Figure 17.1
Port placement for laparoscopic distal pancreatectomy. The initial site of entry, whether by the Hassan or Veress technique, is left to the discretion of the surgeon. A supra- or infra-umbilical port (1) should be carefully placed so it can either join or be far enough away from an upper abdominal hand port (2; if necessary). Secondary working ports are placed on the right for tissue manipulation and electrical dissection devices and for retraction if needed (3, 4). Ports on the left are for the camera and more retraction by the assistant (5). This operation can be performed with as few as four ports, but extra ports should be utilized if the operation requires them
17.2.2 Dissection of Peripancreatic Structures
A 30° or 45° camera is introduced and the abdomen is explored systematically for the completion of operative staging. Then the patient is rotated to the right and placed in steep reverse Trendelenburg, and the splenic flexure is lowered using an electrothermal dissector (ultrasonic shears or electrothermal bipolar tissue sealing device). As the operation progresses, the lesser sac is entered and the omentum is separated from the greater curvature of the stomach (Fig. 17.2). The stomach is grasped and held up to expose the plane of dissection for the operating surgeon. If the short gastric vessels are to be divided, take care to completely encompass these vessels with the electrothermal device to avoid partial transection, which can result in significant bleeding. When splenectomy is planned, the dissection is carried up to the fundus of the stomach to free the spleen completely from the stomach.
Once the greater curvature is freed, the stomach can be retracted out of the field under the left lateral segment of the liver. The use of a fixed hand or liver retractor here can facilitate this retraction, which will free the left hand of the assistant. Now that the pancreas is exposed, the dissection begins with freeing of the inferior and superior borders of the pancreas (Fig. 17.3). The inferior border of the pancreas is carefully dissected out by dividing the overlying peritoneum with an electrothermal dissector. The pancreas is then lifted up bluntly with a grasper to facilitate further dissection and careful identification of vascular structures. Laparoscopic ultrasound can help identify small PNETs if necessary to assist with determining the point of parenchymal division, which should be approximately 2 cm proximal to the tumor [8]. Inferiorly, the transverse mesocolon is lowered either laterally from the splenic flexure or medially at the point of transection, using a combination of careful blunt and bipolar dissection. Take care to dissect behind the pancreas carefully, which will allow visualization of the superior mesenteric vein (SMV), inferior mesenteric vein (IMV), and splenic vein (Fig. 17.4). This maneuver is not necessarily performed to assess resectability, but rather to allow these structures to be identified and protected during further dissection and transection of the pancreas. The SMV can be found anatomically by tracing the right gastroepiploic and/or middle colic veins superiorly.
While freeing the inferior border of the pancreas by lowering the transverse mesocolon, take care to identify the IMV to avoid inadvertent injury. Further dissection posteriorly and superiorly will expose the splenic vein. If the pancreas is going to be divided far left of the SMV en masse with the splenic vein, then SMV dissection is not necessary; this decision is dictated by tumor location and pathology. If a formal left pancreatectomy is planned, the dissection is carried medially until the SMV is reached, and then dissection continues under the pancreas while the SMV is freed and protected. At this point in the dissection, the venous structures are fully identified and ready to be divided.
The goal of the dissection at the superior aspect of the pancreas is to identify the splenic and left gastric arteries and to completely free the lesser curvature of the stomach off of the pancreas. Injury to the coronary or left gastric vein during this part of the operation can lead to severe hemorrhage and must be avoided. Identify the splenic artery, which most commonly arises superiorly off of the celiac axis; it is often tortuous and should not be confused with the hepatic artery takeoff (Fig. 17.5). It is important to have the patient’s cross-sectional imaging available to help correctly identify vascular structures and the relationship of these structures to the tumor. The splenic artery does not have to be isolated at the takeoff unless there is concern for proximity of the tumor to the celiac axis. Once the splenic artery is confirmed, it can be taken more distally, when coursing superiorly along the pancreatic parenchyma. The vessel is freed in order to facilitate stapler placement, completing the dissection of the pancreas and major vascular structures.
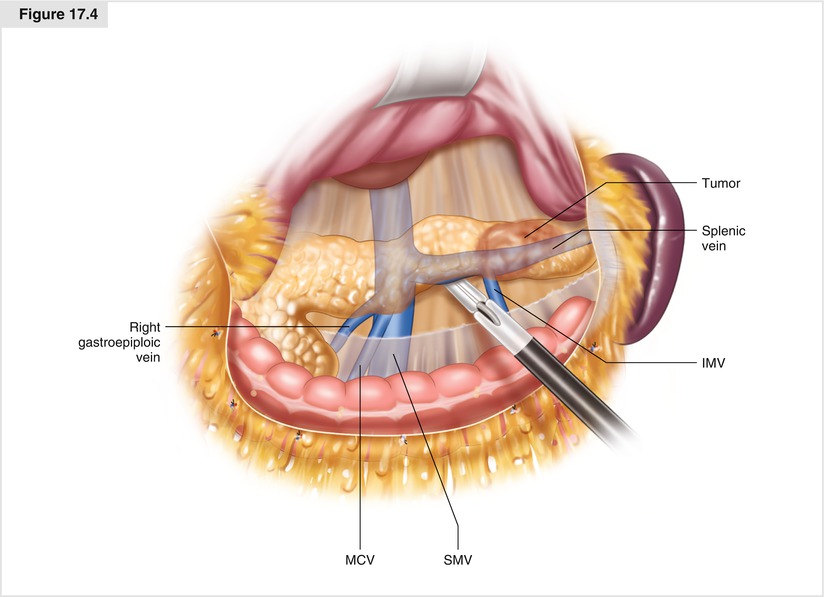
Figure 17.2
Exposure of the pancreas. With the stomach held up to the right and the omentum held inferiorly, the lesser sac is entered. With the patient in reverse Trendelenberg, the omentum and transverse colon will fall as will the greater omentum. The omentum is taken up to the level of the fundus if a splenectomy is planned, allowing the stomach to be pushed out of the field under the left lateral segment. If splenic preservation is planned, stop at the level of the short gastric arcade and retract the stomach for exposure
Figure 17.3
The peritoneum along the inferior edge of the pancreas is dissected out using an electrothermal device. It is safer to begin laterally and move medially, being careful not to go too deep and injure the inferior mesenteric vein (IMV). Dissect carefully over the region of the middle colic vein (MCV), as the superior mesenteric vein (SMV) will be right below the MCV
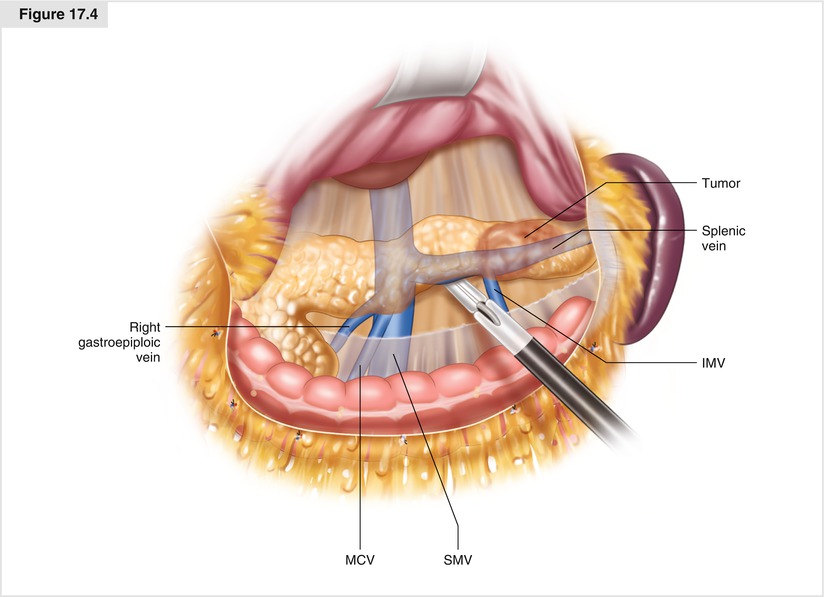
Figure 17.4
As the pancreas is exposed and freed from all attachments, critical vascular structures are identified. Dissection started inferiorly will expose the SMV by following the MCV and the right gastroepiploic vein. This maneuver also allows for exposure of the splenic vein, and it is important to confirm the anatomy before dividing any major vessels. The IMV can also be exposed as the inferior border of the pancreas is freed and transverse mesocolon is lowered. The IMV can be stapled or doubly clipped to facilitate dissection. Small branches from the splenic vein can be divided carefully with the bipolar device under direct vision. As the pancreas is freed inferiorly, dissection can continue behind the pancreas to free it from retroperitoneal attachments. Care must be taken to avoid injury to the renal vein and adrenal gland during this portion of the procedure. Moving laterally, the splenic flexure can then be freed from the spleen, and the entire pancreas is in view. This is a good time to perform intraoperative ultrasound if necessary
Figure 17.5




The top of the pancreas is freed from its attachments, taking great care to locate the splenic artery. Referring to the prior CT can confirm the artery’s location, or intraoperative ultrasound can be used. It is critical to confirm celiac axis anatomy and its branches before any vessels are divided
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree