of the patient. Nevertheless, as demonstrated by the Schiavo case, public acceptance of these distinguishing features in nutritional support varies greatly. Furthermore, some faith communities take issue with the distinction between artificial and basic nutrition (proposition 52).
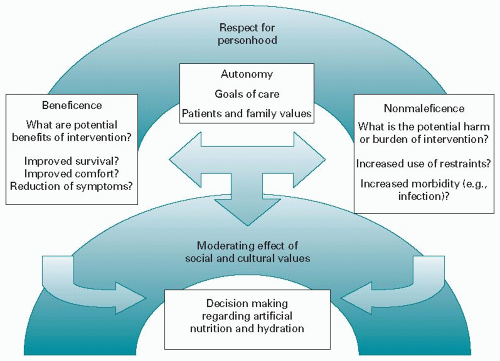 Figure 60.2. Integration of ethical principles into decision making regarding artificial nutrition and hydration. |
TABLE 60.1 American Gastroenterological Association guidelines on enteral feeding | ||
|---|---|---|
|
(age >50 yr) adults referred to a community gastroenterology group for PEG insertion over a 10-year period, mortality rates at 1, 2, and 3 years were 54.3%, 73.2%, and 84.5%, respectively. Like Rabeneck’s study, the overall median survival was between 6 months and 1 year; however, those receiving tube feeding in this cohort were much more likely to be patients with stroke or other neurologic conditions. Very few of the PEGs were placed in patients with cancer. Risk factors for mortality in this cohort were being male, having feeding difficulty, having diabetes, being referred from a hospital, and being 80 years of age or greater (18). Similar to Grant’s cohort, dementia was not an independent risk factor for decreased survival. Because these studies used large databases, identification of truly comparable control groups would have been challenging. Nevertheless, because there was no comparable control group, the impact of gastrostomies on survival could not be ascertained.
TABLE 60.2 Levels of evidence for artificial nutrition | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
hunger during the first quarter of their course in the unit. In all patients reporting either hunger or thirst, these symptoms were consistently and completely relieved by oral care or the ingestion of small amounts of food and fluid. In a case study of a patient refusing nutrition and hydration, the patient experienced no discomfort and died peacefully (19). A survey of Oregon hospice nurses found that among those who had cared for patients who declined nutrition and hydration, the majority reported the ensuing death to be peaceful (20).
TABLE 60.3 Recommendation classifications and levels of evidence | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree