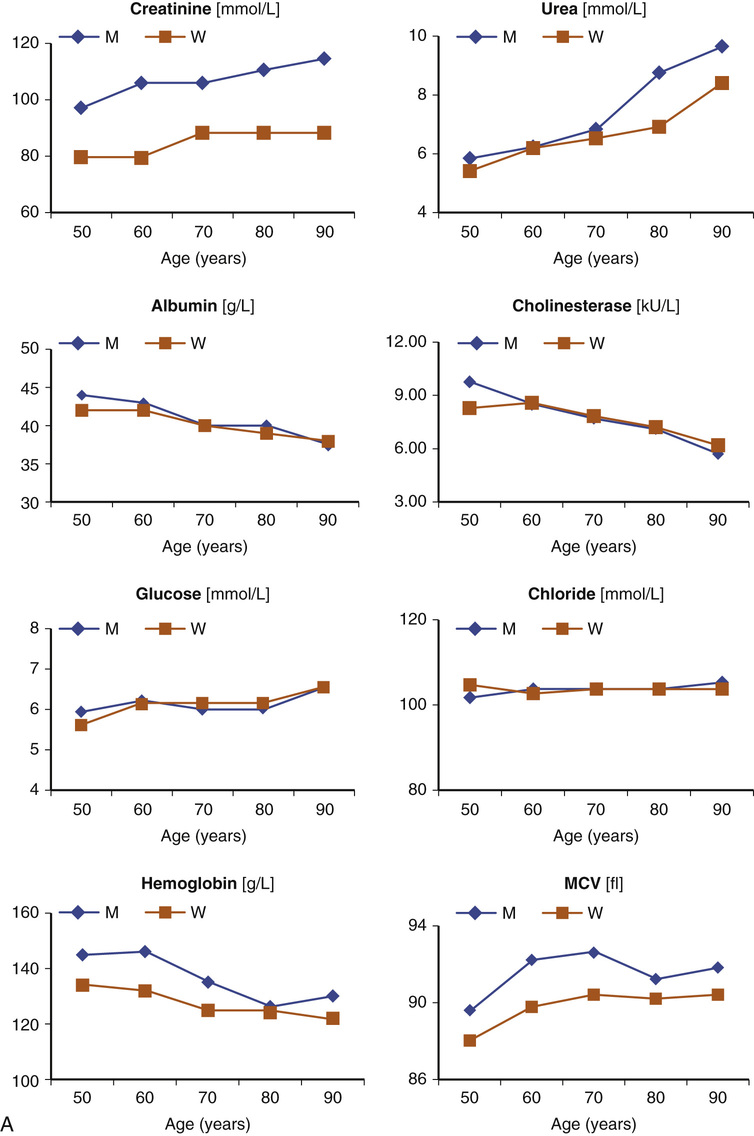
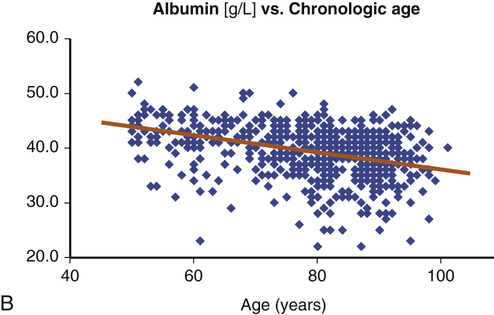
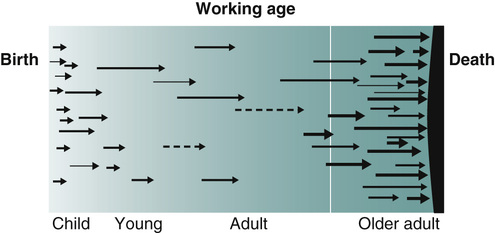
Alexander Lapin, Elisabeth Mueller Radical improvements in health care and general lifestyle have brought about longer life expectancy and, with it, a demographic phenomenon that has never been observed before. The steady growth of the proportion of older adults in the general population, especially in industrialized countries, has resulted in what is called an inverse demographic pyramid. Concurrently, the subject of geriatric medicine has also gained in popularity, both among the members of the professional community and in the general public, but not so in laboratory medicine. Here, except for an occasional call to adjust the reference intervals for specific tests, there has been no fundamental discussion of the consequences of the current demographic trend in the population—that is, until now. This chapter should provide some insights into this problem. Since antiquity, the in vitro diagnosis has followed the same principle. A biologic sample such as blood or urine collected from the patient would be analyzed for its physical and/or chemical properties, and the result would then be interpreted in terms of clinical information indicating the health status of the patient. If the procedure is properly calibrated, the results can be expressed quantitatively and described not in words, as is the case for other diagnostic disciplines, such as pathology or radiology, but as an exact numeric value. Thus, the result of a laboratory analysis is not a descriptive observation derived from a subjective experience of the operator, but is an objective measurement, which always is related to a deductive postulated standard. Because most of the results provided by laboratory investigations can be considered as data that are generally reproducible and comparable, laboratory analysis represents a valid instrument of modern, evidence-based medicine. To keep the clinical interpretation of these data objective, as much as possible, every numeric test result is usually completed by a reference interval, which is listed on the same line next to the test result value. The reference intervals have been derived from the standard statistical distribution of test results obtained from a demographic sample drawn from the normal adult population; normal is understood to be synonymous with healthy.1 However, because the statistical reference interval is based on the 95th percentile of Gaussian normal distribution (the bell curve), 5% of results obtained from healthy individuals will always be outside the reference range yet have no pathologic correlation. It follows that even in the case of a healthy individual, the probability that a random test result value would fall outside the reference interval proportionally increases with the number of the same laboratory tests performed on that same healthy individual. Thus, ironically, the larger the number of tests undertaken, the higher the probability of a patient not being found normal,1 which shows that the statistically based reference concept2 has its limits. Every person is not just an anonymous member of a collective, but a unique unrepeatable individual. You cannot step twice into the same rivers. Attributed to Heraclitus From the point of view of the sociology, the answer to the question whether an older adult is healthy or sick can neither be based on actual performance at work nor reduced to the fact of whether he or she has secured a physician’s note from the employer. By contrast, in older adults, more than in younger adults, the difference between being healthy or sick is based on a very subjective feeling reflecting the quality of one’s life. However, there is yet another aspect to be considered in geriatric laboratory medicine. It is the continuous progressive decline of physiologic functions in an aging human body. Age-dependent impairment of renal and pulmonic functions, progression of osteoporosis, decrease of various endocrine functions, and general weakening of immunity at an older age are typical examples.3–6 Attempts to establish age-related reference intervals, similar to those used in pediatrics, have proven to be unsuccessful. Such intentions failed because the approach did not and could not address the individuality and variability of the senescent process from the clinical and biologic point of view for each patient (Figure 35-1). In pediatrics, as well as in the adult medicine, most of the population is healthy, and those who are sick usually have only one cause (rarely more than one) for their illness. The primary aim of pediatric and adult medicine is to detect and cure the disease as efficiently as possible to protect the future life chances of the patients. Adult medicine strives to return adult patients to their normal productive (working) life as quickly as possible. Geriatrics is different. Here, the clinical histories of older adults who have reached the last part of their lives are much more complex than those in the previous stages of their life. Past crises and emergency situations, but also periods of prosperity and affluence—perceived as the good times—all have influenced the actual health state of an older adult. Diseases and trauma, which randomly occur in the course of life and have left more or less relevant after effects and physical and emotional scars in all of us, contribute to the specificity of the clinical status of each older adult. Moreover, with advancing age, the probability of manifestation of genetically or secondarily predisposed diseases increases progressively. To describe all these inputs, clinical geriatrics uses the term multimorbidity. It is a very important term because it characterizes the occurrence of several diseases and/or pathologic processes to which an older patient is subjected, often in oligosymptomatic and atypical ways. Many different involute processes can be considered as typical physiologic processes of older age. They all can occur with individual accentuation and can be triggered by different random events at different moments of the life. In this context, it becomes more and more difficult to define unequivocally the meaning of the term biologic age.7 Finally, one has to accept that death itself is often a result of one or more diseases breaking out during the ultimate period of life (Figure 35-2). To sum up, when speaking about the normality of patients in geriatrics, it has to be kept in mind that an older, perfectly healthy individual is a biologic rarity, rather than the normal case.8 The opinion that geriatric reference intervals can be estimated by large-scale studies seems to be spurious, even from a theoretical point of view. According to Harris,9 the width of the reference interval is determined by three types of variation, which can be characterized by appropriate coefficients of variation, CV: • CVA—analytic variation, due to the imprecision of an analytic method • CVB—biologic variation, accounting for variations within one individual • CVC—interindividual variation, due to differences among several individuals The total variation (CVTOT) results from the geometric sum of these three variations: In practice, it can be assumed that the analytic variation (CVA) is almost negligible due to the high technical standards of the analytic method. Hence, the total reference interval (CVTOT) is determined by the biologic (CVB) and the interindividual (CVC) variations alone. There are two extreme cases to be considered (Figure 35-3): 1. In the first case, the reference interval of a parameter is almost identical with the biologic variation (CVB) that is nearly the same in all healthy individuals—that is, CVC → 0 (e.g., glucose).
Laboratory Diagnosis and Geriatrics
More Than Just Reference Intervals for Older Adults
Introduction
Objectivity as a Basic Principle of In Vitro Diagnosis
Geriatric Individuality
From Screening to Monitoring
Should a particular individual disease break out, the probability that the corresponding value will be shifted out of the reference range increases. In such conditions, the pathology would be detected early, and the probability to obtain a result outside the reference interval would be increased by repeating the test (see Figure 35-3).
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Laboratory Diagnosis and Geriatrics
35