Fig. 23.1
Trocar placement and a mini-laparotomy site for laparoscopic proximal gastrectomy. Five trocars are placed in the abdominal wall. The trocar site on the left rectus muscle is extended to 5 cm when the stomach is pulled out of the abdominal cavity
Dissection of the Left Gastrocolic Ligament (Video 23.1)
The assistant holds the left side of the gastroepiploic arcade in the right hand and holds the gastrocolic ligament and stretches it to caudal in the left hand. The surgeon holds the right side of the gastroepiploic arcade in the left hand and dissects an avascular area of the omentum approximately 3 cm apart from the gastroepiploic arcade toward the inferior pole of the spleen using a laparoscopic coagulating shears (LCS) in the right hand (Fig. 23.2). In order to mobilize the stomach freely, the physiological adhesions between the pancreas and the posterior wall of the stomach should be separated properly.
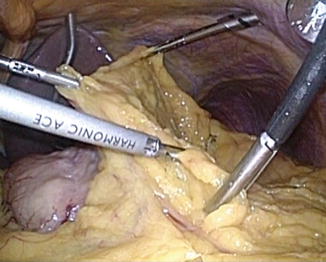
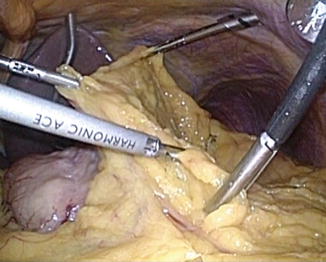
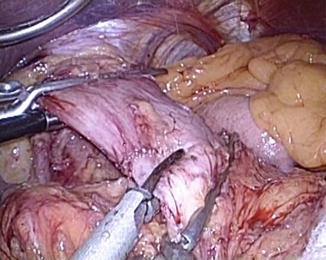
Fig. 23.2
An avascular area of the omentum approximately 3 cm apart from the gastroepiploic arcade is dissected toward the inferior pole of the spleen
To dissect the right gastrocolic ligament, the standing position of the surgeon and the assistant is changed. The assistant holds the gastroepiploic arcade in both hands. The surgeon holds the gastrocolic ligament and stretches the gastrocolic ligament in a caudal direction in the left hand. The surgeon dissects the gastrocolic ligament toward the descending portion of duodenum with the LCS in the right hand (Fig. 23.3). The right gastroepiploic vessels are carefully preserved. If there are abnormally enlarged lymph nodes along the right gastroepiploic vessels or infrapyloric lymph nodes, the operative method needs to be changed to a total gastrectomy, considering the possibility of lymph node metastasis.
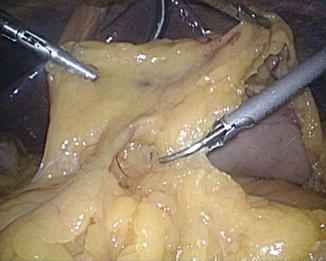
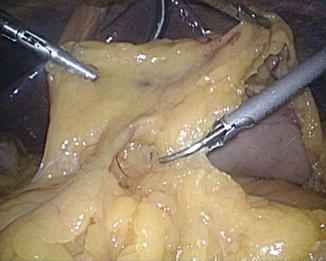
Fig. 23.3
The gastrocolic ligament is dissected toward the descending portion of duodenum
Lymph Node Dissection Along the Left Gastroepiploic Artery and the Short Gastric Artery (Video 23.2)
The assistant grips and lifts the posterior wall of the upper stomach in the right hand and draws the fat tissue near the inferior pole of the spleen to the left and expands the field of view in the left hand. The surgeon identifies the left gastroepiploic artery rising from the tail of the pancreas, peels off the surrounding fat tissue, and dissects the artery distal to the omental branch using the LCS after clipping the artery (Fig. 23.4).


Fig. 23.4
The fat tissue around the inferior pole of the spleen is drawn to identify the left gastroepiploic vessels
The surgeon divides the gastrosplenic ligaments upward toward the superior pole of the spleen with the LCS (Fig. 23.5). It is of particular concern to avoid injury to the spleen or the short gastric vessels by strong traction when the assistant expands the field of view. The short gastric vessels are dissected using the LCS with or without clipping these vessels. Because the gastrosplenic ligaments around the superior pole of the spleen are short, complete dissection should be performed during resection of the esophagus.
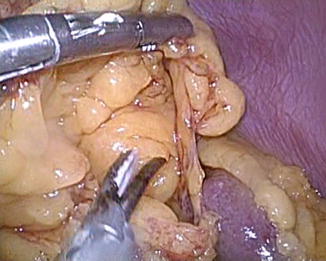
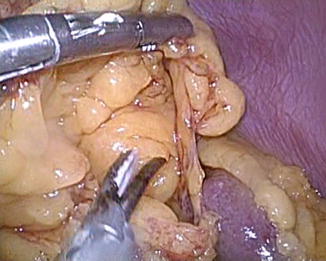
Fig. 23.5
The gastrosplenic ligaments is divided upward toward the superior pole of the spleen
Resection of the Abdominal Esophagus (Video 23.3)
The assistant grips and stretches the lesser curvature in both hands. If there are enlarged suprapyloric lymph nodes, the operative method needs to be changed to the total gastrectomy. The surgeon dissects an avascular area of the lesser curvature along the hepatic branch of the vagus nerve toward the abdominal esophagus. The operating surgeon dissects the esophageal diaphragmatic ligament and exposes the right crus and the front wall of the abdominal esophagus. The fat tissue surrounding the abdominal esophagus is peeled off, and the anterior and posterior branches of the vagus nerves are transected using the LCS. The base of the esophageal cardiac branch of the left inferior phrenic artery is dissected using the LCS after clipping the vessel (Fig. 23.6). After a detachable vessel forceps are applied to the abdominal esophagus, the abdominal esophagus is divided above the esophagogastric junction using the LCS (Fig. 23.7). The residual gastrosplenic ligaments are dissected downward using the LCS with or without clipping of vessels.
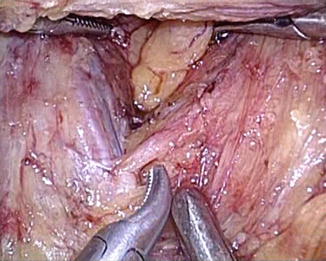
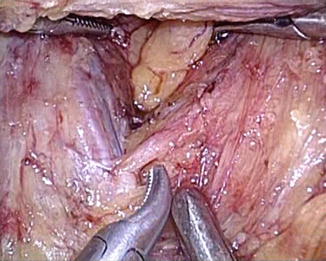
Fig. 23.6
The base of the esophageal cardiac branch of the left inferior phrenic artery is dissected