Fig. 12.1
Abdominal trocar placement
Abdominal Dissection
The gastrohepatic ligament is divided. The dissection is continued to the right crus up toward the phrenoesophageal ligament and across the diaphragm to the left crus. A retrogastric tunnel is created by incising the tissue along the right crus of the diaphragm. Care is taken to visualize the left crus posteriorly and place a blunt grasper behind the gastroesophageal junction (GEJ) from right to left just inferior to the crura. The blunt grasper is visualized as it exits the loose connective alveolar tissue at the angle of His. A Penrose drain is placed around the gastroesophageal junction. The Penrose is secured around the GE junction with an endo-loop.
Following this portion, the operating surgeon grasps the anterior aspect of the stomach, and the lesser sac is entered about halfway up the greater curvature of the stomach. A tissue sealing device is utilized to divide the gastrocolic omentum and short gastric vessels. Great care is taken to preserve the right gastroepiploic vessels (Fig. 12.2). The stomach is mobilized all the way until the left crus and Penrose drain are visualized at the angle of His. Mobilization of the lower half of the greater curvature of the stomach is created between the right transverse colon and the right gastroepiploic vessels. The gastropancreatic folds are divided inferiorly and the stomach is mobilized away from the pancreas until the gastroduodenal artery is visualized. The surgeon on the right side of the table mobilizes the first and second portions of the duodenum along the superior aspect of the duodenum until the common bile duct is reached. Adhesions between the first portion of the duodenum to the liver, gallbladder, or porta hepatis are carefully divided. A formal Kocher maneuver is often not necessary for an intrathoracic esophagogastric anastomosis.
Fig. 12.2
Division of the gastrocolic omentum
The right gastric artery along the superior aspect of the lesser curvature of the stomach is divided with a laparoscopic sealing device. The lesser curvature of the stomach is elevated. The surgeon skeletonizes the left gastric artery and vein at their base to assure an extensive lymphadenectomy is achieved. Subsequently, the left gastric artery and vein are stapled and divided with a vascular load. The lymphadenectomy dissection is continued along the common hepatic artery, splenic artery, and superior portion of the pancreas toward the left crus (Fig. 12.3).
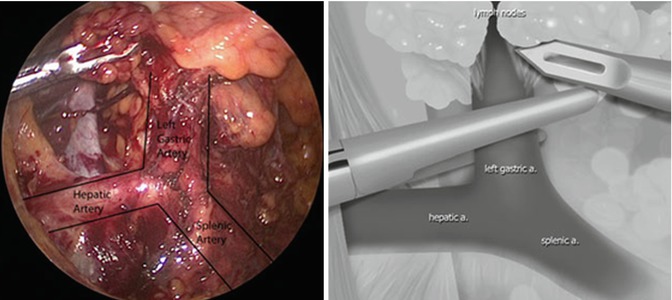
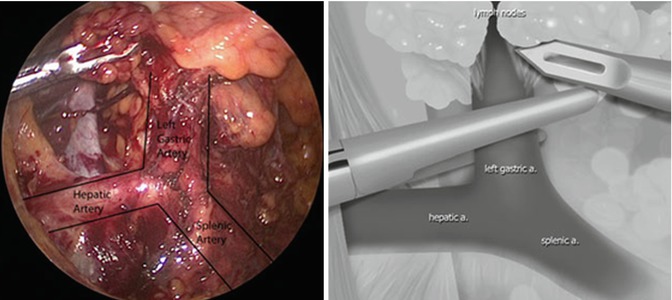
Fig. 12.3
Skeletonization and division of left gastric artery and vein (From Hochwald and Ben-David [16] with permission)
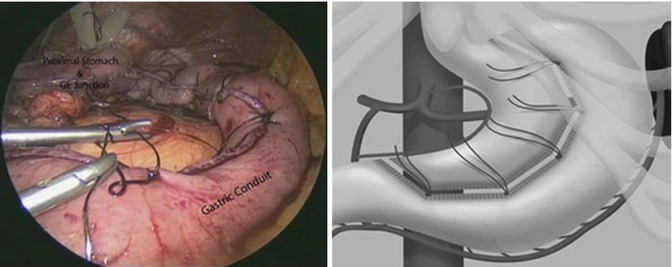
The gastric conduit is created by a series of laparoscopic stapler firings along the lesser curvature of the stomach. The nasogastric tube is pulled back above the gastroesophageal junction. The first firing is done via the right upper abdominal 12 mm port. The stapler is introduced onto the stomach 4 cm proximal to the pylorus along the lesser curvature of the stomach just proximal to the divided right gastric vessels. The stapler firings continue along the body and fundus of the stomach. The final division of the stomach is not done until after each staple line is reinforced with a single interrupted inverting suture of 2-0 silk. These sutures are placed at the junction of the staple lines and are used as handles for subsequent transfer of the stomach to the posterior mediastinum into the right chest (Fig. 12.4).
Following the final application of the stapler and division of the gastric conduit from the proximal stomach and GEJ, the esophagus is further mobilized. The Penrose drain is pulled laterally and medially enabling mobilization of the distal esophagus through the hiatus into the posterior mediastinum. The lower esophagus is widely dissected incorporating all lymphatic tissue. Subsequently, the gastric tube is sutured to the lesser curvature side of the upper divided stomach utilizing two interrupted 2-0 silk sutures.
The Penrose is placed through the hiatus into the posterior mediastinum while maintaining appropriate orientation of the gastric conduit to prevent organoaxial rotation of the gastric tube when it is being pulled into the right chest cavity. This is done by aligning the sutures placed along the lesser curvature of the stomach and straightening the gastric tube. A 16-French feeding tube is inserted into the proximal jejunum as we have previously described [11]. The port site incisions and liver retractor incision are sutured closed and dressed appropriately after expelling the pneumoperitoneum.
Thoracic Dissection
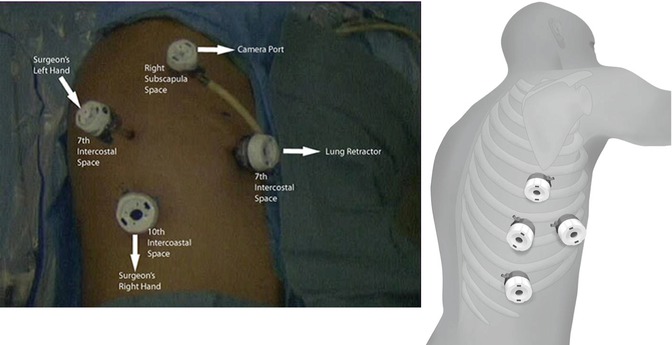
The patient is placed in the left lateral decubitus position ensuring that all of their bony prominences are well padded. The right lung is deflated and a 5-mm trocar is placed under direct vision using a 5-mm 0° scope just inferior to the tip of the right scapula. This serves as the camera port for the duration of the case, and the scope is switched to a 5 mm 30° scope. The right chest cavity is insufflated with 8 mmHg of carbon dioxide (CO2) pressure. This allows for further lung collapse during the thoracic portion of the procedure. A 5-mm port is placed in the seventh intercostal space along the posterior axillary line. A 12-mm trocar is placed in the tenth intercostal space just above the diaphragmatic insertion slightly anterior to the vertebral bodies. A 12-mm port is placed anteriorly in the seventh intercostal space and is utilized for the lung retractor (Fig. 12.5).
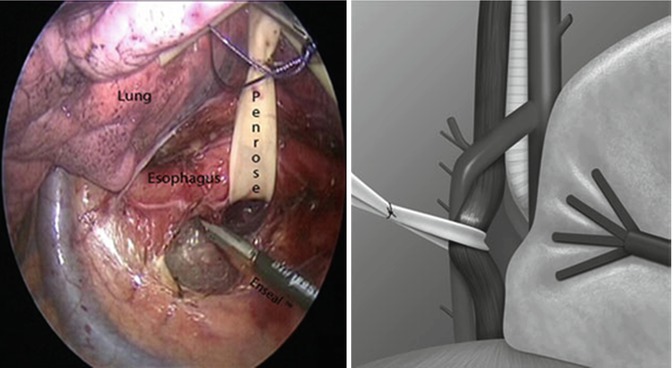
The lung is retracted anteriorly. The inferior pulmonary ligament is divided. The lower esophagus is widely dissected with an ENSEAL® tissue sealing device (Ethicon Endo-Surgery, Inc., Cincinnati, OH), and the Penrose drain is identified in the posterior mediastinum from our previous abdominal dissection. Care is taken not to enter into the left pleural space during this portion of the dissection. The esophagus is mobilized from its distal end to the level of the azygos vein. The Penrose is advanced along the esophagus during this dissection (Fig. 12.6). Periesophageal and subcarinal lymph nodes are included with the specimen. If the thoracic duct is identified, it is suture ligated or clipped. The azygous vein is divided with a 45- or 60-mm vascular load stapler (Fig. 12.7). The dissection continues with mobilization of the proximal esophagus away from the trachea. It is important to continue the esophageal mobilization just distal to the thoracic inlet.
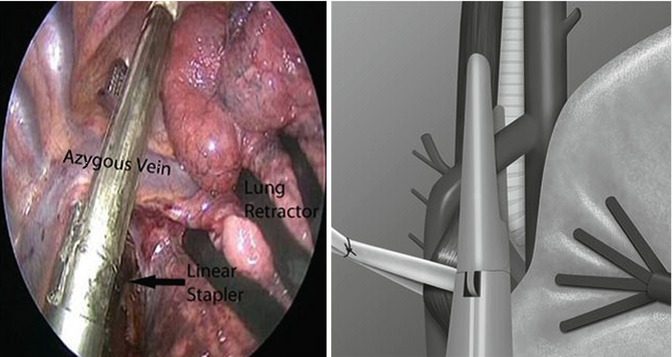
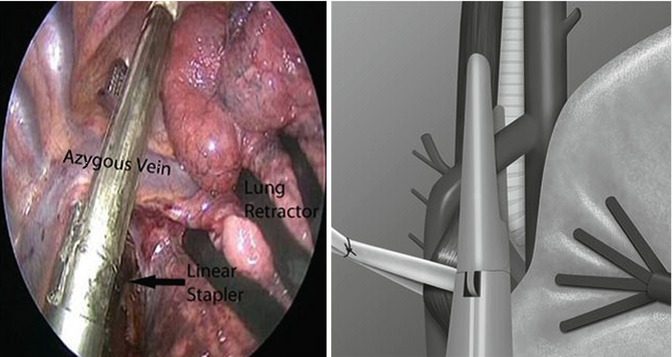
Fig. 12.7




Division of azygous vein (From Hochwald and Ben-David [16] with permission)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree