than 5% round-cell component and low grade is usually associated with a metastatic risk of less than 10%. As MLPS progresses, more round-cell components can be found, either as isolated nodules or transitional areas with mixed cell types. Genetically, MLPS/RCLPS is characterized by a reciprocal translocation of chromosomes 12 and 16;t(12;16)(q13; p11), which can be found in approximately 95% of all cases. This translocation leads to the fusion of the CHOP gene with the TLS (Translocated in Liposarcoma; also called FUS ) gene and consecutively to the generation of a FUS-CHOP hybrid protein. The CHOP gene encodes for a transcription factor that is involved in adipocyte differentiation and growth arrest. TLS is an RNA-binding protein involved in RNA processing that interacts with steroid, thyroid hormone, and retinoid receptors. This fusion gene encodes for 3 different transcripts (Types I–III); type II is the one most commonly found in MLPS/RCLPS. Kuroda and colleagues demonstrated that the introduction of the FUS-CHOP fusion gene into preadipocytes caused oncogenic transformation and inhibited adipocytic conversion. Thus, the FUS-CHOP fusion gene is believed to act as an aberrant transcriptional regulator that interferes with adipocyte differentiation, thereby stimulating adipocytic proliferation and tumor initiation.
PLPS
PLPS is defined as a pleomorphic high-grade sarcoma that contains lipoblasts but no areas of WDLPS or any other line of differentiation. Immunohistochemistry may help in the differential diagnosis with other pleomorphic high-grade sarcomas. Approximately 30% to 50% of all PLPSs may stain positive for S-100; the nonlipogenic areas may stain positive for smooth muscle actin (45%–49%), CD34 (40%), and desmin (13%–19%) ; and a subset of PLPS may stain positive for epithelial markers (epithelial membrane antigen [EMA], 26%; keratin-6, 21%). Genetically, PLPSs usually have high chromosome counts and complex structural rearrangements. Unlike WDLPS/DDLPS and MLPS/RCLPS, no consistent oncogenic event can be found.
Approximately 5% of all LPSs cannot easily be categorized into the previously mentioned categories. Sometimes more than one growth pattern may be observed; in this case, these tumors may be classified as LPS of mixed type.
Clinical Appearance
LPS usually presents as a painless enlarging mass. Men and women are equally affected, most patients are diagnosed in the sixth decade. Depending on growth rate and site of the primary, LPS can attain a very large size and still remain asymptomatic. WDLPS is a locally aggressive, nonmetastasizing tumor that grows slowly and is rarely symptomatic. Retroperitoneal WDLPSs do not have metastatic potential; however, they can progress to high-grade DDLPS and have a high tendency to recur, with then an unfavorable prognosis. Progression to DDLPS occurs more frequently in retroperitoneal than in extremity WDLPS (17% vs 6%) and more often in recurrent disease; 20% of first-time retroperitoneal recurrences compared with 44% of second time local recurrences progress.
MLPSs occur mainly in the deep soft tissues of the extremities with a predilection within the musculature of the thigh. Retroperitoneal MLPSs are rare, and patients are generally younger than patients with WDLPS/DDLPS. These tumors frequently recur, and 1 in 3 patients develops distant metastases and dies of disease. These metastases often occur in unusual sites, such as soft tissues rather than in the lungs. Notably, rate of osseous metastasis (17%) is as high as the rate of pulmonary metastases (14%).
PLPSs are high-grade LPSs that tend to occur in the lower extremities (47%); other sites, such as the upper limb (18%), trunk (14%), or retroperitoneum (7%), are rare. Compared with other LPS subtypes, they behave more aggressively. They grow quicker, recur locally in 30% to 50%, have a 30% to 50% metastasis rate, and an overall tumor-associated mortality of 35% to 50%. In contrast to WDLPS and MLPS, the preferred site of metastasis is the lung. When compared with other high-grade, pleomorphic sarcomas, however, PLPS shows a comparatively prolonged clinical course.
Diagnosis/Imaging
Patients suspected of LPS should be managed by a multidisciplinary team with expertise in treating sarcomas. As LPSs often present as heterogeneous masses with both well-differentiated and dedifferentiated areas, magnetic resonance imaging (MRI) or computed tomography (CT) scans should be done before biopsy. WDLPS usually exhibits as a large encapsulated lipomatous mass with thick internal septations and may include focal nodules. A nodular focus of nonlipogenic tissue larger than 1 cm inside a WDLPS is suggestive of a DDLPS. Therefore, a biopsy should be directed at the nonlipogenic focus. Open biopsies should be preferred over needle biopsies, when feasible, to maximize the chance to detect dedifferentiated areas, as these are of greatest importance for treatment decisions.
Owing to their high water content, MLPSs often pathognomonically present with low signal intensity on T1-weighted and marked signal intensity on T2-weighted MRI. The tumors are usually large, well-defined, and multilobulated intermuscular lesions, with inclusions of adipose tissue. Staging should be completed in all patients diagnosed with LPSs using chest CT, abdominal CT, and a bone scan at baseline. As low-grade LPSs, especially at the extremities, very rarely metastasize, chest radiographs can substitute for CT scans during follow-up.
As MLPSs frequently metastasize to the spine, whole-spine MRI should be routinely performed to screen for spinal metastasis. Even though local therapy for metastatic disease in this setting is mostly palliative, some long-term survivors have been seen after wide resection of solitary lesions.
Prognostic Factors
Most prognostic data on LPSs are based on retrospective analyses from large sarcoma centers; population-based studies are available from Scandinavia ( Table 2 ). Even though patient groups varied considerably between the different studies, histology/grade and site were the most important factors.
| Subtype | Recurrence, % | Metastasis, % | OS, % | DSS, % | Prognosis Factors |
|---|---|---|---|---|---|
| WDLPS | 13–46 (extremity) 91 (retroperitoneal) | Very low | 76–93 | 86 | Location; margin |
| DDLPS | 18–57 | 13–47 | 54–64 | 66–89 | Location; mitotic count |
| MLPS/RCLPS | 7–28 | 10–58 | 40–75 | 69–100 | Age; RC-component |
| PLPS | 16–45 | 32–44 | 0–63 | 50 | Mostly none |
Low-grade LPSs of the extremities or trunk have a 95% disease-specific survival (DSS), compared with 70% DSS of high-grade LPSs of the same location. Low-grade LPS of the retroperitoneum had an 87% DSS, whereas high-grade tumors had only 50% DSS. Other reported prognostic factors included margins and treatment at large sarcoma centers.
For WDLPS, Weiss and Rao were able to show that almost all (91%) retroperitoneal tumors recurred, compared with 43% of those with extremity site. For DDLPS, the risk of metastatic disease was similar regardless of site of primary, but the DSS was considerably worse for the latter (89% vs 66%).
In MLPS and RCLPS, several groups have identified a round-cell component (5%–25%) and presence of necrosis as prognostic factors. In the analyses of Kilpatrick and colleagues, tumors with a round-cell component of more than 25% metastasized in 58% and had a 10-year DSS of 40% compared with a metastatic risk of 26% and 10-year DSS of 66% in those with a round-cell component of less than 25%.
For PLPS, Hornick and colleagues reported age older than 60 years, central location, tumor size, and mitotic rate as predictors for an adverse outcome.
Therapeutic Strategies in LPS
Treatment of localized disease
Like other well-differentiated sarcomas, low-grade LPSs are treated by surgery alone when negative margins can be achieved. As ALTs of the extremities very rarely metastasize, re-resection can be omitted in selected patients with positive margins when this procedure would be associated with increased morbidity. However, in these patients, a regular, reliable follow-up must be ensured.
A wide resection is the standard of care for LPSs with intermediate to high grade, and most investigators recommend a resection margin of at least 10 mm of adjacent normal fat or muscle tissue. In case of close or positive margins, re-resection should be considered whenever feasible. For high-grade LPSs that are located close or adjacent to a neurovascular bundle, it may be necessary to sacrifice important structures so as to achieve wide margins. Alternatively, neoadjuvant or adjuvant treatment using radiotherapy and/or isolated limb perfusion (extremities only) may allow smaller margins (<10 mm). Amputation does not improve survival compared with resection followed by radiotherapy, but can be necessary in patients with chronic infections, severe pain, or lymphedema that results in severe functional impairment. Adjuvant radiotherapy in soft tissue sarcoma of the extremities has been shown to effectively prolong relapse-free survival (RFS), but not overall survival (OS).
Neoadjuvant radiotherapy allows smaller radiation fields with equal local disease control. Although short-term wound complications are more common, late effects of radiotherapy are substantially less frequent.
The role of chemotherapy (CTX) in soft tissue sarcoma remains a matter of dispute and cannot be unequivocally recommended. A limited number of mostly small randomized trials are available for the group of all sarcomas, and no subtype-specific trials have been performed for LPSs. In 1997, the sarcoma meta-analysis collaboration (SMAC) published a meta-analysis of 14 adjuvant trials showing a 10% absolute benefit in RFS, and a 4% improved OS after 10 years, which was not statistically significant. Most trials did not incorporate ifosfamide or used inadequate doses and some trials also included low-risk sarcomas, hence limiting the value of the analysis from today’s perspective. Only 10% LPSs were included. An updated meta-analysis published in 2008 incorporated 4 new ifosfamide-containing combination studies, which amounted to an 11% absolute benefit in OS for combination regimen. The strongest evidence in this meta-analysis was based on the Italian Sarcoma Group trial that had focused on patients with stage III, G2-3, and extremity sarcomas, and who were treated with high doses of ifosfamide and epirubicin. The trial, albeit small, resulted in a 19% absolute benefit in OS after 4 years. This trial was recently contrasted with the results from the European Organisation for Research and Treatment of Cancer (EORTC) Soft Tissue and Bone Sarcoma Group trial of adjuvant CTX using doxorubicin and ifosfamide in soft tissue sarcoma, which did not improve OS (66.5% vs 67.8% after 5 years). Unfortunately, this trial had used rather low doses of ifosfamide and also included intra-abdominal and stage II sarcomas. Again, no LPS-specific data have been extracted from these trials.
The largest analyses on the role of adjuvant CTX in LPS (n = 246) was published in 2004 by Eilber and colleagues, who retrospectively analyzed all primary resectable high-grade extremity LPSs treated at the University of California Los Angeles and Memorial Sloan-Kettering Cancer Center (MSKCC) from 1975 to 2003. They compared the impact of a doxorubicin-based regimen used from 1975 to 1990 and an ifosfamide-based regimen used from 1990 to 2003 with patients who did not receive adjuvant CTX in the same period of time. In their analysis, ifosfamide-containing treatment was associated with improved OS (92% vs 65% after 5 years), whereas doxorubicin treatment was not. Subgroup analyses showed that tumors larger than 10 cm benefited the most from CTX.
For patients with retroperitoneal LPS, local recurrence rates of more than 80% are reported and because of their location, tumors tend to grow large and often infiltrate adjacent structures at the time of diagnosis. Wide resection is the only curative treatment approach and complete resection is associated with significantly longer DSS than incomplete resection (73% vs 43% at 3 years). A median survival for completely resected tumors of 103 months has been described compared with 18 months after incomplete resection. Aggressive surgery generally aims at en bloc resections of the tumor and adjacent organs that are infiltrated by the tumor. Frontline aggressive surgery that is performed in high-volume centers is safe and associated with better outcome compared with less-aggressive strategies. Very few data are available on the role of CTX in retroperitoneal LPS. Additive radiotherapy can be used in incompletely resected tumors, but usually postoperative radiotherapy is limited by the size of the fields and intestinal toxicity. As tumors may serve as their own spacers to reduce radiation to the intestine, neoadjuvant radiotherapy strategies are currently being investigated in retroperitoneal sarcomas (EORTC 62092).
Treatment of locally advanced or recurrent disease
For the treatment of locally advanced LPSs, several neoadjuvant or definitive treatment modalities can be used to achieve local tumor control, including radiotherapy with and without CTX or hyperthermic isolated limb perfusion.
For isolated limb perfusion, the circulation of the extremity is isolated from the body circulation and perfused with a hyperthermic solution of melphalan and tumor necrosis factor (TNF)-α using a heart-lung machine. This prevents TNF-α from entering the systemic circulation, which may cause severe toxicity, such as capillary leak syndrome. Effectiveness in extremity soft tissue sarcoma has been shown in large multicenter studies with response rates of 75% to 85% and limb salvage in more than 85% of patients. Perfusion may allow function-sparing surgery, as frequently tumor margins are completely devitalized, allowing nerve- and vessel-sparing resection. Subtype-specific data are scarce, but some evidence suggests that LPS may respond less frequently than other subtypes, such as undifferentiated sarcomas, leiomyosarcoma, or clear-cell sarcoma.
In patients for whom no acceptable surgical option is available, definitive radiotherapy represents a treatment option, with 5-year local control rates of 30% to 45% and 5-year OS of 25% to 35%.
Systemic CTX may improve the response rate when combined with radiotherapy, but few data are available on the different LPS subtypes; however, combinations of doxorubicin ± ifosfamide are used in combination with radiotherapy. In MLPS, trabectedin treatment has yielded remissions rates of 24%.
In retroperitoneal recurrences, surgery represents the only viable treatment modality; however, surgical approaches cause 3% to 6% mortality and considerable morbidity. A watch-and-wait strategy can be safely applied in asymptomatic recurrences of WDLPS; symptomatic or progressive LPS should, however, be evaluated for surgical treatment. Lewis and colleagues proclaimed that once retroperitoneal soft tissue sarcoma recurs, the outcome of the patient is dictated by tumor biology rather than treatment variables, such as resection margins. Park and colleagues analyzed 105 patients with recurrence of retroperitoneal LPS and were able to show that only patients with a growth rate of less than 0.9 cm per month gain a survival benefit from aggressive resection. They proposed the “1 cm per month rule,” by which tumors with faster growth rate will not benefit from surgery. Therefore, these patients should be offered systemic treatment, potentially followed by surgery in case of response. As incomplete resection does not prolong survival, it should be restricted to patients with existing or immanent tumor-related symptoms.
In patients in whom local treatments cannot be offered because of decreased performance status or extent of disease, CTX should be offered in analogy to patients with metastatic disease.
Treatment of Metastatic Disease
In patients with low-grade, slow-growing tumors, surgery may allow disease control over many years, especially in patients with intra-abdominal tumor spread. Complete resection of metastases restricted to the lung has been associated with prolonged disease-free intervals in sarcomas in general. Notably, histology of LPS was associated with an unfavorable outcome in a large series of patients who underwent metastasectomy.
In patients with fast-growing, high-grade tumors, systemic CTX remains the mainstay of treatment. Approved drugs for LPS are doxorubicin, ifosfamide, dacarbacin (DTIC), and trabectedin (EMA) with gemcitabine ± docetaxel being frequently used in clinical practice. In general, sequential monotherapy represents the standard approach in LPS and doxorubicin the standard first-line therapy for this subtype.
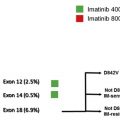
Most clinical trials published on soft tissue sarcomas report on LPSs as a whole group regardless of the fact that response rates may vary considerably between different LPS subgroups. Few large retrospective studies have addressed this lack of detail ( Table 3 ).