Introduction
Successful long-term diabetes self-management requires the integration of pharmacotherapy, proper nutrition, home blood glucose monitoring, continuing patient education, an increase in physical activity, and surveillance for and prevention of short- and long-term complications. Although physicians are eager to prescribe pharmacotherapy to their patients, discussing issues such as home blood glucose monitoring, diet, and exercise is not second nature. Most physicians have had little direct training regarding lifestyle issue management with patients, preferring instead to refer to a dietitian or certified diabetes educator (CDE). Primary care doctors must understand that they remain the “director” of the patient’s management team. Although dietitians and CDEs can educate patients on lifestyle interventions, the physician is responsible for prescribing the actual dietary and activity parameters that patients follow.
Some PCPs have no access to ancillary personnel and may be their patients’ only source of information regarding lifestyle modification. Physicians should encourage the adaptation of healthy and active lifestyle interventions within their patient population who have diabetes or prediabetes. Spending 3 to 5 minutes per visit on lifestyle intervention could have a positive and motivational effect on patients. If, for example, a patient has been successful in losing weight, ask what techniques were used and never forget to praise his or her efforts. One should ask about exercise and smoking cessation at each visit. The physician should make certain that the patient knows the names of his or her medications and the times they should be taken. Determine what drugs need to be refilled so that lapses in treatment will be minimized. While sitting side by side with each patient, the physician should discuss the statistical evaluations of home blood glucose monitoring. Time spent on this will most certainly encourage the patient to continue monitoring. However, a patient who does take the time to monitor and brings the meter in for downloading will certainly become discouraged if no interest is shown in the glucose readings and the efforts are ignored.
Lifestyle interventions are clearly beneficial for patients diagnosed with diabetes. Reducing caloric intake to 1,100 kcal per day has been shown to decrease fasting blood glucose levels in obese patients with T2DM and in those with normal glucose tolerance in as few as 4 days.
1 This improvement is due to decreased hepatic glucose production. Insulin sensitivity and fasting glucose levels decline further following 28 days of calorie restriction in obese patients with T2DM in
association with an average weight loss of only 6 kg. Interestingly, the weight reduction does not appear to have a positive effect on pancreatic β-cell preservation or secreting capacity.
2In a recently published study, basal hepatic glucose production, hepatic and peripheral insulin sensitivity, and β-cell function were measured in 11 patients with T2DM at baseline as well as after 1, 4, and 8 weeks of a very-low-calorie (600 kcal per day) diet.
3 The patients had a duration of diabetes of less than 4 years and a stable BMI ranging from 25 to 45 kg per m
2. After 1 week of caloric restriction, patients began to experience normalization of both β-cell function and hepatic insulin sensitivity as well as a decrease in pancreatic and liver triacylglycerol stores. Intrahepatic lipid concentrations decreased by 30%. Over the 8 weeks of dietary restriction, β-cell function increased toward normal and pancreatic fat decreased. As one is exposed to severe caloric restriction, intracellular free fatty acid concentrations in the liver decline resulting in mirrored decrease in hepatic export of lipoprotein triacylglycerol to the pancreas. Prolonged elevations of plasma free fatty acids decrease insulin secretion. Prior to the onset of spontaneous diabetes in rats, both total pancreatic fat and islet triacylglycerol content increase sharply.
4 Chronic saturated fatty acid exposure of β-cells also inhibits acute first-phase insulin response to glucose, whereas removal of the free fatty acids allows for recovery of this acute response as demonstrated in this study.
5 Thus, the primary pathologic abnormalities associated with T2DM can be reversed simply by reducing dietary energy intake.
Diabetes and mental illness interact in harmful ways (See
Chapter 9). Patients with both diabetes and mental illness tend to be less adherent to medical care and suffer more long-term diabetes-related complications. Comorbid depression and diabetes result in worse health outcomes than other combinations of chronic diseases.
6,
7 Integration of both medical and psychosocial support for such patients, although challenging, is necessary to minimize risk of premature death from suicidality or cardiovascular disease.

Improving Adherence to Diabetes Self-management Skills
Physicians can encourage patients to become active participants in their own care by simply asking how they feel about what has been prescribed to date. What efforts are working and what issues need fine tuning? Are there concepts related to the disease state of diabetes that the patient does not understand? A proactive approach to education in many cases will minimize the likelihood of patients seeking out their own sources of questionable resources from, for example, Internet chat rooms.
Behavioral changes are necessary to reduce long-term risks and maintain healthy lifestyles. By some estimates, less than 50% of patients with diabetes adhere to their recommended behavioral interventions.
8 Adherence is multidimensional in that some patients may comply with medication regimens, while ignoring dietary or exercise recommendations. Others, who “feel just fine,” may exercise 2 to 3 hours a day so that they may avoid starting medications that are needed to manage hyperglycemia, hypertension, and hyperlipidemia. A study using a large national sample (National Health and Nutrition Examination Survey [NHANES]) of patients with T2DM found that 29% of insulin-treated patients, 65% of those on oral medications, and 80% of individuals managed by diet and exercise alone either never performed self-blood glucose monitoring (SBGM) or did so less than once per month.
8The findings from the Cross-National Diabetes Attitudes, Wishes, and Needs (DAWN) Study
9 showed patient-reported adherence rates for medication in T1DM and T2DM patients of 83% and 78%, respectively; self-monitoring blood glucose adherence was 70% and 64%, respectively; and appointment-keeping adherence was 71% and 72%, respectively. The adherence rates observed for diet for T1DM and T2DM patients were 39% and 37%, respectively, and for exercise they were 37% and 35%, respectively. Providers reported significantly better adherence for T1DM than for T2DM patients across most treatment regimens.
Several factors have been shown to influence adherence with diabetes self-care, as summarized in
Table 3-1. Demographic factors such as ethnic minority, low socioeconomic status, and low
levels of education have been associated with lower regimen adherence and greater diabetes-related morbidity.
10 Lower frequency of self-blood glucose monitoring has been observed among African American and Hispanic/Latino patients when compared with non-Hispanic white patients with diabetes (10).
Patients with comorbid mental illness must have their psychological issues corrected before intensification of diabetes therapy is attempted as detailed in
Chapter 9. Both treatment compliance and outcomes are linked directly to the patient’s affective state.
11 PCPs should screen patients with diabetes for mental illness (schizophrenia, bipolar depression, major mood disorder, and generalized anxiety disorder) and initiate treatment when appropriate.
Family relationships play an important role in diabetes management. Greater levels of social support from spouses and other family members are associated with enhanced participation in diabetes self-management and reduce the stress associated with chronic disease management.
10One of the most important motivators of patient compliance is related to the amount of support received from the health-care team members. Patients who are satisfied with their doctor-patient relationship are more adherent to their treatment program and participate more fully in diabetes self-management.
12 One of the key elements to success in achieving good glycemic control for participants in the Diabetes Control and Complications Trial (DCCT) was the amount of support and availability patients received from their local health-care study site.
13Factors that promote adherence include reminder cards and phone calls about upcoming appointments, minimizing delays in seeing patients once they arrive at the office, and reinforcing positive attributes of the visit, rather than focusing on the negative aspects of chronic complications.
14,
15Patients prefer simplified treatment regimens to ones that are more complex and tend to accept the need to begin pharmacotherapy for diabetes much quicker than integrating lifestyle or behavioral changes into their daily lives.
14,
16

Is the Patient “Noncompliant” or “Nonadherent”?
Physicians often relate interesting tales of patient “noncompliance.”
Compliance is best defined as “the extent to which a person’s behavior coincides with medical advice.”
15 Noncompliance implies that patients intentionally disregard or disobey the advice of their health-care provider. Noncompliance provokes negative attitudes toward patients while discouraging patients from becoming active participants in their own diabetes self-management.
Adherence is viewed as an “active, voluntary, and collaborative effort in a mutually acceptable course of behavior prescribed to produce a positive therapeutic outcome.”
15 Patients who adhere to their treatment programs do so by choice, agree to participate in self-management, understand the implications of treating all metabolic abnormalities to target, and agree to become students of their own disease states. Once presented with a treatment plan and provided with the tools necessary to become successful at self-management, a patient may voluntarily choose to adhere to the prescribed plan, offer alternative suggestions to the professional team, or, most commonly, comply with the structured plan for a short time before becoming nonadherent. Patient adherence may be multidimensional. For example, patients may have no problems using four injections of insulin daily, yet only monitor their blood glucose levels once or twice daily despite warnings that failure to monitor may result in hypoglycemia.
In an attempt to enhance patient adherence to a prescribed treatment program, health-care providers should consider the following options:
1 / Allow patient adherence to evolve over time. Weight loss and increased physical activity can prevent or delay diabetes and complications related to prolonged exposure to hyperglycemia.
17 Techniques that facilitate adherence to lifestyle changes can be adapted to primary care. Often the patient’s readiness to work toward change must develop gradually. Patients facing the long-term task of adjusting their lifestyle benefit from assistance in setting highly specific behavior-outcome goals and short-term behavior targets. Individualization is achieved by tailoring goals and targets to the patient’s preferences and progress, building the patient’s confidence, and intensifying therapy as necessary to pursue these prescribed metabolic targets. Coach patients on ways they may achieve positive outcomes. Help them become self-reliant, and minimize their perceptions of burdensome lifestyle interventions. Patients who have multiple comorbidities (hyperlipidemia, hypertension, chronic renal failure, mental illness, severe clinical obesity, autonomic dysfunction, diabetic retinopathy) associated with their diabetes diagnosis should be referred to other specialists and ancillary personnel for intensive intervention education and management.
2/ Target a single behavioral change rather than multiple interventions at each visit. When promoting behavioral or lifestyle changes, the physician should focus on a single intervention at each visit. For example, attempting to discuss appropriate timing of home blood glucose monitoring and smoking cessation at a single 15-minute visit is unlikely to yield any positive results. Diabetes is a stressful disorder, as is nicotine abuse. A discussion of diet, weight loss, exercise, and medication timing, while arranging for specialty evaluations to monitor for retinopathy, is too overwhelming for even the most dedicated patient (
Table 3-2).
3/ Praise the patient at each visit. One should offer praise to each patient at the time of the follow-up appointment. As difficult as this may be for some physicians to accept, patients often do what they can in an attempt to find favor in the eyes of their health-care team. Patients will bring in their glucose logs, their medication vials, or articles of interest that they read on diabetes management. Taking a minute to visually inspect these items means a great deal to patients. Those individuals who have been successful at weight reduction or smoking cessation or who initiated an exercise program should receive praise from the physician and a “high five.”
4/ Do not be afraid to change course. Some physicians may be reluctant to intensify diabetes treatment because they may view a deterioration in the patient’s condition as a reflection of their own disease state mismanagement. However, diabetes is a chronic disease that is by nature progressive and a “work in progress.” Therefore, if one determines that a patient’s glycemic control is not responding to the prescribed treatment, one should not hesitate to offer an alternative plan.
The physician should remember to target success rather than accept failure. Patients do appreciate the efforts of their health-care management team as long as they can be involved in the decisionmaking process.
5/ Allow patients with poor glycemic control to be comfortable while intensifying their diabetes management. The patients with diabetes who are the most challenging to manage are those who have been under poor control for many years and have already experienced microvascular and macrovascular complications. These unfortunate individuals may have finally decided to get more active in their diabetes self-management, although reversal of end-stage disease is unlikely to occur. Treatment of these patients should still focus on lowering the A1C to the safest target. Patients who have spent the majority of their lives living with glucose levels in the 300 mg per dL range may not feel well when the glucose averages 150 mg per dL. They may develop adrenergic symptomatology suggestive of acute hypoglycemia. These uncomfortable symptoms tend to persist for 2 weeks before subsiding once the glycemic control is normalized. Patients who develop adrenergic symptoms should be reassured that they are simply adjusting their body sensors toward normal glycemic control. If they feel symptomatic, a blood glucose level should be obtained, and if it is 70 mg per dL or greater, no treatment should be attempted. Intensive diabetes management incorporates any modality that improves glucose control and lowers the AIC to target. Patients who feel “miserable” while treatment is intensified may become nonadherent to the prescribed protocol and linger in a state of persistent hyperglycemia.
6/ Maintain a positive attitude for all patients, even those with end-stage disease. Physicians are unable to offer patients a “cure for diabetes.” Still, the physician can provide patients with many therapeutic interventions to improve and maintain glycemic control, enhance quality of life, and treat many of the long-term diabetes-related complications. From a psychological and a physiologic viewpoint, physicians should attempt to allow patients to be as comfortable as possible with their chronic disease management. There are now excellent treatments for painful diabetic peripheral neuropathy that may improve patients’ symptomatology within 2 weeks of beginning medication therapy. Men with erectile dysfunction can nearly always be treated successfully with oral medications, intraurethral pellets, or intracavernosal injections. Early interventions for patients with chronic kidney disease can slow the progression of this disease process. The use of statins and aspirin can improve outcomes in patients at risk for macrovascular disease. Physicians must always work for patients in an attempt to find therapies that can improve their quality of life and minimize future long-term complication risks. Often, patients believe that having diabetes is a “death sentence.” In reality, with proper education and intervention, health-care providers can always offer their patients hope for a brighter future of diabetes management. Physicians must never give up on any patient, no matter how challenging they may be.
7/ Identify and treat patients with comorbid depression. Identifying patients with significant psychosocial issues can improve treatment compliance. Fifteen to twenty percent of patients with diabetes have comorbid depression.
11,
18 These individuals may have a difficult time adhering to self-care behaviors and display worsening of their glycemic control. Treating patients who have major depressive disorder with antidepressants may improve adherence to diabetes self-management programs.
16
8 / Individualize diet and physical activity treatment plans. Individual tailoring of diet and physical activity treatment plans is recommended by major guidelines focused on diabetes, obesity, and exercise.
19,
20 Placing patients on a “1,800-calorie ADA diet” is inappropriate for patients who are lean, active, adolescent, elderly, acutely ill, or incapable of following pigeon-holed recommendations. Healthy food choices and flexible meal plans should be discussed. Patients should be made aware that
diabetes is a disorder of carbohydrate metabolism. Simply avoiding “sugar” in the diet will not improve glycemic control. One should remind patients that glucose is the central nervous system’s obligate source of energy. Without carbohydrate ingestion and glucose utilization, the body cannot survive. However, excessive ingestion of carbohydrates results in the inability of the pancreatic β-cell to produce enough insulin to prevent hyperglycemia. As hyperglycemia is prolonged, glucotoxicity destroys β-cells and other important tissues including the eyes, kidneys, nerves, and endothelial cells.
Patterns of disordered eating behaviors (DEB) should also be identified in patients with both T1DM and T2DM. The incidence of DEB is estimated to range from 3%-26% of all patients with diabetes.
21 Patients with DEB are prone to extreme glycemic variability, diabetic ketoacidosis, abrupt alterations in weight, and maladaptive behavioral patterns.
Patients often are overwhelmed by large goals that seem unachievable. Target behaviors should be phased, using small increments. The physical activity target can be gradually increased from setting a 4,000 steps per day goal for walking using an inexpensive pedometer to more intense activity for longer periods, possibly with the assistance of a personal trainer. Group education sessions for patients with diabetes may be initiated with a 5- to 15-minute period of exercise. Patients should understand that any increase in physical activity is likely to improve hyperglycemia. By starting gradually, the patient can build confidence over time, with each stage having a higher likelihood of lasting success. Small advances also provide many opportunities for physician praise. Putting small steps together side by side will eventually encourage a patient to achieve the treatment target.
9 / Use visual imagery to demonstrate the relationship between hyperglycemia and glucose toxicity. A simple exercise in visual imagery might help patients understand the relationship between hyperglycemia and glucotoxicity. Patients who do not have diabetes have blood that is perfectly fluid in nature. Their blood is pure and fresh, similar to the water coming from a mountain stream. In contrast, hyperglycemia causes blood to become thick, sticky, and gooey, similar to maple syrup. As this hyperglycemic liquid flows through the body, the blood sticks to everything, including the eyes, kidneys, blood vessels, nerves, joints, muscles, tendons, skin, and β-cells. The longer the patient is exposed to hyperglycemia, the more likely he or she is to develop complications from kidney, nerve, eye, and heart disease. No one feels well with maple syrup running through the blood vessels. The clinician’s job is to work with patients to allow them to have the syrup replaced by fresh mountain stream water.
10/ Answer patients’ questions and concerns in a relaxed and labor unintensive manner. Imagine going to your own physician for treatment of a chronic progressive disease such as multiple sclerosis or Alzheimer’s disease. Most likely, you are not an expert or thought leader in your field in this disorder, yet you understand that like many other chronic disorders we manage in primary care, MS and AD cannot be cured. With proper intensive therapy, the disease progression may be slowed and the interruption of your current quality of life will be minimal. Still, aren’t there many questions that you have related to living with either disorder? What are the potential side effects of the medications prescribed, and when should they be taken—with food or on an empty stomach? Will they interfere with your blood pressure or thyroid meds? Are these new meds on my insurance formulary and if so, at what tier co-pay? Have
my lab studies changed at all since the last visit? Do I need any additional studies performed at this time? Are there any clinical trials that may be appropriate for patients such as myself? How much longer will I be able to work before I am forced into retirement? Can you complete these forms for me so that I can acquire a handicapped placard for my car? OK. How would you feel if you asked these questions to your PCP while his hand was cradling the door handle as soon as he entered your exam room? After all, he only has 8 minutes to see you and he is really busy. Patients with diabetes have similar concerns. In fact, they feel frustrated that their questions are not being addressed, yet they are often being berated by providers as being “noncompliant” with their treatment plan. Spending a few extra minutes with each patient at the conclusion of each visit will solidify your relationship with them and assure that you are partnering with them toward improving their quality of life.
Lifestyle interventions that may be used to improve patient adherence with diabetes self-management are summarized in
Tables 3-3 and
3-4.

Dietary Management for T1DM
To maximize success as an insulin-dependent patient, each individual must be cognizant of the following relationships between insulin and food intake:
The onset of action and the duration of action of the prandial (bolus) insulin dose
How much insulin is required to cover the expected glycemic excursions that will result from the consumption of a given amount of carbohydrates (I/CHO). This ratio may be stable throughout the day or may be variable, depending on the degree of the patient’s insulin resistance.
The effect of fat content on carbohydrate absorption
How insulin resistance varies during the day. Additional insulin will be required during periods of peak insulin resistance, whereas reduced doses will be needed during times of minimal insulin resistance.
What level of activity is planned as a dose of insulin is being absorbed. Moderate to heavy physical activity will require a 50% reduction in prandial insulin dosing.
Patients with autonomic neuropathy may have gastroparesis. If insulin is dosed as the patient begins to eat, the patient may develop immediate hypoglycemia due to the delay in nutrient absorption yet will experience postprandial hyperglycemia hours later as insulin levels wane while glucose levels peak.
Although these tasks seem daunting, with practice, most patients can learn the basic principles of medical nutritional therapy. With time, dietary management of diabetes not only becomes second nature but allows patients an opportunity to challenge their own nutritional skills to improve their glycemic control. The DCCT demonstrated that patients who adjusted their food intake and insulin dosage in response to preprandial blood glucose levels achieved lower A1Cs than did patients using conventional therapy.
22 Rather than placing all patients on a “specific diet” (i.e., a 1,800-calorie ADA diet), mealtime flexibility should be encouraged, as patients dose insulin based on their carbohydrate intake. The physician should remember that patients are people too, and restricting food intake due to diabetes will lead to “closet eaters” and “cheaters.” One should allow patients to eat sensibly but insist that appropriate insulin be given for each meal. Structured or paired glucose testing allows one to determine if the premeal insulin bolus is injected at the appropriate time and dose based upon the meal content.
Food contains carbohydrates, fats, and proteins as sources of energy, as well as vitamins and minerals. The carbohydrates in food have the most impact on blood glucose levels. Foods that are high in fat content can contribute to obesity and heart disease while prolonging the time of carbohydrate absorption from the gut. Dietary fat, however, plays only a minor role in glycemic control. Protein is another minor player in short-term glycemic control: 50% of consumed protein is converted into carbohydrate over 4 to 6 hours. By constituting only 10% to 20% of the total daily calorie consumption, dietary protein does not have an impact on blood glucose levels.
Generally, all carbohydrates, the preferred energy source in the body, convert to glucose within 1 to 2 hours after consumption. Variables such as fat, fiber, and the glycemic load of a meal can alter the peak excursion of blood glucose. However, these are secondary to the total amount of carbohydrate consumed. Carbohydrate consumption must be balanced with insulin production and
utilization. Insulin-requiring patients must use exogenous insulin to minimize the upward drive each gram of carbohydrate has on blood glucose levels. Patients with T2DM can balance carbohydrate consumption with exercise and medications, which either enhance the release of endogenous insulin by their pancreatic β-cells or improve insulin sensitivity within skeletal muscle cells and adipose tissue.

Insulin-to-Carbohydrate Ratios and Supplemental Insulin
I/CHO is used to determine how much exogenous (injected) insulin is required to cover a given quantity of carbohydrates. Patients with T2DM who are insulin resistant and/or obese may have lower I/CHO and require more insulin; often, 1 U of rapid-acting insulin analogue is needed to cover 5 g CHO. Conversely, lean patients with T1DM may have a much higher I/CHO and may only require 1 U rapid-acting insulin analogue for each 20 g CHO consumed.
Premeal and postmeal self-monitoring is the optimal way to determine the accuracy of the patient’s “carb counting” and ability to respond with an appropriate insulin dose. There may be variations in the patient’s I/CHO. Each patient will have a unique response to each meal and will need to learn to calculate his or her own individual I/CHO. Patients should to be taught the many nuances of I/CHO:
Patients may have different meal bolus ratios for different times of the day.
Meals with large quantities of fat result in delayed glucose availability.
If the premeal glucose level is within normal limits, the bolus insulin covers food intake only.
Low premeal blood glucose levels require less bolus insulin.
High premeal levels require enough insulin to bring glucose back to normal in addition to insulin to cover food.
One should err on the side of conservative optimism when adjusting insulin doses. Excessive insulin doses should be discouraged. Some patients believe that avoiding hyperglycemia at all cost is critical to their well-being. Often, these individuals will dose themselves into hypoglycemia, only to have to consume additional carbohydrates to reverse their lows. This will result in weight gain and increased insulin resistance.
To calculate a meal bolus dose of insulin based on carbohydrate consumption, the rule of 500 is used:
500/total daily insulin dose = CHO covered by 1 U rapid-actinginsulin analogue (lispro, aspart, glulisine)
An example of the 500 rule in use for an adult: A patient receiving a total of 50 U insulin per day: 500 ÷ 50 U insulin = 10 g CHO per unit of rapid-acting insulin analogue
Patients may need to use supplemental insulin in addition to adjusting for carbohydrate intake if the preprandial blood glucose level is greater than 150 mg per dL. Supplemental insulin can be determined by the
rule of 1,800, which predicts how much 1 U of insulin will lower the blood glucose level: insulin sensitivity factor (1,800 per total daily dose of insulin) (
Table 3-6).
Patients should be instructed on the proper interpretation of food labels, which provide information regarding nutrients, calories, and serving sizes. A can of macaroni may contain 35 g of carbohydrates per serving, which in the example described in
Table 3-6 would require 4 U of insulin coverage. Should the patient eat two servings of macaroni, a total of 8 U plus supplemental insulin for preprandial hyperglycemia would be required to cover this meal.
Some patients may benefit from purchasing carbohydrate-counting books that are available through the ADA (http://www.diabetes.org/home.jsp). Carbohydrate counting does take some practice and is more reproducible in patients having the best overall glycemic control.
We can do some carb counting for two apples—one large, one medium—and determine how much insulin is needed to consume each one. Apples are 13% carbohydrate by weight. A large apple
weighs approximately 238 g, and a medium-sized apple weighs approximately 139 g. The carbohydrate content of each apple is as follows:
Large apple: 238 × 0.13 = 30.9 g of carbs
Small apple: 139 × 0.13 = 18.1 g of carbs
A patient with an I/CHO of 1:10 would need 3.1 U to cover a large apple but only 1.8 U for a medium one. If several foods are added to this meal, the carbohydrate content of each would be determined and added to the premeal carbohydrate count. If 80 g of carbs will be consumed, the patient will need to bolus 8 U of insulin.
Most insulin pumps have “bolus wizard-type” features, allowing patients to input the type of food they will be consuming (even restaurant and fast food items are included in the wizard calculator). Based upon the patient’s I/CHO ratio, the pump will determine for the patient the most appropriate amount of insulin to bolus.
For patients having an aversion to carb counting, use of a simpler prandial insulin dosing method might be considered. Bergenstal et al. compared the efficacy of a simple insulin dosing titration method with carbohydrate counting for adjusting mealtime insulin glulisine and determined
that either method was effective at reducing A1C levels.
23 Based upon the suggestions provided in this publication, we have been initiating prandial insulin at the dose of 0.1 U per kg per meal. Thus, a 70-kg patient would inject 7 U 15 minutes prior to each meal (if the premeal glucose level is greater than 80 mg per dL. If less than 80, the insulin would be injected at the same time the meal is consumed). The dose of insulin would be adjusted as shown in
Table 3-7.
Structured glucose testing should be performed 2 hours after each meal at least three times each week. If the 2-hour postprandial glucose level is either 140 to 180 mg per dL or the “delta” (difference between the baseline premeal glucose and the 2-hour postprandial glucose) is 0 to 50 mg per dL, the amount of insulin provided prior to eating is deemed appropriate. If persistent discrepancies exist, the baseline dose of prandial insulin should be reevaluated. One should also remember that basal insulin should be optimized to allow patients to achieve their fasting targeted blood glucose of 70 to 130 mg per dL.

The Diabetes Food Pyramid
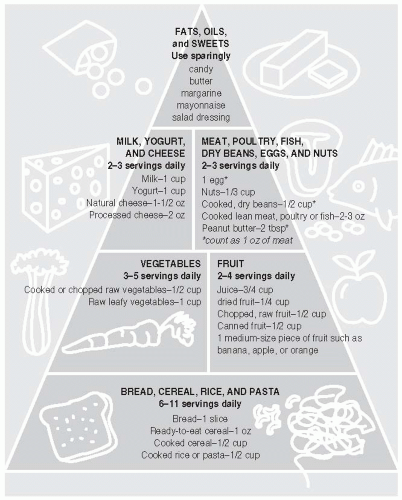
The Diabetes Food Pyramid divides food into six groups (
Fig. 3-1). These groups or sections on the pyramid vary in size. The largest group—grains, beans, and starchy vegetables—is on the bottom. This means that patients should eat more servings of grains, beans, and starchy vegetables than of any of the other foods. The smallest group—fats, sweets, and alcohol—is at the top of the pyramid, suggesting that fewer servings of these items should be consumed.
At the base of the pyramid are bread, cereal, rice, and pasta. These foods contain mostly carbohydrates. The foods in this group are made mostly of grains, such as wheat, rye, and oats. Starchy vegetables such as potatoes, peas, and corn also belong to this group, along with dry beans such as black-eyed peas and pinto beans. Starchy vegetables and beans are in this group because they have about as much carbohydrate in one serving as a slice of bread. Patients are advised to choose 6 to 11 servings from this group daily.
All vegetables are naturally low in fat and good choices to include often in meals or snacks. Vegetables are full of vitamins, minerals, and fiber. This group includes spinach, chicory, sorrel, Swiss chard, broccoli, cabbage, bok choy, brussels sprouts, cauliflower, kale, carrots, tomatoes, cucumbers, and lettuce. Starchy vegetables such as potatoes, corn, peas, and lima beans are counted in the starch and grain group for diabetes meal planning. Three to five servings of vegetables daily should be considered.
The next layer of the pyramid is fruits, which also contain carbohydrates. They also have plenty of vitamins, minerals, and fiber. This group includes blackberries, cantaloupe, strawberries, oranges, apples, bananas, peaches, pears, apricots, and grapes. Although two to four daily servings of fruit are suggested, their effect on blood glucose levels is greatest in the morning when insulin resistance is at its peak. Therefore, delaying fruit consumption until the afternoon when insulin resistance is reduced may help control glycemic excursions after meals.
Milk products contain a lot of protein and calcium as well as many other vitamins. The patient should choose nonfat or low-fat dairy products for the great taste and nutrition without the saturated fat. The ADA recommends two to three milk servings per day.
The
meat group includes beef, chicken, turkey, fish, eggs, and tofu. Beans are in the starch group (1/2 cup of beans equals 15 g of carbohydrates, 3 g of protein, and no fat, unless cooked with
bacon or ham). Other proteins in the meat group are peanut butter, cheese, and cottage cheese. Cheese is high in fat: Usually, 1 oz of cheese contains 8 g of fat. Meat and meat substitutes are great sources of protein and many vitamins and minerals. The patient should choose from lean meats, poultry, and fish and cut all the visible fat off meat. The portion sizes should be small. Three ounces is about the size of a deck of cards. Only 4 to 6 oz per day divided between meals is recommended. The long-term effects of consuming more than 20% of energy as protein on the development of nephropathy have not been determined. However, intake of protein in the usual range does not appear to be associated with the development of diabetic nephropathy.
19The use of fats and sweets (such as potato chips, candy, cookies, cakes, crackers, and fried foods) should be minimized and consumed on special occasions such as birthdays or anniversaries.
The effect of
alcohol on blood glucose levels depends not only on the amount of alcohol ingested but also on the amount of alcohol consumed in relationship to food intake. Alcohol is oxidized by the liver, where gluconeogenesis may become impaired, resulting in hypoglycemia. Because both insulin and alcohol can inhibit gluconeogenesis, patients with T1DM who inject insulin and drink alcohol without eating may develop severe hypoglycemia. Alcohol also increases triglyceride levels, resulting in hyperlipidemia.
28,
29 In general, the effects of alcohol on glucose metabolism are
not severe. Because insulin is not required to metabolize alcohol, no food group need be eliminated from the calculated intake. One must always remember that alcohol adds calories to the diet and, for this reason, is counted in the fat exchange group (
Table 3-8). Patients with pancreatitis, dyslipidemia, or neuropathy should avoid the use of alcohol.
28