Integration of surgery and radiation (external beam, EBRT; intraoperative, IORT) has become more routine for patients with locally advanced primary cancers and those with local-regional relapse. This article discusses patient selection and treatment from a more general perspective, followed by a discussion of patient selection and treatment factors in select disease sites (pancreas cancer, colorectal cancer, retroperitoneal soft-tissue sarcomas). Outcomes with combined modality treatment (surgery, EBRT alone or with concurrent chemotherapy, IORT) are discussed. The ultimate in contemporary integration of radiation and surgery is found in patients who are candidates for surgery plus both EBRT and IORT.
Key points
- •
Patient selection criteria: For patients with locally advanced primary cancer (borderline resectable, locally unresectable) or local-regional cancer relapse, the decision to proceed with combined-modality treatment that includes both surgery and radiation (external beam [EBRT], intraoperative [IORT]) should be determined by the surgeon and radiation oncologist in the setting of a joint preoperative consultation, whenever feasible.
- •
Patient evaluation: The pretreatment patient workup should include a detailed evaluation of the extent of the locally advanced primary or locally recurrent lesion combined with studies to rule out hematogenous or peritoneal spread of disease.
- •
Sequencing of surgery, EBRT, and IORT: Optimal sequencing of surgery and EBRT for locally advanced primary or local-regionally recurrent cancers should be discussed and determined at the time of a joint multispecialty consultation involving a surgeon, radiation oncologist, and often a medical oncologist. This collaboration allows input from all specialists with regard to studies that would be helpful for IORT and EBRT treatment planning, as well as whether IORT may be appropriate.
- •
Combined modality treatment–related morbidity: In patients with locally advanced primary or locally recurrent malignancies, the issue of morbidity following aggressive treatment is placed into clearer perspective by a comparison with tumor-related morbidity. For instance, when EBRT is used as the only radiation modality for patients with residual disease following surgical resection of locally advanced rectal cancer or those with locally recurrent colorectal cancers, more than 90% of patients have local persistence or relapse of disease, and most are dead within 2 to 3 years (end result is nearly 100% tumor-related morbidity and/or mortality).
Introduction
Integration of surgery and radiation has become more routine for patients with locally advanced cancers at many disease sites. The intent of this article is to discuss general patient selection, patient evaluation, and treatment factors with regard to issues that cross a variety of disease sites. This discussion is followed by presentation of patient selection and treatment factors for select disease sites (pancreas cancer, colorectal cancer, and retroperitoneal soft-tissue sarcomas) and a discussion of combined-modality treatment outcomes that include surgery, external-beam radiation (EBRT) alone, EBRT plus concurrent chemotherapy (chemoRT), and intraoperative radiation (IORT). The ultimate in contemporary integration of radiation oncology with surgery is found in patients who are candidates for surgery plus both EBRT and IORT.
Introduction
Integration of surgery and radiation has become more routine for patients with locally advanced cancers at many disease sites. The intent of this article is to discuss general patient selection, patient evaluation, and treatment factors with regard to issues that cross a variety of disease sites. This discussion is followed by presentation of patient selection and treatment factors for select disease sites (pancreas cancer, colorectal cancer, and retroperitoneal soft-tissue sarcomas) and a discussion of combined-modality treatment outcomes that include surgery, external-beam radiation (EBRT) alone, EBRT plus concurrent chemotherapy (chemoRT), and intraoperative radiation (IORT). The ultimate in contemporary integration of radiation oncology with surgery is found in patients who are candidates for surgery plus both EBRT and IORT.
General patient selection, evaluation, and treatment factors
Patient Selection Criteria
For patients with locally advanced (borderline resectable, locally unresectable) or locally recurrent cancers, the decision to proceed with combined-modality treatment that includes both surgery and radiation should be determined by the surgeon and radiation oncologist in the setting of a joint preoperative consultation, whenever feasible. Such a consultation allows input from both specialties with regard to studies that would be helpful for diagnosis and treatment planning, determination of optimal sequencing of surgery and external beam radiation (EBRT), as well as whether both EBRT and intraoperative radiation (IORT) are appropriate treatment modalities in addition to maximal surgical resection.
Patient Evaluation
The pretreatment patient workup should include a detailed evaluation of the extent of the locally advanced primary or locally recurrent lesion combined with studies to rule out hematogenous or peritoneal spread of disease. In addition to history and physical examination, the routine evaluation includes a complete blood count (CBC), liver and renal chemistries, chest film or computed tomography (CT), and tumor-specific serum tests (carcinoembryonic antigen [CEA], CA 19-9, CA-125, and so forth). When palpable pelvic primary tumors or relapses are immobile or fixed on rectal or bimanual examination, or symptoms suggest pelvic recurrence following primary resection, CT or magnetic resonance imaging (MRI) of the pelvis and abdomen can confirm lack of free space between the malignancy and a structure that may be surgically unresectable for cure (ie, presacrum, pelvic side wall). In such patients, preoperative chemoRT should be given before an attempt at resection. Distant metastatic spread should also be excluded with appropriate imaging (CT of chest/abdomen/thorax, positron emission tomography [PET or combined PET/CT], among others). If hematuria is present or findings on CT or MRI suggest bladder involvement, cystoscopy can be performed before or at the time of surgical exploration/resection.
Sequencing of Surgery, EBRT, and IORT
Optimal sequencing of surgery and EBRT for locally advanced or recurrent cancers should be discussed and determined at the time of a joint multispecialty consultation involving a surgeon, radiation oncologist, and, often, a medical oncologist. Such collaboration allows input from all specialists with regard to studies that would be helpful for IORT and EBRT treatment planning as well as whether IORT may be appropriate. Specialized surgeons (vascular, plastics, and so forth) may also need to become involved in subsequent consultations.
For many patients with locally advanced primary or locally recurrent lesions, preoperative EBRT of 45 to 50 Gy in 1.8- to 2.0-Gy fractions (plus concurrent chemotherapy as indicated by disease site) followed by exploration and resection in 3 to 6 weeks offers theoretical advantages over a sequence of resection followed by EBRT. The potential advantages include the following: (1) deletion of patients with metastases detected at the restaging workup or laparotomy thus sparing the potential risks of aggressive surgical resection alone or plus IORT; (2) possible tumor shrinkage with an increased possibility of achieving a gross total R0 or R1 resection; (3) alteration of implantability of cells that may be disseminated at the time of an R1 or R2 surgical resection; (4) reduction of treatment interval between EBRT and IORT (when resection and IORT precede EBRT, if postoperative complications ensue, the delay to EBRT ± chemotherapy may be excessive); (5) intact vascular supply to tumor with better oxygenation; (6) better clinical tumor volume (CTV) definition when gross tumor is intact; (7) ability often to treat more conservative EBRT fields and exclude more dose-limiting organs and structures.
The following general criteria have guided the selection of appropriate patients for IORT at the authors’ institution. (1) By definition, there must be no medical contraindications for exploratory surgery and an attempt at gross total resection. (2) Surgery alone will not achieve acceptable local control because of the high probability of microscopic or gross residual disease after maximal resection, based on preoperative imaging. (3) EBRT doses needed for adequate local control following subtotal resection or unresectable disease would exceed normal tissue tolerance (60–70 Gy in 1.8–2.0 Gy for microscopic residual [R1 resection], 70–90 Gy for gross residual [R2 resection] or unresected disease). (4) IORT will be given at the time of a planned surgical procedure. (5) The IORT plus EBRT technique would likely result in a more suitable therapeutic ratio between cure and complications by permitting direct irradiation of unresected or marginally resected tumor while surgically displacing or shielding dose-limiting structures or organs. (6) There is no evidence of distant metastases or peritoneal seeding (rare exceptions: treatable single-organ metastasis, slow progression of systemic disease, or excellent systemic therapy options).
EBRT Doses and Technique
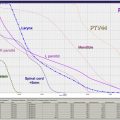
EBRT doses of 45 to 54 Gy are delivered in 1.8-Gy fractions, 5 days per week over 5 to 6 weeks in patients with no prior irradiation. For pelvic lesions, treatments are given with linear accelerators using at least 6 MV photons and 3-dimensional conformal radiation (3D-CRT) or intensity-modulated radiation (IMRT) techniques. With extrapelvic lesions, unresected or residual disease plus 3- to 5-cm margins of normal tissues are included to 40 to 45 Gy with 3D-CRT or IMRT. Reduced fields with margins of 2 to 3 cm are treated to 45 to 54 Gy. With a variety of disease sites (eg, gastrointestinal, gynecologic), concurrent chemotherapy is often given during EBRT with regimens based on 5-fluorouracil (5FU) or cisplatin.
For previously irradiated patients, an attempt is made to re-irradiate with low-dose preoperative EBRT (20–30 Gy in 1.8-Gy fractions or 1.5 Gy twice a day). This therapy is preferably delivered in combination with concurrent chemotherapy.
IORT Doses and Technique
In institutions that choose to have the availability of IORT as a component of treatment, a carefully constructed team needs to exist. This team should include a surgeon, radiation oncologist, anesthesiologist, operating room nursing and radiation physicist (alone or plus a radiation therapist). IORT is delivered, after maximal surgical resection, with electron-beam radiation (IOERT), high-dose-rate brachytherapy (HDR-IORT), or electronic brachytherapy/low-kilovolt IORT, depending on institutional preference.
IORT energy and dose are dependent on the amount of residual disease remaining after maximal resection, and on the EBRT component that has been given preoperatively or is feasible postoperatively. For patients who have received standard preoperative EBRT doses of 45 to 54 Gy (1.8-Gy fractions, 5 days per week), the IORT dose usually varies from 10 to 20 Gy: narrow margins or microscopic residual, 10 to 12.5 Gy; gross residual, 15 to 20 Gy; unresectable disease, 20 Gy. In previously irradiated patients, the IORT dose is usually 15 to 20 Gy if EBRT doses of 20 to 30 Gy can be safely given preoperatively or postoperatively. IORT doses of 25 to 30 Gy have been given to patients in whom no or limited EBRT is planned, but such doses have higher risks of normal structure intolerance.
The biological effectiveness of single-dose IORT is considered equivalent to 1.5 to 2.5 times the same total dose of fractionated EBRT. The effective dose in the IORT boost field, when added to the 45 to 50 Gy given with fractionated EBRT, is as follows: 60 to 70 Gy, IORT dose of 10 Gy; 75 to 87.5 Gy, 15-Gy IORT boost; 85 to 100 Gy, 20-Gy IORT boost.
Dose-Limiting Structures/Treatment-Related Morbidity
In patients with locally advanced primary or locally recurrent malignancies, the issue of morbidity following aggressive treatment is placed into clearer perspective by a comparison with tumor-related morbidity. For instance, when EBRT is used as the only radiation modality for patients with residual disease following surgical resection of locally advanced rectal cancer or those with locally recurrent colorectal cancers, more than 90% of patients have local persistence or relapse of disease, and most are dead within 2 to 3 years (the end result is nearly 100% tumor-related morbidity and/or mortality).
Patient selection and treatment factors by disease site
Pancreas Cancer
Patient evaluation and selection
The basic workup for a patient with pancreas cancer should consist of history, physical examination, basic laboratory studies (CBC, liver functions, renal function), and imaging studies. At present, most patients have a CT of the abdomen (with or without pelvis) followed by biopsy via CT or endoscopic ultrasonography (EUS) ( Table 1 ). At Mayo Clinic Arizona (MCA), tissue diagnosis is preferably achieved at the time of EUS rather than with thin-needle biopsy at the time of an abdominal CT or ultrasound examination. Accurate clinical staging requires high-quality, multiphase, helical CT to accurately define the relationship of the pancreatic cancer to the celiac axis and superior mesenteric vessels in 3 dimensions, as well as the absence of extrapancreatic disease.
| Diagnostic Procedure | Diagnosis and Staging Capability | Recommend Routine Use |
|---|---|---|
| Primary tumor/regional nodes a | ||
| Computed tomography (CT) of abdomen ± chest (pancreas protocol) | Most valuable modality to determine degree of extrapancreatic extension and distant metastases | Yes |
| Endoscopic ultrasonography (EUS) alone or with endoscopic retrograde cholangiopancreatography (ERCP) | More accurately defines involvement of pancreatic duct and inferior extent of biliary duct and lymph node involvement; predicts resectability | EUS: preferable, biopsy node(s), if feasible; ERCP: optional |
| Magnetic resonance imaging (MRI) | Clarify resectability if uncertain on CT | Optional |
| Metastatic workup | ||
| Chest films | Screen for metastases (mets) | Yes |
| CT of chest | Will detect small mets better than chest film | Optional |
| Positron emission tomography (PET/CT) | Excellent for detecting unsuspected mets | Optional; encouraged with borderline or unresectable lesions before chemoradiation |
| Laparoscopy | May allow visualization of small surface liver metastases or peritoneal seeding | Optional; encouraged if plan preop. or primary chemoradiation and CA 19-9 markedly elevated (≥1000) |
a Laboratory studies: complete blood count (CBC), creatinine, liver function studies (alkaline phosphatase [ALP], bilirubin, aspartate aminotransferase [AST], lactate dehydrogenase [LDH]), albumin. Tumor markers: CA 19-9 has high sensitivity (>90%) but low specificity (75%); carcinoembryonic antigen (CEA) (optional).
Objective, reproducible radiographic criteria are used to define disease extent and resectability. Potentially resectable disease is defined as: (1) the absence of extrapancreatic disease; (2) the absence of superior mesenteric or portal vein encasement, abutment or distortion, or associated thrombi, and presence of a patent superior mesenteric artery (SMA)–portal vein confluence; and (3) distinct fat planes around the SMA, celiac axis, and hepatic artery. The accuracy of CT in predicting unresectability and the inaccuracy of intraoperative assessment of resectability are both well established. Borderline resectable tumors, which may benefit from neoadjuvant therapy, include tumors with (1) abutment or encasement of the SMV/portal vein without arterial involvement whereby sufficient vessel is present proximally and distally to permit resection and venous reconstruction; (2) gastroduodenal artery encasement without extension to the celiac axis and with or without abutment or minor encasement of the hepatic artery; and (3) abutment of less than 180° of the SMA.
External-beam radiation
For patients with borderline resectable or unresectable cancers, preoperative chemoRT is preferably given before exploratory laparotomy and possible surgical resection alone or plus IOERT ( Table 2 ). At MCA, neoadjuvant gemcitabine plus abraxane is frequently given before preoperative chemoRT in view of the high risk of systemic relapse in these patient groups. For patients with resectable cancers, chemoradiation can be delivered either preoperatively or postoperatively (see Table 2 ). Some institutions prefer preoperative chemoradiation even for potentially resectable cancers.
| Disease Extent | Surgery | Irradiation (Alone or with Chemotherapy) | Chemotherapy |
|---|---|---|---|
| TisN0M0 | Pancreaticoduodenectomy and regional nodes | NR routinely; evaluate adjuvant concurrent chemo EBRT (CCRT) | NR routinely |
| Resectable | Pancreaticoduodenectomy (head lesion) a and regional nodes | Postop. CCRT, 45–54 Gy Evaluate preop. CCRT | CCRT: gemzar or 5FU based Systemic CT: gemzar based |
| Borderline resectable | Pancreaticoduodenectomy and regional nodes | Postop. CCRT, 45–54 Gy Evaluate preop. CCRT/IOERT b | CCRT: gemzar or 5FU based Systemic CT: gemzar based Evaluate neoadjuvant gemzar-abraxane prior to CCRT and after resection |
| Locally unresectable | Evaluate for resection after preop. CCRT | Preop. CCRT, b 45–50 Gy Attempt resection and IOERT | CCRT: gemzar or 5FU based Systemic CT: gemzar based Evaluate neoadjuvant gemzar-abraxane Evaluate alternative CCRT, maintenance chemotherapy |
| Metastatic | Palliative bypass or stent may be indicated | Palliative CCRT if indicated | ICT phase I, II, or III; MACT |
a If resectable body/tail lesion, distal pancreatectomy, and splenectomy plus regional nodes.
b Prefer preop. CCRT for borderline resectable and unresectable pancreas cancers, based on imaging.
EBRT is typically delivered through multiple fields (3D-CRT, IMRT) on a daily basis over a period of 5 to 6 weeks for a dose of 45.0 to 50.4 Gy in 1.8 daily fractions. Concurrent chemotherapy is given during EBRT 5 days per week (Monday to Friday) with infusional 5FU or capecitabine, or as weekly gemcitabine.
Nodal target volumes for tumors of the head of the pancreas include the pancreaticoduodenal, peripancreatic, porta hepatis, celiac, and suprapancreatic nodes. For lesions involving the body and tail of the pancreas, the suprapancreatic, celiac and splenic hilar nodes should be included; inclusion of more medially placed lymph nodes (pancreaticoduodenal and porta hepatis) can be optional, depending on the ability to spare normal organs and structures.
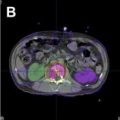
Normal tissue tolerances should be carefully respected with regard to kidneys, liver, stomach, small intestine, and spinal cord, and will influence the choice of beam direction and weighting. Use of non-coplanar beams can allow for greater sparing of normal liver and kidney parenchyma. When IORT is being considered as a component of treatment for patients with a medial lesion over the vertebral column (head of pancreas, medial body), the dose to the spinal cord should be limited to 35 to 40 Gy.
Intraoperative radiation
IORT for pancreatic cancer has predominantly been delivered with electrons. The beam energy and dose of IOERT is determined by the resection status and geometry of the treated field. Unresectable tumors often require energies of 12 to 18 MeV to achieve adequate coverage of the depth of the target tumor volume. After marginal resection of initially borderline resectable or unresectable lesions, the tumor bed can be adequately treated with lower-energy electrons in the 9 to 12 MeV range. Intraoperatively, the radiation oncologist and surgeon consult regarding the unresectable tumor or retroperitoneal area at risk for residual tumor after maximal resection of the primary, and the volume at risk is encompassed within a field defined by an IOERT applicator with a margin of at least 1 cm (ie, 5 cm unresectable tumor or tumor bed = 7-cm applicator). For cancers resected with narrow margins or microscopic residual tumor, IOERT doses in the range of 10.0 to 12.5 Gy are given (preferably 12.5 Gy for microscopic residual). For gross residual or unresected cancers, IOERT doses of 15 to 20 Gy have been used. Preferably a library of predefined isodose curves for a range of IOERT applicator field shapes and electron energies should be available in the operating room for intraoperative consultation. An electron energy should be chosen to adequately encompass the target tissues within the 90% isodose curves while limiting the dose to the spinal cord.
Surgical technique: pancreaticoduodenectomy
Pancreaticoduodenectomy involves the excision of the pancreatic head, duodenum, gallbladder, and bile duct, with or without removal of the gastric antrum, after careful inspection of all intra-abdominal organs and peritoneal surfaces. Any suspicious lesions should be biopsied and sent for frozen-section examination, because presence of distant metastasis is a contraindication to proceeding with resection. Vascular resection of the superior mesenteric–portal vein confluence using either lateral venectomy or segmental venous resection and reconstruction should be performed when there is no tissue plane between the tumor and superior mesenteric and portal vein. Despite all efforts, a microscopically positive margin will occur in 10% to 20% of cases, owing to perineural invasion along the mesenteric plexus at the origin of the SMA and microscopic lymphatic spread beyond the extent of the palpable tumor. Although there are numerous reports showing that a positive margin of resection is an independent predictor of poor long-term survival, this concept has been recently challenged.
One of the most debated technical aspects of the pancreaticoduodenectomy is the extent of the associated lymphadenectomy (standard vs extended). To date there have been 3 prospective randomized controlled trials that compare standard lymphadenectomy with the extended lymphadenectomy in patients undergoing resection of the pancreatic head for malignant disease. The largest 2 series (Yeo and colleagues from Johns Hopkins University, and Farnell and colleagues from Mayo Clinic, Rochester [MCR]) have both failed to show any survival benefit of extended lymphadenectomy for pancreatic head carcinoma. The third study, by Pedrazzoli and colleagues, also demonstrated no difference in the overall survival (OS), although patients with positive lymph nodes who underwent extended lymphadenectomy were noted to have improved survival. More recently, Iqbal and colleagues published a meta-analysis comparing standard with extended pancreaticoduodenectomy. The investigators concluded that extended pancreaticoduodenectomy offers no survival benefit and is associated with increased morbidity.
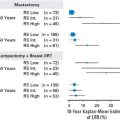
Combined modality outcomes: borderline resectable and unresectable cancers
For unresectable cancer of the pancreas, EBRT with concurrent 5FU-based or gemzar-based chemotherapy results in a doubling of median OS when compared with surgical bypass or stents alone (3–6 vs 9–13 months) and a 2-year OS of 10% to 20%. Five-year OS is rare, however, and local control is low. In a Thomas Jefferson University Hospital (TJUH) series, local control was achieved in 20% or fewer of patients treated with EBRT alone to doses of 60 to 70 Gy in 1.8- to 2.0-Gy fractions over 7 to 8 weeks. With chemoRT, local control was achieved in approximately 30% of patients ( Table 3 ).
| Series | Ref. | No. of Patients | Survival Overall (%) | Relapse (%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Median (mo) | 2-y | 3-y | P | Local | P | Liver/PS | |||
| Thomas Jefferson | |||||||||
| EBRT ± CT | 46 | 7.3 | — | — | 78 | — | |||
| IOERT/5FU-Leuc/EBRT a | 49 | 16 | 22 | 7 | 29 | 55 | |||
| Massachusetts General | |||||||||
| EBRT ± 5FU/IOERT | 22 | 16.5 | 33 | 20 | >.05 | 31 (2 y) | >.05 | — | |
| EBRT ± 5FU/IOERT + Miso | 63 | 12 | 20 | — | 45 (2 y) | — | |||
| EBRT ± 5FU/IOERT | 150 | 13 | 15 | 7 | — | — | |||
| Mayo Clinic Rochester | |||||||||
| EBRT ± CT | 122 | 12.6 | 16.5 | — | 80 (2 y) | 56 | |||
| IOERT/Postop. EBRT ± 5FU | 37 | 13.4 | 12 | — | .25 | 34 (2 y) | .0005 | 54 | |
| IOERT/Postop. EBRT ± 5FU | 56 | 10.5 | 6 | 0 | 35 (2 y) | — | |||
| Preop. EBRT + 5FU/IOERT | 27 | 14.9 | 27 | 20 | .001 | 32 (2 y) b | 52 | ||
| Mayo Clinic Arizona | |||||||||
| Preop. EBRT + 5FU or Gem/IOERT | 31 | 19 | 31 | 16 | 16 | 71 | |||
| R0/R1 resection after preop. CRT | 16 | 23 | 48 | 35 | .002 | 6 | .1 | 69 | |
| R2 resection or Unresectable | 15 | 10 | 13 | 0 | 27 | 73 | |||
a Perioperative 5FU/leucovorin was given before, during, and after EBRT.
b 2-year local relapse of 19% in the 23 patients with tumor diameter ≤7 cm versus 75% in the 4 patients with tumors >7 cm.
The combination of EBRT and intraoperative electrons (IOERT) has appeared to improve local control in IOERT series from Massachusetts General Hospital (MGH), Mayo Clinic, and TJUH. However, this has not translated into significant improvements in either median or 2-year OS (see Table 3 ).
In the latest update of MGH results, 150 patients with locally unresectable cancer of the pancreas received IOERT as a component of treatment from 1978 to 2001 in conjunction with EBRT and 5FU-based chemotherapy. Long-term survival was seen in 8 patients, and 5 were alive at or beyond the 5-year interval. Actuarial 1-, 2-, 3-, and 5-year survival for the 150 patients was 54%, 15%, 7%, and 4%, respectively, and median survival was 13 months (see Table 3 ).
In the initial MCR series, IOERT usually preceded EBRT. When results were compared with EBRT ± 5FU, local control at 1 year was 82% for EBRT plus IORT ± 5FU versus 48% for EBRT ± 5FU; at 2 years it was 66% versus 20%, respectively ( P = .0005; see Table 3 ). This result did not translate into a difference in either median or 2-year OS (13.4 months median OS with IOERT vs 12.6 months without IOERT; 12% vs 16.5% 2-year OS) in view of a high incidence of abdominal relapse in both groups of patients (20 of 37 IOERT patients, or 54%, developed liver or peritoneal metastases vs 68 of 122, or 56%, in non-IOERT patients).
In an attempt to improve patient selection and survival, MCR investigators delivered the chemoRT preoperatively instead of postoperatively. Median OS was 14.9 months with this sequence, and 2- and 5-year OS were respectively 27% and 7%. These findings were compared with results in 56 patients who had IOERT plus postoperative EBRT (median OS 10.5 months, 2-year OS 6%, P = .001; see Table 3 ). Although 2-year OS appeared to be better with the altered sequence of preoperative chemoRT followed by IOERT, this was likely due to altered patient selection, as the rate of liver plus peritoneal relapse did not change (14 of 27 at risk, 52%).
Investigators at MCA have used preoperative chemoradiation followed by restaging, and surgical exploration with resection/IOERT, as indicated, for select patients with borderline resectable or unresectable cancer of the pancreas. A series of 31 patients with no prior treatment had subsequent surgical exploration after preoperative chemoRT. R0 or R1 resection was performed in 16 of 31 patients, and 28 of 31 received IOERT. As seen in Table 3 , median OS for the total group of patients was 19 months, 2-year OS 31% and 3-year OS 16% (see Table 3 ). Survival outcomes appeared to be improved in the 16 patients with gross total resection (R0/R1) after preoperative chemoRT versus the 15 patients with R2 resection or unresectable disease (median OS 23 vs 10 months; 2-year OS 48% vs 13%; 3-year OS 35% vs 0%; P = .002, log rank). Liver or peritoneal relapse was documented in 22 of 31 patients (71%).
A pooled analysis of 270 patients from 5 European Institutions was presented at the 2008 meeting of the International Society of Intraoperative Radiation Therapy (ISIORT 2008) by Valentini and colleagues. Radical surgery was performed in 247 cases (91.5%; R0 resection 53.4%, R1 resection 27.4%, R2 resection 19.2%) and exploratory laparotomy in 8.5%. Surgery was preceded by EBRT in 63 patients (concurrent chemotherapy, 38% of patients) and 106 received postoperative EBRT (concurrent chemotherapy, only 7.5% of patients). In the total group of patients, median OS was 19 months and 5-year OS was 17.7%. Survival and local control appeared to be better in patients treated with preoperative radiation or chemoRT before IORT (ie, preoperative EBRT or chemoRT/IORT) compared with either the postoperative sequence of treatment (IORT/postoperative EBRT or chemoRT) or IORT alone (median OS of 30 vs 22 and 13 months; local control: median not reached with preoperative EBRT/chemoRT group vs median 28 months with postoperative EBRT/chemoRT and median 8 months with IORT alone). On multivariate analysis, nodal status and timing of EBRT/chemoRT significantly affected survival.
Summary and future possibilities
Long-term survival and disease control are achievable in select patients with borderline resectable or locally unresectable cancer of the pancreas, and survival appears to be better in patients with resection after full-dose preoperative chemoRT. Accordingly, continued evaluation of curative-intent combined modality therapy is warranted in this high-risk population of patients. However, additional strategies are needed to improve both resectability rates after preoperative chemoRT and disease control (local, distant). The incidence of abdominal relapse must be decreased by using either more aggressive or new regimens of systemic or regional therapy (intrahepatic, intraperitoneal). Targeted therapies (ie, epidermal growth factor receptor inhibitors, vascular endothelial growth factor inhibitors) and pancreas cancer vaccines are also being evaluated in an attempt to improve systemic disease control. As improvements are made in distant disease control, the benefit of improved local control with IORT-containing regimens may become even more apparent.
Colorectal Cancer
Patient selection and evaluation
For patients with locally unresectable or borderline resectable primary colorectal cancers (T4N0M0; tethered T3N0M0) or local or regional relapse, the indications for preoperative chemoRT alone or plus IORT should be determined by the surgeon and radiation oncologist in the setting of a joint preoperative consultation, whenever feasible. This collaboration allows input from both specialties with regard to studies that would be helpful in determining optimal sequencing of surgery and chemoRT, optimizing treatment planning for EBRT and deciding whether IORT is indicated ( Tables 4 and 5 ). Patients with resectable but high-risk rectal cancers (T3N0, TanyN1–3M0) may also be candidates for combined-modality treatment that includes preoperative or postoperative chemoRT without IORT (see Table 5 ).
| Diagnostic Procedure | Diagnosis and Staging Capability | Recommend Routine Use |
|---|---|---|
| Primary tumor ± regional nodes a | ||
| Colonoscopy | Very accurate modality for detecting and defining primary lesions in rectum, sigmoid (flexible sigmoidoscopy [flex sig]), or remaining colon (colonoscopy) | Yes |
| Endorectal ultrasonography (EUS) | Useful in defining depth of penetration of primary rectal cancers; may define suspicious lymph nodes | Yes, if preoperative chemoradiotherapy is considered; biopsy suspicious nodes |
| Computed tomography (CT) of abdomen + pelvis b | Most valuable of all modalities for determining extrarectal or extracolonic local invasion and nodal metastases | Yes |
| CT colonography with intravenous contrast | Highly accurate for detecting/defining colon lesions before surgery, equal to CT of abdomen and pelvis for local and distal metastases | Optional. Recommend if need to localize and stage a known colon lesion. Can replace barium enema if incomplete colonoscopy |
| Barium enema | Double-contrast examination alone or single-contrast examination used in combination with flex sig to identify colon lesions. Less accurate than colonoscopy | Optional. Double- or single-contrast barium enema used in combination with flex sig for screening or for incomplete colonoscopy |
| Metastases | ||
| Chest film; CT chest | Chest film used commonly for metastasis screening; CT chest is best for detecting metastases | Yes |
| CT of abdomen/pelvis or CT colonography with intravenous contrast | Useful in defining para-aortic node enlargement or liver metastases; CT colonography equal to CT of abdomen and pelvis for local and distant metastases | Yes regarding CT abdomen/pelvis; Optional regarding CT colonography: recommend if need to localize and stage a known colon lesion |
| Positron emission tomography (PET) | Used to detect CT occult metastases or further evaluate indeterminate CT findings; preferable as a merged PET/CT study | Yes, with rising CEA and negative or indeterminate CT; before resection or radiofrequency ablation of liver metastases |
| Magnetic resonance imaging (MRI) of liver | Used primarily to evaluate indeterminate liver lesions on CT | Optional. Recommended for indeterminate liver lesion at CT or contraindication to CT (dye allergy, renal failure) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree