and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Incidence
Leg ulcers are common in SCD. The incidence ranges from 2.5 to 25 % in the US and 30–75 % in Jamaica. They are more common in men and in patients with low steady state hemoglobin and high hemolytic rate. The most frequent sites are the medial and lateral aspects of the ankle, but they can also affect the heel and dorsum of the foot and can be circumferential.
Pathogenesis
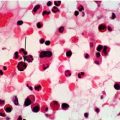
Leg ulceration is thought to be related to impaired microvascular circulation and vaso-occlusion in the small dermal vessels. This is most likely to cause problems in the peripheries of the lower limbs, where circulation is more prone to becoming compromised, and where, in SCD, tissue oxygen levels are particularly low. Ulcers may occur spontaneously or secondary to trauma such as from an insect bite, or through wearing inadequate footwear. Other contributory factors are venous incompetence, peripheral edema, abnormal autonomic vascular control and decreased oxygenation. Low nitric oxide levels probably also have a role in provoking vascular dysfunction. Biopsy of involved skin may show microvascular changes including intimal proliferation, neovascularization and perivascular proliferation similar to the changes seen in diabetic or vascular ulcers.
Clinical Presentation/Course
The typical established ulcer is round, with raised margins, and a deep base containing necrotic slough, often with surrounding hyperpigmentation. It is not unusual for patients to present after weeks or months of self-management. Leg ulcers in SCD are almost invariably painful and neuropathic pain is common. Stiffness and decreased range of movement in the ankle joint is seen in over 50 % of cases. Complications include superinfection, osteomyelitis, psychosocial disturbance and deterioration in quality of life. Whilst early treatment can be effective, delays may lead to development of large, persistent ulcers. It is not unusual for a large, deep ulcer to require several years to heal, with a high risk of recurrence after minimal trauma.
Diagnosis and Investigation
This is a clinical diagnosis, however complicating conditions should be excluded as these will influence response to treatment. Microbiological swabs should be taken to exclude secondary infection. It may also be appropriate to assess for lower limb venous incompetence, and to exclude underlying osteomyelitis with X-ray or MR scan. Zinc deficiency has been associated with leg ulceration and we recommend checking zinc levels and instituting replacement therapy if required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree