Several large case series and single-institution trials have shown that laparoscopy is feasible for rectal cancer. Pending the results of the UK CLASICC, COLOR II, Japanese JCOG 0404, and ACOSOG Z6051 trials, the oncologic and long-term safety of laparoscopic rectal cancer surgery is unclear and the technique is best used at centers that can effectively collect and analyze outcomes data. Robotic and endoluminal techniques may change our approach to the treatment of rectal cancer in the future. Training, credentialing, and quality control are important considerations as new and innovative surgical treatments for rectal cancer are developed.
Following the success and wide implementation of laparoscopic cholecystectomy, reports on the use of laparoscopy for colon resections soon appeared. Unfortunately, due to initial concerns regarding the oncologic quality of the operation and reports of port site implants, there was hesitance in the application of laparoscopy to colon and rectal cancer. Between 1994 and 2004 there were multiple randomized control trials conducted to study the use of laparoscopy for the treatment of colon cancer. The data on colon cancer have since matured, suggesting that laparoscopy offers short-term benefits with no compromise on the oncologic outcome. On the other hand, the number of large multicenter randomized trials on the use of laparoscopy for rectal cancer is limited. The dearth of quality data is probably secondary to the technical challenges of working within the confines of the bony pelvis while adhering to the principles of total mesorectal excision (TME), autonomic nerve preservation, and maintenance of adequate circumferential and distal margin. This review provides an update on the current and upcoming data on the use of laparoscopy for the treatment of rectal cancer. The authors also briefly review the critical areas of technique that affect oncologic resection and the data on the use of robotics for rectal cancer.
Laparoscopic colon cancer surgery
Laparoscopy is now an established technique for the treatment of colon cancer at major centers. Mature data from the COST, COLOR, ALCCaS, and CLASICC trials have clarified that the oncologic outcome and 3- to 5-year survival can be maintained while providing significant short-term benefits. Today, with compelling evidence from the large multicenter trials, there is increasing use of laparoscopy for the treatment of colon cancer, and with standardized techniques laparoscopic colon cancer surgery is being used by surgeons in the community as well.
Laparoscopy for rectal cancer
In stark contrast to the robust data for colon cancer that have developed over the last decade, there are limited quality data on the use of laparoscopy for the treatment of rectal cancer. The United Kingdom Medical Research Council (UK MRC) CLASICC trial is the only major colon cancer trial that did not exclude rectal cancer patients. In the CLASICC trial, a randomized trial involving 27 centers in the United Kingdom, 242 rectal dissections (randomized 2:1, laparoscopic to open) were performed by surgeons who had completed a minimum of 20 laparoscopic colon resections. Even this specialized group of surgeons had a 34% conversion rate to open operation for completion of rectal dissection. Tumor fixation and uncertainty of margins were the 2 most common reasons for conversion. The CLASICC trial offers the highest level of evidence for the use of laparoscopy to treat rectal cancer. In addition, randomized controlled single-institution trials have shown favorable outcomes for short-term results and oncologic parameters. The data from large single-center trials and case series are reviewed in 2 meta-analyses and Cochrane reviews of the data.
Laparoscopy for rectal cancer
In stark contrast to the robust data for colon cancer that have developed over the last decade, there are limited quality data on the use of laparoscopy for the treatment of rectal cancer. The United Kingdom Medical Research Council (UK MRC) CLASICC trial is the only major colon cancer trial that did not exclude rectal cancer patients. In the CLASICC trial, a randomized trial involving 27 centers in the United Kingdom, 242 rectal dissections (randomized 2:1, laparoscopic to open) were performed by surgeons who had completed a minimum of 20 laparoscopic colon resections. Even this specialized group of surgeons had a 34% conversion rate to open operation for completion of rectal dissection. Tumor fixation and uncertainty of margins were the 2 most common reasons for conversion. The CLASICC trial offers the highest level of evidence for the use of laparoscopy to treat rectal cancer. In addition, randomized controlled single-institution trials have shown favorable outcomes for short-term results and oncologic parameters. The data from large single-center trials and case series are reviewed in 2 meta-analyses and Cochrane reviews of the data.
Technique
The authors’ preoperative preparation of the patient includes a mechanical bowel preparation, betadine rectal wash in the operating room, preoperative antibiotics, and deep venous thrombosis prophylaxis with perioperative low molecular weight heparin. The patient is placed in a modified lithotomy position on a cocooning bean bag secured to the operating table with Velcro or safety straps, and padded to prevent pressure injury. It is critical to ensure that the thighs are in line with the torso to avoid interference with the laparoscopic instruments. Pneumoperitoneum is achieved using a Veress needle or an open technique. If a hand-assist device is used, an 8-cm lower midline or pfannenstiel incision is used to gain access.
One 10-mm trocar is placed at the umbilicus for the camera. After achieving pneumoperitoneum, a second 10-mm suprapubic trocar is placed, which is useful for retraction and passage of the Endo-Cutter stapling device. Two 5-mm trocars are placed under direct vision along the right anterior axillary line, the first 2 finger breadths inferior to the costal margin and the second 2 finger breadths superior to the right anterior superior iliac spine. One 5-mm trocar is placed as lateral as possible in the left anterior axillary line.
The patient is placed in Trendelenburg position and tilted to have the left side up. A 10-mm laparoscopic grasper is used to identify and expose the inferior mesenteric artery (IMA), which is the only artery arising from the aorta above the sacral promontory and below the duodenum. Care is taken to retract the small bowel medially so that the entire sigmoid mesentery is in clear view. With upward traction on the IMA, the peritoneum is incised along the inferior border of the vessel. The retroperitoneal window is developed medial to lateral, and the left ureter is clearly identified. The inferior mesenteric vein is identified in a similar fashion between the duodenum and the IMA, running parallel to the aorta at the base of the left colon mesentery. Mesenteric fat is dissected off the vessels to skeletonize the artery and vein completely. The vessels are divided with either an energy source or a stapling device. The authors’ preference is to use to the 5-mm ENSEAL device, applying 3 overlapping burns on the vessel and dividing in the middle. Prior to division, it is essential to ensure that the ureter is not adherent to the posterior surface of the mesentery along its entire course and that the hypogastric nerves are free of the IMA. The sigmoid colon is then freed off its lateral attachments and dissection is carried along the splenic flexure. The retroperitoneum is seen as a purple layer adherent to the mesentery posteriorly. With appropriate traction and countertraction, the left colon mesentery is dissected off the retroperitoneum up to the tail of the pancreas. The patient is placed in reverse Trendelenburg, head-up, position. The avascular plane along the inferior border of the pancreas, just anterior to the pancreas, is incised to gain entry into the lesser sac. The splenic flexure is mobilized completely to gain as much mobility of the colon as possible.
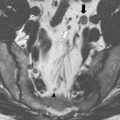
The patient is returned to Trendelenburg position, placed in a neutral right/left position, and attention is then turned to the pelvis. The rectum is retracted anteriorly and out of the pelvis to expose the avascular plane posterior to the mesorectum. The hook cautery is used to develop the posterior plane as far distally as possible and laterally along the pelvic side walls in a semicircular midline motion that follows the curve of the pelvis. The right and left hypogastric nerves are identified and protected. With constant traction on the rectum opposite to the side of dissection, the lateral peritoneal attachments are released. The anterolateral ligaments are then divided with the hook cautery using the areolar tissue plane as the guide for dissection. The mesorectum is dissected to at least 5 cm below the distal level of the tumor.
If the patient is to have a low anterior resection, an endoscopic stapler is placed in the suprapubic port. The mesorectum is divided at right angles to the rectum at the appropriate level using the energy device to facilitate transection of the rectum. An endoscopic gastrointestinal stapler is used to divide the rectum at the desired level 5 cm below the tumor. A stapler that articulates is useful, and often requires 2 or more applications to transect the rectum. There is evidence that minimizing the number of stapler fires for rectal transection may decrease the incidence of anastomotic leaks. The specimen is exteriorized through the ileostomy site or a separate incision. The colon is divided in the standard fashion and the anvil of the circular stapling device placed in the proximal colon. The shaft of the end-to-end anastomosis (EEA) stapler is then placed in the rectum and the anastomosis completed under direct visualization.
If the patient is scheduled to have an abdominoperineal resection, the laparoscopic dissection is carried as far distally as possible. The proximal colon is divided and the specimen left in the pelvis. The trocar sites are closed, and the colostomy placed through the left lower quadrant and matured. The patient is then placed in a prone jack-knife position for the perineal dissection, specimen extraction, and closure.
The specimen is evaluated both macroscopically and microscopically by a specialized pathologist to grade the quality of resection. The specimen is examined by the surgeon and pathologist and inked in the operating room. Quirke and colleagues outlined a protocol to systematically evaluate the macroscopic quality of the TME specimen. The completeness of the mesorectal envelope after the dissection has been shown to correlate with local recurrence and cancer outcomes by the Dutch TME studies. A new classification system of the mesorectal planes was recently described: MA-0 (complete), MA-1 (incomplete but mostly intact), and MA-2 (violated, inadequate mesorectal excision). The distal and circumferential margins should be assessed by an expert pathologist. The importance of the circumferential resection margin has been highlighted by Quirke and colleagues over the years, and documentation of circumferential resection margin involvement is an independent prognostic factor for rectal cancer.
Short-term outcomes
The mean operating time for laparoscopic resection of rectal cancer has been reported to be between 180 and 220 minutes, with most large series reporting longer operative times for the laparoscopic techniques. There are few reports of equivalent or shorter operative times for laparoscopic rectal resection. Most comparative studies and randomized trials report lower blood loss in the laparoscopic group. A recent Cochrane review of the literature confirmed that laparoscopic proctectomy is associated with a lower blood loss. In the CLASICC trial, there was a decrease in median length of stay from 13 to 11 days with no significant difference in the time to first bowel movement and resumption of normal oral diet. Neither the meta-analyses nor the CLASICC trial reported any difference in 30-day mortality. The 2 meta-analyses showed more convincing short-term advantages including a lower incidence of wound infection (0% vs 14%), overall morbidity (21% vs 28%), return of stoma function (1.5 days earlier), and length of hospital stay (2.7 days shorter) for the laparoscopic group. A Cochrane review of 80 studies that included 4224 patients found that laparoscopic TME was associated with quicker return to normal diet, less pain, less narcotic use, and less immune response. The Cochrane review reported a trend toward longer operative time and higher operative cost.
Oncologic outcomes
TME has decreased the incidence of recurrence after proctectomy for rectal cancer. Adherence to the principles of TME with laparoscopic surgery seems critical in maintaining a good oncologic outcome. The best available markers for a successful TME remain evaluation of the quality of the TME specimen, uninvolved circumferential resection margin (CRM), uninvolved distal margin, and maximal lymph node harvest. Even though the 2006 meta-analysis showed no difference in overall oncologic outcomes between laparoscopic and open approaches, the investigators recommended multicenter randomized trials. The rates of positive CRM were lower overall and were not different between the laparoscopic and open groups.
One concerning trend noted in the CLASICC trial was a numerically larger, though statistically insignificant, rate of positive CRM in laparoscopic-assisted anterior resection compared with open resection (12% vs 6%). However, the higher CRM positivity in the anterior resection arm did not translate into a higher local recurrence rate at the 3-year follow up. The overall 3-year survival rate was 68%, with no difference in the survival rate or quality of life between the laparoscopic and open arms. On subset analysis, there was no difference in overall survival between the 2 modalities among patients who underwent an abdominoperineal resection or anterior resection. Of note, the rate of complete TME was higher in the laparoscopic group than in the open group, supporting the argument that laparoscopy may offer better visualization and magnification in the pelvis.
A study specifically designed to assess the macroscopic quality of rectal resections randomized 72 patients to laparoscopic versus open proctectomy. Laparoscopic proctectomy was associated with a lower anastomosis ( P <.001) and a higher likelihood of having an intact visceral fascia. Two randomized controlled trials and other large nonrandomized comparative trials found no difference in the number of lymph nodes retrieved between the laparoscopic and open rectal resections.
Bladder and sexual function
Preservation of pelvic nerves during TME is important to maintain bladder and sexual function. Despite efforts to identify and preserve pelvic nerves during TME, the incidence of bladder and sexual dysfunction has been reported to range between 0% to 12% and 10% to 35%, respectively. Although a beneficial relationship has not been established as yet, the magnification offered with laparoscopic dissection may facilitate the identification of pelvic nerves. In the CLASICC trial, bladder and sexual function were not found to be statistically different between laparoscopic and open TME. Overall 65% of patients were able to void without difficulty. Male sexual function and erectile function tended to be worse in the laparoscopic group than in the open group, though not statistically significant ( P = .063). The investigators attributed the difference to the higher number of TME dissections in the laparoscopic group (80% in the laparoscopic group vs 63% in the open group). On multivariate analysis of the CLASICC data, TME and conversion to open surgery were both independent predictors of postoperative male sexual dysfunction. A recent retrospective review of laparoscopic proctectomy reported a bladder and sexual dysfunction rate of 6%. The investigators attributed their superior results to the experience of their surgeons and highlighted the steep “learning curve” for laparoscopic proctectomy. Preservation of pelvic nerves is clearly an important aspect of proctectomy, and upcoming studies will clarify whether laparoscopy can offer improved identification and preservation of pelvic nerves.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree