Highlights
- •
Suture-free PN is a safe and feasible technique for T1a renal masses.
- •
Suture-free PN benefits short-term and long-term SRF and eGFR compared to conventional Suture PN.
Abstract
Objective
To determine whether argon-beam-coagulation (ABC) suture-free technique results in more favorable renal function than conventional suture technique after laparoscopic partial nephrectomy.
Methods
This study was a single-center, open-label randomized controlled study. A total of 32 patients with T1a renal tumor and R.E.N.A.L score ≤7 were recruited. The primary endpoint of the study was the absolute variation of the ipsilateral split renal function (SRF) at 12 months. The following secondary endpoints were addressed: the 1, 3, 6, and 12-months variation of eGFR; the 1, 3, 6-months variation of SRF; perioperative outcomes (including operative time, warm ischemia time, time to hemostasis, blood loss).
Results
The suture-free group had a significantly shorter operative time (90.4 ± 22.0 minutes vs. 117.8 ± 23.5 minutes, p = 0.003) and warm ischemia time (9.6 ± 4.7 minutes vs. 21.3 ± 8.3 minutes, p < 0.001) than the suture group. At the last follow-up, the change of ipsilateral SRF was 7.5 ± 5.1 ml/min for the suture-free group and 13.1 ± 6.7 ml/min for the suture group ( p = 0.014). The change of eGFR demonstrated a similar trend (5.5 ± 4.4 ml/min vs. 12.6 ± 6.0 ml/min, p=0.001). Multivariate linear analysis confirmed that suture-free technique was associated with a less decrease of renal function.
Conclusions
Suture-free partial nephrectomy is a feasible technique for T1a renal masses and benefits long-term SRF and eGFR compared to conventional procedure.
Introductions
Renal cell carcinoma (RCC) is a malignant tumor originating from renal tubular epithelial cells, accounting for about 2% to 3% of adult malignant tumors. With the popularization of physical examination and the rapid development of imaging, the detection rate of early renal cell carcinoma is increasing year by year. According to the current guidelines, laparoscopic partial nephrectomy (LPN) has become the standard treatment for T1a RCC and an alternative operation for some T1b tumors.
The basic principle of partial nephrectomy is to ensure complete tumor resection while preserving the patient’s renal function as much as possible. With advances in surgical techniques, negative margins have become an achievable goal in most of the large urological centers. Thus, the protection of renal function has become an important goal in the improvement of PN. As reported, more than 25% of patients with localized renal cell carcinoma already had chronic renal insufficiency before surgery and acute kidney injury (AKI) occurred in roughly 20% of partial nephrectomies [ ]. Several studies have shown an independent association between decreased renal function and substantial comorbidity, increased admissions, and increased cardiac-related and non-cardiac- related deaths [ ]. For patients with preoperative chronic kidney deficiency (CKD), the cumulative incidence estimates of CKD progression at 5 years were 21%, which was significantly higher than those with normal baseline renal function [ ]. Plenty of evidence has shown that patients with CKD have lower health-related quality of life (HRQOL) than the general population and even a moderate decrease in estimated glomerular filtration rate (eGFR) is associated negatively with HRQOL, especially among older adults [ , ]. Owing to the impact of AKI and CKD on prognosis confirmed in other medical and surgical fields [ , ], the protection of renal function during PN can significantly reduce the risk of developing renal failure and improve the overall survival of patients [ ]. In the last decade, several techniques have been proposed, such as early unclamping, on-demand clamping and clampless surgery, to minimize or even eliminate the detrimental effect of renal ischemia [ ]. Although several propensity-score matching studies proved the benefit of renal function in the off-clamp patients with one-year follow-up after surgery [ , ], a prospective randomized clinical trial (RCT) of 80 patients who underwent robot-assisted partial nephrectomy showed no significant differences in change of postoperative eGFR or percent split renal function (SRF) between off-clamp and on-clamp groups at a median 3-month follow-up [ ]. In a systematic review, off-clamp PN was only recommended to be particularly applicable for patients with decreased baseline renal function [ ]. Moreover, a recent large multicenter RCT study with 324 patients confirmed that limited warm ischemia in on-clamp group had minimal or no effect on functional recovery after PN in patients with regular baseline function compared with off-clamp [ ].
Considering that the off-clamp PN may not benefit renal function after surgery, the suture-free technique has become a hotspot in the improvement of partial nephrectomy because it avoids the renal parenchymal loss caused by suture to the greatest extent. It has been reported that the use of hemostatic drug spraying, monopolar or bipolar coagulation to achieve suture-free PN does not increase the risk of intraoperative or postoperative complications and has good safety and tumor control results [ ]. However, monopolar/bipolar cautery are good for small capillary and venous vessels and can be helpful in point coagulation of smaller parenchymal bleeding during LPN. Other energy devices, such as Harmonic Scalpel or LigaSure, have also been reported to be used in suture-free PN, but their role in parenchymal hemostasis is limited and need the combination of monopolar coagulation or hemostatic materials [ , ]. In this study, we chose the argon-beam-coagulator (ABC) as the method for hemostasis, because the gas can clear blood and debris from the operative field and improve efficiency of coagulation. Moreover, the ABC method is suitable for hemostasis in PN by creating a thin eschar, with a mean depth of tissue necrosis of 2.4 mm, which minimizes the loss of renal function [ , ]. Retrospective study showed that the decrease in the eGFR at 6-month follow-up was lower in the suture-free PN (5.2%) than in the traditional PN (9.1%) [ ]. However, the evidence level of most of the current studies is low, and no randomized controlled studies have been carried out to determine whether suture-free technique results in more favorable renal function than conventional suture technique after laparoscopic PN.
In this study, we carried out a single-center, open-label, randomized controlled trial to compare the variation of renal function and perioperative complications between suture-free group and the conventional suture group among patients with T1a RCCs who received PN. The results of this study will provide relatively high-quality clinical evidence for the selection of renal reconstruction techniques in partial nephrectomy.
Patients and methods
Study design
This clinical trial (ChiCTR2100053362) was a single-center, open-label randomized controlled study aimed at evaluating the effects of ABC suture-free techniques versus conventional suture method on renal function following laparoscopic PN. The protocol was approved by the Institutional Review Board of Shanghai Ninth People’s Hospital, Shanghai Jiaotong University. All involved investigators—including the surgeon, radiologist, pathologist, laboratory technologist, nurses, and assistants—were thoroughly briefed on the study protocol through both online and offline meetings. The randomization process was executed as follows: a random sequence was generated using software to ensure reproducibility in grouping. The random envelope method was employed to conceal group assignments, with each grouping scheme placed in an opaque envelope labeled sequentially. Codes were inscribed on the envelope’s exterior, which was then sealed and delivered to the researcher. Upon enrollment, each patient was assigned a number, and the envelope corresponding to their group was opened. Patients were randomized to the Suture-free group and Suture group at a 1:1 ratio. All surgeries were conducted by a single surgeon (Dr. Xu), who was informed of the randomization arm immediately prior to the procedure. Additionally, the radiologists, pathologists, and laboratory technologists remained blind to the randomization results throughout the trial. An independent physician, unaware of the randomization information, evaluated all follow-up data and determined whether clinical interventions were necessary to minimize bias.
Baseline, perioperative, and follow-up data was collected with Case Report Form (CRF), including the general information (age, sex, body mass index (BMI), history of hypertension or diabetes), hemoglobin, eGFR and SRF at various intervals post-surgery (1, 3, 6, and 12 months). Data accuracy was ensured through independent recording by 2 clinical research coordinators (CRCs) who had no knowledge of group assignments. A double data entry process was employed, wherein both CRCs entered the data independently to generate a list of discrepancies, which they rectified until their databases were completely consistent. Notably, the CRCs had no access to group allocation information at any point during the study. Preliminary findings indicated that the average decline in GFR at 12 months postsuture-free PN was 6.0 ± 5.1 ml/min, compared to a decrease of 13.6 ± 7.8 ml/min in the suture group. Based on a sample size estimation formula and factoring in a 20% loss to follow-up rate, the minimum required sample size was determined to be 16 patients per group.
Participants
From December 2021 to March 2022, all the consecutive patients clinically diagnosed of renal tumor suspicious for malignancy and intending to undergo PN were screened. Inclusion criteria included: T1a stage renal tumor; R.E.N.A.L score ≤7 points (all participates had a R.E.N.A.L score ≤7 in the preliminary study); age between 18 and 75 years old; ECOG score: 0–1 points; females of childbearing age should agree to use contraceptive measures during the study period. Exclusion criteria encompassed patients with contraindications for general anesthesia, as well as those with comorbid conditions potentially affecting renal function during the study period, as assessed by the investigator. Detailed inclusion and exclusion criteria are presented in Table S1 .
Surgical procedures
Patient positioning and port placement
LPN was performed via the transperitoneal or retroperitoneal approach according to the location of tumor and the surgeon’s preference. For transperitoneal LPN, patients were administered general anesthesia and placed in the standard flexed lateral position. Three trocars were utilized: a 12-mm trocar was placed lateral to the rectus muscle at the umbilicus level for the camera; another 12-mm trocar was positioned lateral to the rectus muscle inferior to the costochondral margin, and a third 12-mm working trocar was set within the midclavicular line, lateral to the first. An additional 5-mm subxiphoid trocar may be added for liver retraction during right-sided LPN. In the case of retroperitoneal LPN, 3 trocars were inserted below the tip of the 12th rib, 2 cm above the iliac crest, and along the anterior abdominal wall.
Tumor resection and hemostasis
The procedures for tumor identification were consistent in both Suture-free and Suture groups. After incising Gerota’s fascia and perinephric fat, the tumor and surrounding renal parenchyma were exposed. The renal hilar artery was subsequently clamped. In the Suture-free group, tumors were excised with cold scissors and enucleated with a suction aspirator within the tumor’s pseudocapsule. Any prominent vessels supplying the tumor were clipped with hem-o-lok during the resection. Once complete tumor resection was achieved, the tumor bed was treated with ABC (ERBE VIO300D, Germany, 120W) to control bleeding. Following this, the renal hilar artery was unclamped. Should bleeding reoccur, the tumor bed was re-sprayed with ABC until hemostasis was attained. It is important to note that if an opening in the collecting system was identified, a solid stitch was to be applied before ABC spraying commenced. In the Suture group, the tumor bed was closed with a first-layer stitch, while the renal capsule was reconstructed as a second layer. A drain was placed postsurgery for several days.
Endpoints
The primary endpoint of the study was the absolute variation of the ipsilateral SRF at 12 months. Secondary endpoints included variations in eGFR at 1, 3, 6, and 12 months; changes in SRF at 1, 3, and 6 months; and perioperative outcomes (such as operative time, warm ischemia time (WIT), time to hemostasis, and blood loss). The time to hemostasis was defined as the interval between the completion of tumor resection and full hemostasis of the tumor bed. Renal dynamic scintigraphy was employed for evaluating SRF, while the EPI equation was utilized for calculating eGFR, as previously described [ ]. The Clavien-Dindo classification system was used to categorize the severity of surgical complications: Grade I represented any deviation from the normal postoperative course without necessity for treatment; Grade II encompassed pharmacological treatment with drugs; Grade III necessitated surgical, endoscopic, or radiological intervention; Grade IV indicated life-threatening complications requiring intensive care unit (ICU) management; and Grade V indicated patient mortality [ ].
Statistical analysis
Frequencies and percentages were reported for categorical variables, while means and standard deviations were provided for continuous variables. Comparisons between pre- and postoperative GFR values were conducted using the t-test, with statistical significance set at p < 0.05. Chi-square tests were employed for comparing categorical variables. A multivariable linear regression model was fitted to assess the impact of suture technique on both short-term and long-term renal function, considering WIT and BMI as covariates.
Results
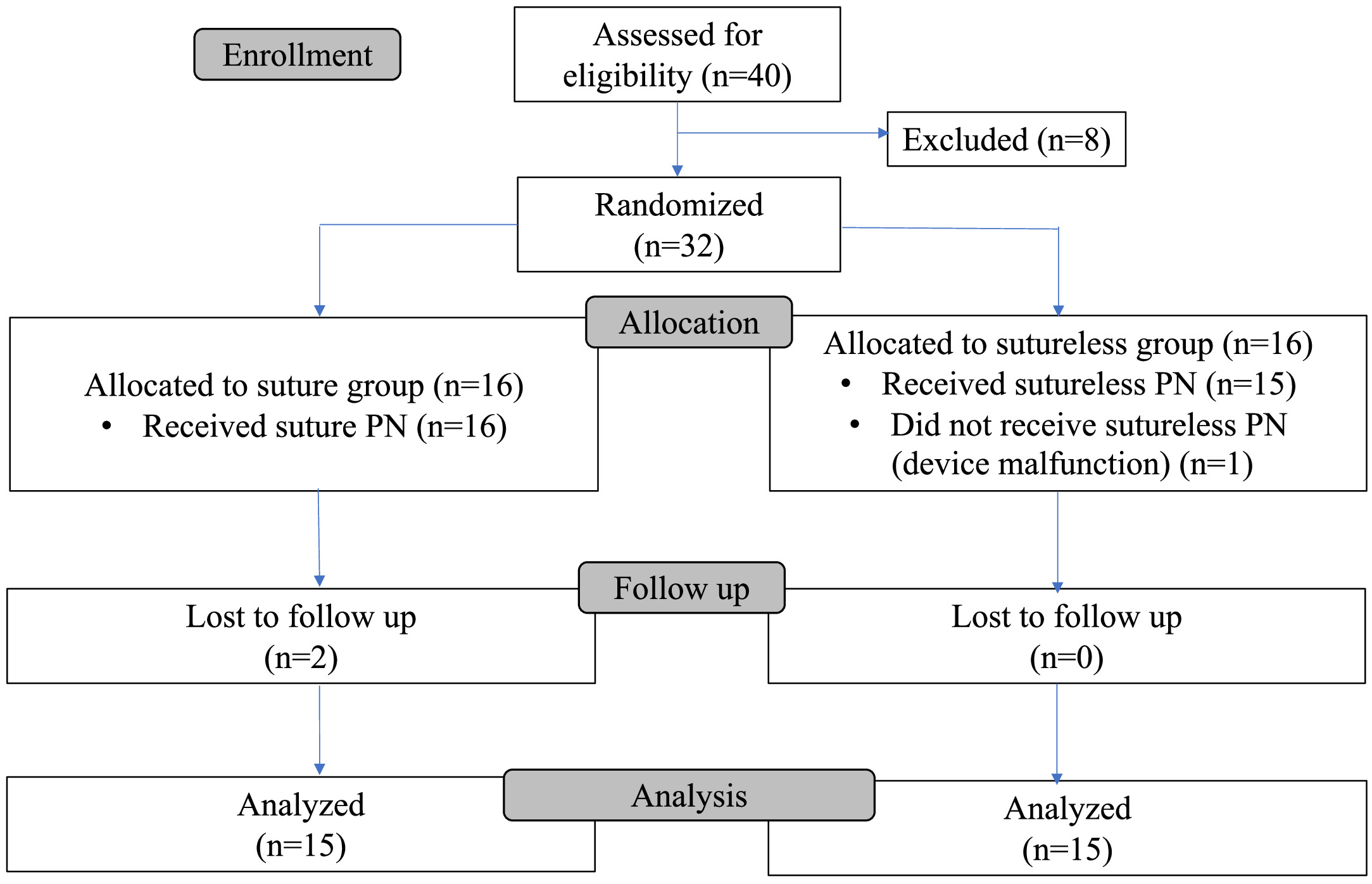
A total of 40 patients were screened. Eight of them were excluded for concurrence with symptomatic urinary stones or cardiac insufficiency. Finally, 32 patients were 1:1 randomized to the conventional-suture (Suture) group and the ABC suture-free (Suture-free) group. One patient was converted from Suture-free arm to Suture arm intraoperatively due to ABC malfunction. Due to the COVID-19 epidemic, 2 patients in the Suture arm were unable to come to the hospital for review after their surgery according to the protocol. Finally, data from 15 patients in the Suture-free group and 15 patients in the Suture group were analyzed to evaluate the effect of suture on renal function after PN ( Fig. 1 ).
The baseline clinical characteristics were shown in Table 1 . Patients in the 2 groups were similar in gender, age, BMI, history of hypertension, diabetes mellitu, smoking status, baseline Hb, tumor size, and R.E.N.A.L. score. The mean size of tumors in both groups were 2.5 cm, with a low R.E.N.A.L. score (5.1 ± 1.0 in Suture-free group vs. 5.4 ± 1.2 in Suture group). The baseline eGFR before surgery was 96.1 ± 20.8 ml/min for Suture-free group, and 93.3 ± 28 ml/min for Suture group ( p = 0.759). However, the ipsilateral SRF on the affected side was relatively poor in the Suture-free group (41.9 ± 11.5 ml/min vs. 47.9 ± 8.8 ml/min), but the difference was not statistically significant ( p > 0.05).
| Variables | Suture-free | Suture | P value |
|---|---|---|---|
| NO. of patients | 15 | 15 | |
| Sex | |||
| Male | 12 | 10 | 0.409 |
| Female | 3 | 5 | |
| Age (y) | 54.2 ± 13.0 | 58.1 ± 13.2 | 0.418 |
| BMI (Kg/m 2 ) | |||
| Smoking | 23.6 ± 3.5 | 24.1 ± 4.3 | 0.722 |
| yes | 9 | 8 | 0.713 |
| no | 6 | 7 | |
| Hypertension | |||
| yes | 6 | 8 | 0.464 |
| No | 9 | 7 | |
| Diabetes mellitus | |||
| yes | 4 | 3 | 0.667 |
| No | 11 | 12 | |
| Hb before surgery | 139.3 ± 22.2 | 137.6 ± 12.8 | 0.795 |
| eGFR before surgery (ml/min) | 96.1 ± 20.8 | 93.3 ± 28.1 | 0.759 |
| Ipsilateral split renal function (ml/min) | 41.9 ± 11.5 | 47.9 ± 8.8 | 0.119 |
| Tumor size (cm) | 2.5 ± 1.2 | 2.5 ± 0.9 | 0.904 |
| R.E.N.E.L score | 5.1 ± 1.0 | 5.4 ± 1.2 | 0.404 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree