Fig. 13.1
Patient positioning
A bean bag and an overlying gel pad are prepositioned on the operating table.
The patient is positioned on the operating table so that the anterior superior iliac spine lies just inferior to the break of the table.
Patient is positioned in left lateral decubitus position. The trough supporting the right arm is positioned so as to allow the right arm to fall forward. An axillary roll is placed and all areas are appropriately padded and secured.
The table is raised and flexed so as to open the intercostal spaces and the subcostal spaces and rotate the hips down and away from the horizontal position.
The bean bag is desufflated with patient in this position, making sure that the patient is not rotated.
After positioning, repeat bronchoscopy is performed to confirm the location of endotracheal tube. The right lung is clamped and single-lung ventilation is begun.
Thoracoscopic Dissection (Video 13.1)
Port Placement (Fig. 13.2)
Access: In most patients, two five and two twelve mm ports are necessary to perform the thoracic esophageal dissection. After desufflating the right lung, a 5 mm Optiview trocar with a 5 mm, 0° laparoscope is used to gain access and inserted under direct vision just inferior to the tip of the scapula. It is important that this port is placed about equidistant between the sternum and the vertebral bodies. This serves as the camera port. The chest is insufflated to a pressure of 8 mmHg. The camera is subsequently switched to a 5 mm, 30° scope after safe entry into the right pleural space is confirmed.
A 5 mm port is then placed anteriorly in the seventh intercostal space. This port is utilized to retract the lung anteriorly during the initial dissection. If a 5 mm fan retractor is not available, a 12 mm port can be placed for a larger fan retractor. During the latter parts of the dissection, this port can be used by the assistant to help with the high thoracic dissection.
A 12 mm port is inserted in the tenth intercostal space just above the diaphragmatic insertion in a straight line beneath the camera port.
A 5 mm port is inserted in the seventh intercostal space midway between the inferior 12 mm and 5 mm camera ports. This along with the 12 mm port is used as the surgeon’s working ports. It is critical that these two ports are not placed too posteriorly so that interference with the vertebral bodies is encountered.
Dissection
5 mm fan retractor is used to retract the lung anteriorly, exposing the esophagus. If a 5 mm fan is not available or adequate, this can be enlarged to a 12 mm port.
Dissection is begun by dividing the inferior pulmonary ligament to the level of inferior pulmonary vein.
The goal is to encircle the lower esophagus with a Penrose drain and to widely dissect the periesophageal tissue free from the posterior mediastinum. To accomplish this, the periesophageal tissue is widely opened anteriorly and posteriorly to the lower esophagus using the ENSEAL® tissue sealing device (Ethicon Endo-Surgery, Inc., Cincinnati, OH), carefully preserving the inferior pulmonary vein and avoiding entry into the pericardium and left pleural space.
The esophagus is encircled carefully using a RealizeTM (Ethicon Endo-Surgery, Inc., Cincinnati, OH) dissector and a ¼-in. penrose is placed around the esophagus, and the ends are secured with an endoloop tie as shown in Fig. 13.3. It is critical to have a 2-0 silk tie sutured to one end of the penrose and a small loop fashioned in the suture that can be attached to the RealizeTM and subsequently pulled around the esophagus. The penrose is left slightly loose so as to allow its movement along the length of the esophagus.
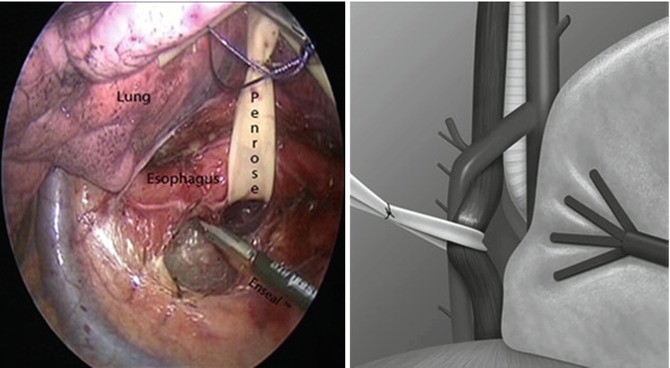
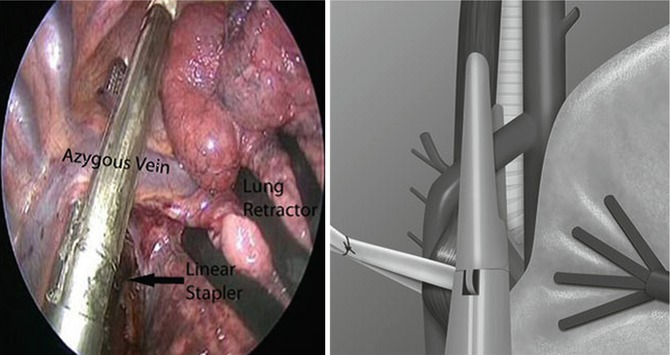
Fig. 13.3
Thoracoscopic mobilization of the esophagus (From Hochwald and Ben-David [1] with permission)
Both limbs of the penrose drain are grasped, and the esophagus is widely dissected from distal to proximal in the right chest. Periesophageal lymph nodes are left on the specimen. The vagus nerves are divided. The dissection is carried superiorly toward the azygous vein. The subcarinal lymph node packet is carefully dissected while preserving the membranous portions of the mainstem bronchi.
During dissection of the lower esophagus from the inferior pulmonary ligament to the level of the azygous vein, it is critical to apply a generous amount of clips to the tissue between the aorta and the vertebral bodies and the esophagus. If the thoracic duct is visualized, it is ligated, otherwise, multiple clips are applied in this area to prevent injury to the thoracic duct or its branches.
A window is made superior to the azygous vein and it is divided using a 45- or 60-mm vascular cartridge of the powered ECHELON FLEXTM ENDOPATH® stapler (Ethicon Endo-Surgery, Inc., Cincinnati, OH). Frequently the staple line on the azygous vein should be reinforced with titanium clips if there is any evidence of bleeding (Fig. 13.4).
Dissection is carried superiorly to the azygous vein, and an attempt is made to stay close to the esophagus above the azygous vein to avoid injury to the recurrent laryngeal nerve (RLN).
We make an attempt to complete the cervical esophageal mobilization through the thoracoscopic phase of the operation. Excellent visibility afforded by high-definition imaging and long instruments helps us accomplish this routinely. However, we try to minimize the use of energy devices on the tissue between the esophagus and the trachea to avoid injury to the RLN. The dissection is carried under the subclavian vessels up to the level of the clavicle.
After the cervical esophagus is mobilized at a point superior to the thoracic inlet, we proceed with dissection toward the GE junction and care is taken to ensure that the esophagus is mobilized down to the diaphragm. However, it is important not to dissect into the abdominal cavity.
After the esophageal mobilization is complete, the ¼-in. penrose is left in the superior apex of our dissection. The penrose should be above the subclavian vessels – in close proximity to the clavicle to ensure that the cervical esophageal dissection has been completed.
Hemostasis is ensured and a 24 F Blake drain is left posteriorly in the thoracic cavity and brought out through the 12 mm port site, and a purse-string suture is used to secure it to the skin. This drain is connected to a pleuravac.
The right lung is insufflated under direct vision and the port sites are closed with 4-0 Monocryl and Dermabond is applied.
Repositioning
The chest tube is connected to −20 mmHg of wall suction.
To recruit atelectatic right lung segments, the patient is put on dual lung ventilation with a PEEP set to 8 mmHg.
The patient is placed supine and the left arm is tucked. A shoulder roll is inserted under the shoulder blades to optimize cervical exposure.
The head is extended and tilted slightly to the right.
The patient is placed supine on the operating table. Split-leg tables or stirrups are not used. A footboard is placed to facilitate steep reverse Trendelenburg position during the abdominal dissection.
Cervical Dissection (Video 13.2)
A 6 cm skin incision is made along the anterior border of sternocleidomastoid starting from the suprasternal notch.
The platysma is divided.
Sternocleidomastoid muscle is identified and moved laterally, carefully ligating and dividing any crossing jugular vein branches.
A self-retaining retractor is used to facilitate further dissection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree