16 Intraoperative Radiation Therapy
Intraoperative irradiation therapy (IORT) in its broadest sense refers to the delivery of irradiation at the time of an operation. This can involve the use of electrons (intraoperative electron irradiation therapy; IOERT), high dose rate brachytherapy (HDR-IORT) or orthovoltage (used by select institutions) in conjunction with surgical exploration and resection with or without external beam irradiation therapy (EBRT) and chemotherapy. IORT evolved as an attempt to achieve higher effective doses of irradiation while dose-limiting structures are surgically displaced.1–4
Rationale for Intraoperative Irradiation
Influence of Dose on Local Control
In many animal experiments, local tumor control increases sharply with increasing irradiation dose, and the shape of the curve closely follows the theoretical model.5 The animal data also show that the irradiation dose needed to control a certain percentage of tumors will increase as the tumor volume increases and, conversely, that the percentage of tumors that will be controlled at a certain dose level will decrease as the volume of the tumor increases. Although a given irradiation dose may be able to control a small tumor mass with high probability and acceptable morbidity, that same dose may be ineffective against larger volume tumors that contain a larger number of clonogenic cells.
Fletcher and colleagues6 performed an extensive evaluation of dose–response curves of human tumors emphasizing adenocarcinoma of the breast and squamous cell carcinomas (SCCs) of the head and neck. In breast cancer, the probability of controlling subclinical nodal or chest wall disease was 60% to 70% with a dose of 30 to 35 Gray (Gy), 85% with 40 Gy, and 95% with 45 to 50 Gy (the usual fractionation was 10 Gy per week in 2.0-Gy fractions). For locally advanced breast cancers, LC required much higher doses. For these large tumors, 70% LC was achieved with doses of 90 Gy (with protracted fraction) by Fletcher6 versus 35% LC with doses of 50 to 60 Gy in the series of Griscom and Wang.7
The most extensive information on LC versus dose exists for SCCs of the head and neck. These data have been summarized by Fletcher and Shukovsky6 and Tepper.8 For microscopic disease in lymph nodes, a dose of 30 to 40 Gy produces LC in 60% to 70% of patients, compared to greater than 90% control at doses of 50 Gy in 25 fractions over 5 weeks. For early-stage primary tumors of the head and neck, a strong dose–response curve has not been demonstrated, because of good control at virtually all doses commonly used. Data compiled by Tepper for higher stage tumors indicate that 20% LC results after a dose of 46 Gy, 50% control with 58.5 Gy, and 80% control only with a very high dose of 75.5 Gy. Thus, a marked improvement in LC results from the ability to increase the tumor dose significantly.
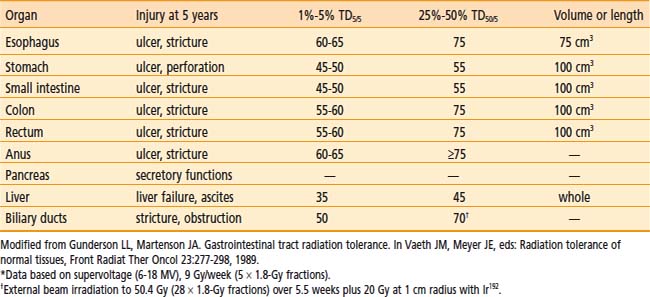
Local Tumor Control versus Complications
For patients with locally advanced abdominal or pelvic malignancies in whom all disease cannot be removed surgically with negative margins, EBRT (with or without chemotherapy) is often only palliative, because doses greater than 45 to 50 Gy in 25 to 28 fractions cannot be delivered safely. Gastrointestinal tolerance to fractionated EBRT is demonstrated in Table 16-1.9 If treated with tolerable doses, patients often have local persistence or relapse of disease with secondary complications that may require hospitalization and/or reoperation for small bowel obstruction, ureteral obstruction, bowel perforation, and so on.
Impact of Local Control on Distant Metastases
In the ASTRO Gold Medal paper of Dr. Herman Suit,10 the theme of distant metastases developing from a locally recurrent tumor was discussed as a component of the overall premise that LC benefits survival. Data were presented from several spontaneous tumor systems to suggest that the rate of distant metastases was related to both tumor size and disease presentation as primary versus locally recurrent disease. In both the spontaneous fibrosarcoma FSaII and SCC VII lines in the C3H/Sed mouse, Ramsey et al. reported increased rates of distant metastases with 6-mm versus 12-mm tumor size and primary versus recurrent tumors.11 Ramsey’s work confirmed an earlier evaluation by Suit et al.12 in which 12-mm isotransplants of C3H mouse mammary tumors were treated with single-dose irradiation and evaluated for disease control both locally and distantly. The rate of distant metastases increased with lack of LC. The incidence of distant metastases was 31% (16 of 52) in mice with LC, 50% (9 of 18) in those with local relapse who were salvaged with further resection, and 80% (12 of 15) in mice with local relapse in whom salvage was not attempted.
Human data were also quoted to support the thesis of metastases arising from the local relapse. For patients with squamous cell cancers of the cervix, prostate, and head and neck cancers, the metastatic frequency was higher in patients with local relapse than in those with LC.13–16
Treatment Issues: Sequencing, Irradiation Dose, and Technique
Technique and Dose: IORT
The technical aspects of both the surgical and irradiation components of IORT procedures have been discussed in detail in previous publications1–3 and will not be reiterated in detail. A carefully constructed team including surgeons, radiation oncologists, anesthesiologists, operating room nursing staff, radiation physics and dosimetry staff, and radiation therapists must jointly oversee IORT procedures.
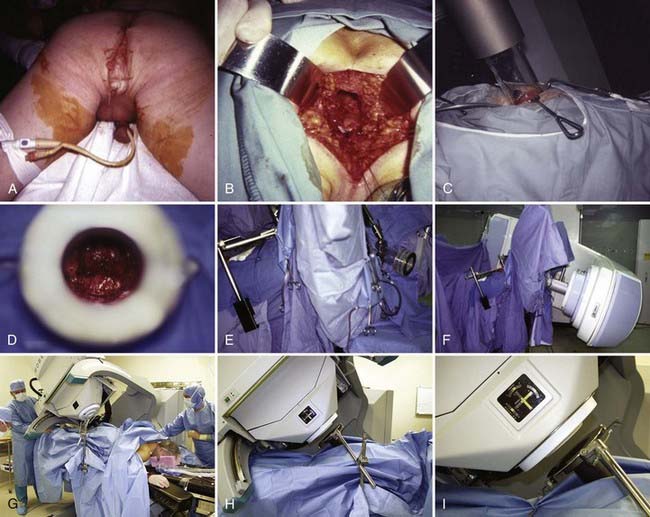
Following surgical exploration and maximal resection, the radiation oncologist joins the surgeon in the operating room to determine whether IORT is indicated and technically feasible, based on a review of surgical-pathologic findings. The site of the IORT treatment field is determined and marked with sutures or clips. If the IORT treatment machine is in the radiation oncology department, the patient will then be transferred to a stretcher for transport after temporary closure of incisions, and placed on the linear accelerator table in the radiation oncology department for IOERT treatment. If the institution has a mobile X-band accelerator (Mobetron, electron energies of 4 to 12 MeV) that can be brought to the operating room, the IOERT applicator is immobilized in position with a modified Buchwalter retractor after the applicator size and shape has been selected to encompass the tumor bed or unresected disease with a margin of ∼1 cm (Fig. 16-1A-F). The operating room table is then shifted adjacent to the IOERT machine and the gantry angle of the mobile accelerator is adjusted to provide alignment between the IOERT applicator and the accelerator head (Fig. 16-1G-I). The IORT team exits the room and IOERT is delivered while the patient and anesthesia equipment are monitored. The operating room table is then shifted back to the original location for surgical reconstruction and closure of incisions.
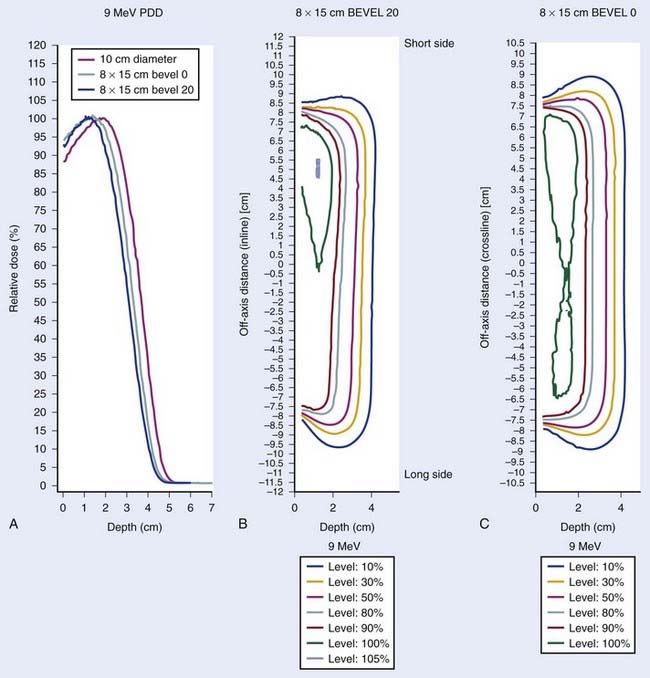
The IOERT energy and dose are dependent on the amount of residual disease remaining after maximal resection and on the EBRT component that is feasible (Figs. 16-2 and 16-3). When an R0 or R1 resection has been accomplished, 6 or 9 MeV electrons would provide adequate depth dose, but for R2 resection or unresectable disease, 9- to 12-MeV electron energies or higher would be necessary to ensure adequate depth dose coverage (Fig. 16-2). If previously unirradiated patients have received preoperative doses of 45 to 54 Gy (1.8-Gy fractions 5 days per week), the IORT dose usually varies from 10 to 20 Gy: microscopic residual disease or less, 10 to 12.5 Gy; gross residual disease, 15 to 20 Gy. In previously irradiated patients, the IORT dose is usually 15 to 20 Gy if EBRT doses of 20 to 30 Gy can safely be given pre- or postoperatively. IORT doses of 25 to 30 Gy have been given to patients in whom no or limited EBRT is planned, but such doses have higher risks of nerve intolerance. The biologic effectiveness of single-dose IORT is considered equivalent to 1.5 to 2.5 times the same total dose of fractionated EBRT.17 The effective dose in the IOERT field, when added to 45 to 50 Gy given with EBRT, is 60 to 70 Gy for 10-Gy IOERT, 75 to 87.5 Gy with a 15-Gy boost, and 85 to 100 Gy with 20-Gy IOERT.
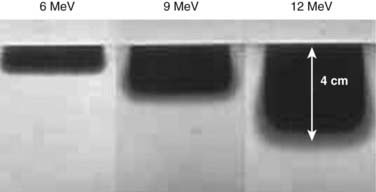
FIGURE 16-2 • Depth dose of 6, 9, and 12 MeV electrons with nonbevel applicator on the Mobetron mobile accelerator using film measurements.
IORT is given with IOERT, HDR-IORT, or orthovoltage machines, depending on institutional preference and available technology. Some institutions have both IOERT and HDR-IORT equipment and choose which to use according to anatomical constraints and amount of residual disease after maximal resection (i.e., HDR-IORT is not ideal if thickness of residual disease exceeds 0.5 cm).4 If both are technically feasible, IOERT is often chosen because of shorter set-up and treatment times, better depth dose, and more homogeneous dose distribution. Since IOERT is delivered with rigid Lucite or metal applicators, some locations may be anatomically challenging, and HDR-IORT with malleable flab applicators may be preferable, if available.
In IOERT only institutions that have a wide variety of applicators including 15° and 30° beveled ends (Fig. 16-1A,B), the combination of applicator choice and patient position can usually result in a successful treatment. Most abdominal sites are usually easily treated with IOERT approaches using either flat or 15° bevel applicators (Fig. 16-1C-F). For pelvic lesions, the availability of 30° bevel applicators usually allows successful approximation of the IOERT applicator to the tumor bed whether treated through the abdominal incision (Fig. 16-4) or the perineal incision after abdominal-perineal resection (Fig. 16-5).
Dose-Limiting Structures and IORT Tolerance
In patients with locally advanced malignancies, the issue of morbidity following aggressive treatment that includes IORT is placed into clearer perspective by a comparison with tumor-related morbidity.18–34 For instance, when EBRT is used as the main treatment modality for locally advanced rectal cancers, more than 90% of patients have local relapse or persistence of disease and most are dead in 2 to 3 years (nearly 100% tumor-related morbidity/mortality).
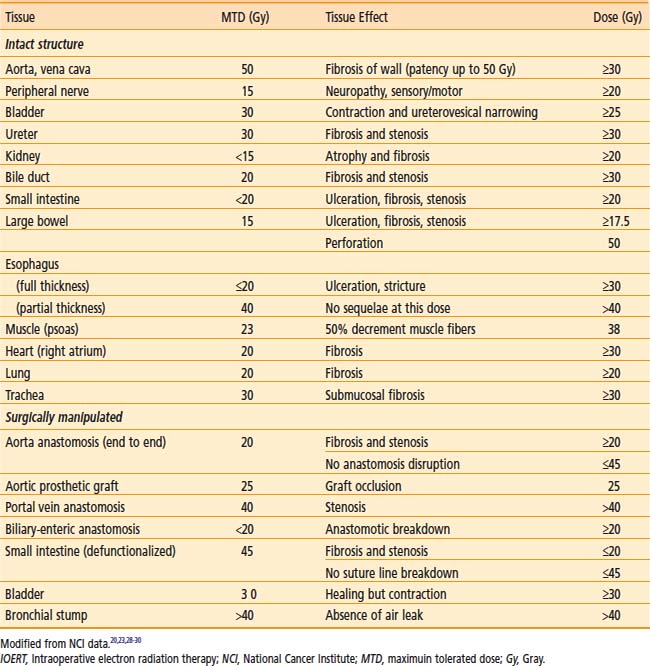
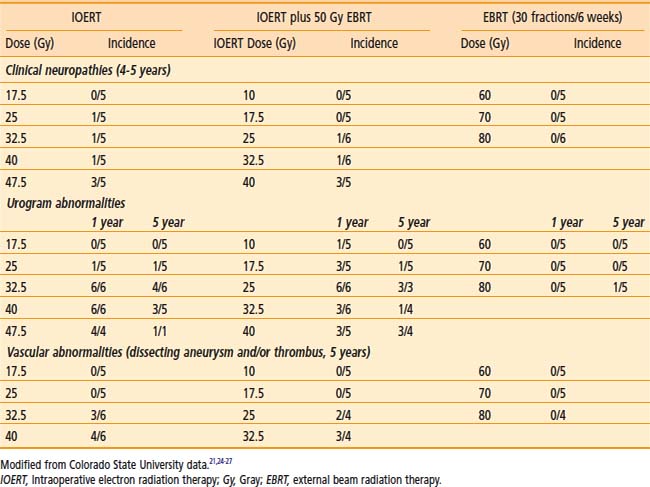
IOERT tolerance for intact or surgically manipulated organs or structures in animals is shown in Table 16-2.
Dose-sensitive structures include ureter and bile duct.20–22,26,29–31 Neither structure is dose-limiting, because stents can be inserted as indicated to overcome obstruction and preserve renal or liver function. In an early Mayo Clinic Rochester (MCR) analysis, 44% of previously unobstructed ureters became partially or totally obstructed when included in the IOERT field.22 A later MCR analysis of 146 patients in whom the ureter was within the IOERT field, found that the risk of subsequent obstruction was highest in patients receiving >15 Gy IOERT.31
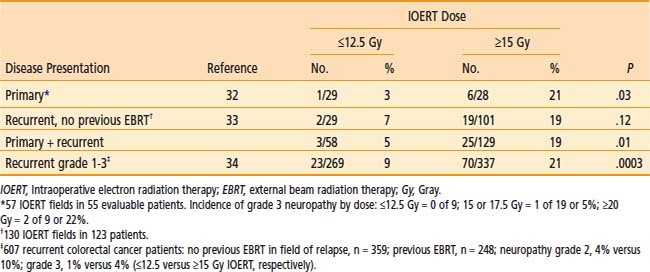
Peripheral nerve is the principal dose-limiting normal tissue for IOERT in the pelvis or retroperitoneum20–27,30,32–34 in animal studies from the National Cancer Institute (NCI) and Colorado State University (CSU) (Tables 16-2 and 16-3) and clinical analyses from MCR (Table 16-4), the NCI and other institutions. The anatomic location of peripheral nerve tissue often makes it adjacent to or involved by tumor. Even when nerve is uninvolved, it is usually impossible to move or shield nerve from the IOERT field.
An in-depth analysis of nerve and ureteral tolerance of IOERT was published on 51 patients who received IOERT at MCR as a component of treatment for the management of locally advanced primary or recurrent pelvic malignancies.22 Treatment consisted of EBRT (median 50.4 Gy), maximal resection when feasible, and an IOERT boost (range: 10 to 25 Gy) that utilized 9 to 18 MeV electrons. Fifty of the 51 were eligible for peripheral neurotoxicity analysis. Sixteen (32%) developed grade 1 to 3 peripheral neuropathy (unilateral pelvic or extremity pain, leg weakness, numbness or tingling). Pain was severe (grade 3) in only 3 (6%). Neuropathy incidence by IOERT location was as follows: pelvic sidewall 15 of 32 (47%), presacrum 1 of 12 (8%), central pelvis 0 of 6 (0%).
In MCR analyses of IOERT regimens in 187 patients with locally advanced colorectal cancer,32,33 tolerance data suggest a relationship between IOERT dose and the incidence of grade 2 or 3 neuropathy (see Table 16-4; EBRT factors appeared constant). With an IOERT dose of 10 to 12.5 Gy, the incidence of grade 2 to 3 neuropathy was 5%; with doses of ≥15 Gy, the incidence was 19% (P = .01). The incidence of grade 3 neuropathy was ∼5% in both primary and locally recurrent patients and the incidence of grade 1 to 3 neuropathy was ∼32%. This trend is consistent with animal data that suggest a correlation between IOERT dose and the incidence of clinical and electrophysiologic neuropathy in dogs.
In the most recent MCR analysis of 607 patients with locally recurrent colorectal cancer, the incidence of grade 1 to 3 neuropathy was 15% (grade 1: 32 patients [5.3%]; grade 2: 43 patients [7.1%]; grade 3: 18 patients [3.0%]; see Table 16-4).34 For IOERT doses of ≤12.5 Gy (versus ≥15 Gy), the incidence of grade 2 neuropathy was 4% (versus 10%) and the incidence of grade 3 neuropathy was 1% (versus 4%), P < .0003.
Pancreas IOERT
EBRT Plus Chemotherapy
For unresectable lesions, the use of EBRT plus concurrent 5-FU or gemzar-based chemotherapy results in a doubling of median survival rate (SR) compared with surgical bypass or stents alone (median SR: 3 to 6 months vs 9 to 13 months) and an increase in 2-year SR from 0%-5% to 10%-20%.35–39 However, 5-year SR is rare and LC is low. In a series from Thomas Jefferson University (TJUH) using EBRT doses of 60 to 70 Gy in 1.8- to 2.0-Gy fractions over 7 to 8 weeks, LC was achieved in less than 20% of patients treated with EBRT alone.35–36 With EBRT plus chemotherapy, LC was achieved in ∼30% of patients.
IORT Alone or Plus EBRT
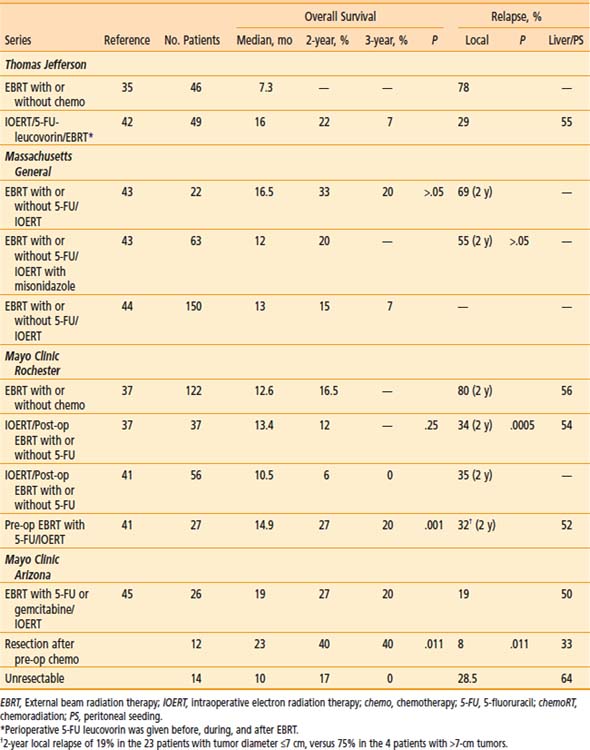
The combination of EBRT plus IOERT has resulted in an improvement in LC in IOERT series from MGH, Mayo, and TJUH37,39–45 (Table 16-5). This has not, however, translated into major improvements in either median or 2-year survival. The delivery of EBRT plus concurrent chemotherapy before restaging and laparotomy plus IOERT or resection plus IOERT translates into improved patient selection and some improvement in median and 2-year survival.41,45
Table 16-5 Pancreas: EBRT With or Without IOERT or Brachytherapy for Unresectable/Borderline Resectable Cancers
Massachusetts General Hospital
In the 1970s and 1980s, the treatment regimen at MGH was a combination of low-dose pre-op EBRT, IOERT, and high-dose post-op EBRT.40 Patients with locally unresectable disease (no distant metastases) received 10 to 15 Gy of pre-op EBRT (pancreas and nodes). If metastases were not found and the primary was unresectable, IOERT was given (15 to 20 Gy with 15 to 23 MeV). After recovery from surgery, the patient received post-op EBRT for an additional 35 to 39.6 Gy (4-field technique to clipped tumor with or without lymph nodes [LN]) in conjunction with intravenous (IV) 5-FU (500 mg/m2 for 3 days during week 1 of EBRT).
Misonidazole, a hypoxic-cell sensitizer, was combined with IOERT in a series of 41 MGH patients in an attempt to improve local tumor control; patients also received EBRT plus concurrent 5-FU.43 Outcomes were compared with those in 22 IOERT patients who did not receive misonidazole (1-year LC of 67% [versus 55%] and 2-year 45% [versus 31%], favoring misonidazole patients; P > .05). One-year overall survival (OS) was 50% (versus 77%), 2-year OS was 20% (versus 33%), and median survival was 12 months (versus 16.5 months; favoring non–misonidazole patients; P > .05). Median survival in the entire group of 63 patients was 14 months. There was a bias toward larger tumors in patients treated with misonidazole (15% of misonidazole/IOERT patients with small tumors ≤4.5 cm versus 50% in the control group of 22 patients).
In the most recent update of MGH results, 150 patients with locally unresectable pancreas cancer received IOERT as a component of treatment from 1978 to 2001 in conjunction with EBRT and 5-FU based chemotherapy.44 Long-term survival was seen in 8 patients and 5 were alive at or beyond the 5-year interval. Actuarial 1-, 2-, 3- and 5-year survival for the 150 patients was 54%, 15%, 7%, and 4%, respectively and median survival was 13 months. Survival was significantly related to the diameter of the IOERT treatment applicator (which is a surrogate for tumor size). In the 26 patients treated with a 5- or 6-cm applicator, 2- and 3-year survival were 27% and 17%, respectively; 0 of 11 patients treated with a 9-cm diameter applicator survived beyond 18 months and those treated with a 7- or 8-cm applicator had intermediate survival (P < .05).
Mayo Clinic
In the initial MCR series, IOERT usually preceded EBRT.37 When results were compared with EBRT with or without 5-FU, LC at 1 year was 82% for EBRT plus IORT with or without 5-FU (versus 48% for EBRT with or without 5-FU); at 2 years, LC for EBRT plus IORT with or without 5-FU was 66% (versus 20% for EBRT with or without 5-FU; P = .0005). This did not translate into a difference in either median or 2-year SR (median SR: 13.4 months with IOERT versus 12.6 months without; 2-year SR: 12% with IOERT versus 16.5% without). A higher percentage of patients in the non-IOERT group received concurrent 5-FU during EBRT. The lack of survival improvement was related to a high incidence of abdominal relapse in both groups (20 of 37 IOERT patients [54%] developed liver or peritoneal metastases versus 68 of 122 [56%] in non-IOERT patients).
In an attempt to improve patient selection and survival, investigators from MCR delivered the EBRT plus chemotherapy before restaging and exploration.41 In 27 patients who received IOERT after EBRT, LC was achieved in 21 of 27 (78%) with actuarial rates of 86% and 68% at 1 and 2 years, respectively. Median survival was 14.9 months with this sequence and 2 and 5 year survival were, respectively 27% and 7%. These findings were compared with results in 56 patients who had IOERT before receiving the high-dose external component at Mayo or elsewhere (median SR: 10.5 months; 2-year SR: 6%; P = .001). In an earlier analysis of 37 patients treated solely at Mayo with the latter sequence, median and 2-year survival were, respectively, 13.6 months and 12%. Although 2-year SR appeared to improve with the altered sequence of pre-op treatment followed by IOERT, this was likely due to altered patient selection, because the rate of liver plus peritoneal failure did not change (14 of 27 at risk [52%]).
Investigators from Mayo Clinic Arizona have used only the sequence of pre-op chemoradiation (chemoRT) followed by restaging, surgical exploration with resection/IOERT, as indicated, for select patients with borderline resectable or unresectable pancreas cancer.45 A series of 26 patients with no previous treatment have received IOERT after pre-op chemoRT; resection was performed in 12 of 26 patients before IOERT (R0 or R1 = 9; R2 = 3). Median SR for the total group was 19 months; 2-year OS was 27%; 3-year OS was 20% (see Table 16-5). Survival outcomes appeared to be improved in patients with resection after pre-op chemoRT versus those without resection (median survival: 23 months versus 10 months; 2-year OS: 40% versus 17%; 3-year OS: 40% versus 0%; P = .011, log-rank). Liver or peritoneal relapse has been documented in 13 of 26 patients (50%).
European Pooled Analysis
A pooled analysis of 270 patients from five European Institutions was presented at International Society of Intraoperative Radiation Therapy (ISIORT) 2008 by Valentini et al.46 Radical surgery was performed in 247 cases (91.5%; R0 resection: 53.4%; R1: 27.4%; R2: 19.2%) and exploratory laparotomy in 8.5%. Surgery was preceded by EBRT in 63 patients (concurrent chemotherapy in 38%) and 106 received post-op ERBT (concurrent chemotherapy in only 7.5%). Median OS was 19 months for the total group of patients and 5-year OS was 17.7%. Survival and LC appeared better in patients treated with pre-op EBRT/chemoRT compared to post-op EBRT (or chemoRT) or IORT alone (median OS: 30 months, 22 months, and 13 months, respectively; median LC: not reached, 28 months, and 8 months, respectively). On multivariate analysis, nodal status and timing of EBRT significantly affected survival. In the subset of patients who remained free from local relapse for more than 2 years, 3-year and 5-year OS were 32% and 28% (versus 12% and 0% in patients with local relapse within 2 years).
Gastric IOERT
EBRT Alone or Plus Chemotherapy
When EBRT with or without chemotherapy is utilized for patients with residual disease after resection or unresected lesions, most trials show an advantage to combined versus single modality treatment (EBRT plus chemotherapy versus EBRT or chemotherapy alone). Long-term survival is 10% to 15%.47,48
IORT Alone or Plus EBRT
For partially resected gastric cancer, the use of IOERT alone or in conjunction with EBRT has yielded a 5-year SR of 15% to 20%.47–58 Abe and Takahashi reported a Kyoto trial of surgery with or without IOERT in 211 patients in which subset analyses suggested SR advantages with IOERT for Japanese stages II to IV.49–51 The 5-year SR for stage IV disease in 27 IOERT patients was 15% (versus 0% for 18 patients treated with surgery alone; three of four IOERT survivors had residual disease). Five-year results with stages II and III were 84% (versus 62% for patients treated with surgery alone) and 62% (versus 37%). In a Pamplona pilot study, EBRT with or without chemotherapy has been combined with IOERT in 48 patients (EBRT doses of 46 Gy in 1.8- to 2.0-Gy fractions; IOERT dose usually 15 Gy).52 In 13 patients with stage IV disease, in-field relapse occurred in only three patients. Two of eight patients with known residual disease after maximal resection were long-term disease-free survivors (>22 and >65 months).
Separate randomized trials have been reported from Beijing53 and the NCI.54 In the Beijing series, patients with stage III (serosal involvement or node positive tumors) or IV disease (unresectable metastases or adjacent organ involvement) were randomized to surgery with or without IOERT (25 to 40 Gy). In a report of 200 patients,37 a SR advantage with IOERT was shown for stage III patients (5-year SR: 65% versus 30%; 8-year SR: 52% versus 22%; P < .01). At NCI, Sindelar et al. performed a small randomized trial of IOERT versus EBRT after complete resection, which demonstrated improved LC with IOERT but no SR benefit.54
A series of 24 patients with esophageal or gastric cancer received IOERT as a component of treatment at MCR in conjunction with pre- or post-op EBRT and maximal resection.58 Local and regional control of disease was excellent (85% at 5-year) but survival was less than optimal in view of the ∼80% rate of distant metastases.
MCR analyses demonstrated that even patients with local or regional relapse of gastric cancer may be candidates for salvage with aggressive approaches that includes IOERT as a component of treatment. For patients who received preoperative EBRT plus concurrent chemotherapy followed by maximal resection and IOERT, 4-year survival was ∼20%57 and 5-year survival exceeded 10%.58
Future Possibilities
For patients with locally advanced gastric cancer (resection but residual disease or unresectable), it seems reasonable to build on three positive segments of treatment data (EBRT plus chemotherapy, IOERT, neoadjuvant chemotherapy) and patterns of failure data.48 For patients with residual disease after resection, EBRT plus chemotherapy or IOERT with or without EBRT has produced long-term SR in 10% to 20% of patients in most single-institution analyses and randomized trials. Neoadjuvant chemotherapy for locally advanced disease has resulted in subsequent total resection of disease is ≥50% of patients in several European trials; however, the incidence of subsequent local regional failure (LRF) is ≥50% even after total resection. For patients with unresectable or borderline resectable disease on the basis of pre-op imaging, further evaluation of “neoadjuvant” chemotherapy with or without EBRT is reasonable. In patients with subsequent resection but residual disease or resection but high risk factors (beyond gastric wall, node positive, or both), IOERT or EBRT or both could be evaluated in conjunction with further chemotherapy.
Colorectal IORT (IOERT, HDR-IORT)
EBRT Alone or Plus Chemotherapy/Resection
EBRT has been combined with resection and chemotherapy for locally advanced colorectal cancers. In separate series from Princess Margaret Hospital (PMH) and Mayo Clinic, using EBRT alone (PMH, Mayo) or combined with systemic therapy (Mayo), the local relapse rate was more than 90% in evaluable patients.59Although a combination of EBRT (with or without 5-FU) with surgery for residual disease after subtotal resection or initially unresectable disease produces better LC than no resection, local relapse is too high at 30% to 50%. For locally recurrent rectal cancers, EBRT with or without chemotherapy results in excellent short-term palliation (6 to 12 months), but LC and long-term survival are infrequent (0% to 5%; 5 years).60
EBRT Plus IORT: Primary Unresectable Cancers
In an attempt to decrease local recurrence and improve survival, institutions in the United States, Europe, Japan, and Scandinavia have combined an IORT boost with fractionated EBRT (45 to 50 Gy in 1.8-Gy fractions) and resection.32,59–67 In US studies, the IOERT dose varies from 10 to 20 Gy, depending on the amount of residual disease after maximal resection (microscopic: 10 to 12.5 Gy; gross <2 cm: 15 Gy; gross ≥2 cm or unresectable: 17.5 to 20 Gy. The HDR-IORT dose at Memorial Sloan-Kettering Cancer Center (MSKCC) has been 12 or 15 Gy as calculated at a 0.5 cm distance from the Harrison-Anderson-Mick (HAM) applicator surface.62,63
MGH Results: EBRT Plus Resection With or Without IOERT
EBRT Plus Resection
The incidence of local relapse as a function of disease extent after preoperative EBRT alone or plus concomitant 5-FU (no IOERT) has been evaluated in three separate MGH analyses.59,60 For patients with locally unresectable T4 rectal cancers treated with preoperative EBRT and curative resection in the original MGH series, five of eight patients (62.5%) with persistent gross tumor extension beyond the rectal wall relapsed in the pelvis versus 0 of 3 patients with tumor confined to the wall or only microscopic extrarectal extension.59,60 In an analysis of 28 patients with tethered (T3) rectal cancers treated with preoperative EBRT and resection at MGH, 5-year actuarial local relapse and disease-free survival were 24% and 66%, respectively.59 No correlation between LC and posttreatment extent of tumor extension into or beyond the rectal wall and/or lymph node involvement was observed.
In another MGH analysis, 47 patients with T4 rectal cancers received 45 to 50.4 Gy pre-op EBRT and R0 resections.59 Patients did not receive IOERT, either because it was not felt to be indicated because of a favorable response to preoperative EBRT, or IOERT was not technically feasible. For 24 patients with no residual tumor or tumor confined to the rectal wall after preoperative EBRT, the 5-year actuarial local relapse rate was only 13% versus 68% for 27 patients with persistent transmural tumor and/or lymph node metastases and no clearly defined indication for IOERT.
EBRT Plus Resection, IOERT
In the initial MGH report, 16 patients with locally unresectable primary lesions received EBRT before resection and IOERT.60 When results were compared with historical controls treated only with EBRT and resection, 1- and 2-year SR was statistically better in the IOERT patients and disease relapse within irradiation fields was 0% versus 43%, respectively, (IOERT vs non-IOERT).
Sixty-four patients with locally unresectable T4 rectal cancer had full-dose pre-op EBRT (alone or plus 5-FU) followed by resection and IOERT at MGH.59,61 The 5-year LC and DSS for 40 patients undergoing complete resection plus IOERT were 91% and 63%, respectively (Table 16-6). For 24 patients undergoing partial resection, LC and DSS correlated with the extent of residual cancer (microscopic residual disease: 65% and 47%, respectively; gross residual disease: 57% and 14%, respectively).