Highlights
- •
Racial and insurance disparities impact access to integrated care.
- •
Advanced cancer stages increase likelihood of integrated care.
- •
Treatment and hospital factors minimally affect delivery of integrated care.
- •
Future studies need more detailed data and patient views on integrated care.
Abstract
Introduction
Cancer patients often have complex medical needs from diagnosis to survivorship/end-of-life care. Integrated care, including care coordination, multidisciplinary rounds, and supportive care services, is crucial for high-quality cancer care. Yet, factors influencing integrated care receipt are not well understood. This study describes patterns of integrated care among individuals diagnosed with kidney or urinary bladder cancer and examines patient- and hospital-level factors associated with these services.
Methods
Analyzing 2019 National Cancer Institute Patterns-of-Care data, we assessed integrated care service receipt among stage I to IV kidney and stage 0a to IVb urinary bladder cancer patients aged ≥ 20 years using a stratified Surveillance, Epidemiology, and End Results registry sample. Integrated care services within 12 months postdiagnosis were identified by medical record abstraction. Multivariable logistic regression analyses identified patient, clinical, and hospital-level factors significantly associated with receipt of integrated care.
Results
Significant variations in receiving integrated care were observed based on insurance status; uninsured patients less likely to receive these services. Racial/ethnic differences were also noted, as non-Hispanic white patients had higher likelihoods of receiving integrated care. Stage IV kidney cancer patients were 2.63 times [1.44–4.79] more likely to receive integrated care than stage I patients. Treatment characteristics and hospital-level factors appeared to have minimal impact on receiving these services.
Conclusion
The lower likelihood of receiving integrated care among patients with no insurance and among certain racial/ethnic groups underscores gaps in equitable access to patient-centered cancer care. Future research should include patient perspectives to enhance understanding of unmet needs and influencing factors related to integrated care services.
1
Introduction
Cancer etiology is often multifactorial and complex: genetic, lifestyle, and environmental factors may influence the development of cancers and their subtypes [ ]. The intricacies of cancer care demand a personalized approach at every stage—from diagnosis to treatment and survivorship [ ]. Designing and implementing high-quality patient-centered cancer care in healthcare systems varying in organizational, cultural, and structural characteristics is challenging. Yet, it is essential for achieving high-quality, patient-centered outcomes. This is underscored by key initiatives, including the development of ASCO’s Patient-Centered Cancer Care Standards [ ], the National Committee for Quality Assurance’s Patient-Centered Specialty Practice Recognition Program [ ], the National Cancer Institute (NCI)’s funding opportunities that include evaluation of models of patient-centered care [ ] and President Biden’s Cancer Moonshot initiative, which includes an emphasis on patient navigation [ ].
Integrated care refers to “the management and delivery of health services so that clients receive a continuum of preventive and curative services, according to their needs over time and across different levels of the health system” [ ]. Care coordination, multidisciplinary rounds, and supportive care are types of integrated care services that may be provided as part of cancer care. Integrated care approaches including patient navigation, home telehealth, and nurse case management can improve patient experience and quality of end-of-life care [ ]. Evidence suggests that these integrated approaches can double the likelihood of appropriate healthcare utilization and enhance outcomes like therapy planning, pain control, patient survival, and quality of life [ ].
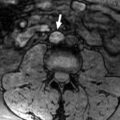
However, the integration of such care faces obstacles primarily due to inadequate evidence on how various factors—ranging from socioeconomic status to healthcare organization—affect its delivery. Current insights are largely derived from qualitative research or registries focusing on limited cancer types or specific patient groups [ ]. To address this gap, our study focuses on delivery of integrated care among patients with kidney or urinary bladder cancer, diseases that involve complex treatment regimens and may benefit from integrated care [ ]. These cancers often require a multidisciplinary approach across various stages, potentially involving urologists, medical oncologists, radiation oncologists, and other specialists, with treatment modalities ranging from surgery and systemic therapies to radiation and immunotherapy, depending on the stage and specific characteristics of the disease. For instance, advanced kidney cancer may require a combination of surgical intervention, systemic therapies, and management of complications, necessitating coordination between urologists, medical oncologists, and supportive care specialists. This complexity underscores the potential benefits of integrated care in managing these cancers. To provide a deeper understanding of the factors influencing receipt of the patient-centered cancer care, we used cancer registry data linked with electronic medical records and explored the relationship of patient’s sociodemographic and clinical characteristics, and hospital structure factors with the care coordination, multidisciplinary rounds, and supportive care services.
2
Materials and methods
2.1
Data sources and study population
We used NCI Patterns of Care (POC) studies to analyze care coordination, multidisciplinary rounds, and supportive care for individuals diagnosed with kidney and urinary bladder cancer ( Supplemental Document ). Conducted by the NCI in partnership with Surveillance, Epidemiology, and End Results (SEER) registries, POC studies draw stratified random samples from these registries and collect detailed diagnostic and treatment data through medical record abstracting [ , ]. In 2021, the POC studies included samples of men and women diagnosed with stage I to IV kidney cancer (renal cell cancer/renal adenocarcinoma) stratified by sex, race/ethnicity, and stage; and men and women diagnosed with stage 0a to IVb urinary bladder cancer (transitional cell carcinoma/urothelial carcinoma) stratified by sex and race/ethnicity from January 1, 2019, to December 31, 2019 [ ]. All participating registries completed Institutional Review Board (IRB) review and approval or exemption prior to initiation of POC data collection using a standardized data abstraction tool. Information on accessing POC data is available online [ ].
Patients aged ≥ 20 years diagnosed with malignant kidney cancer cases using International Classification of Diseases for Oncology, third edition (ICD-O-3) C64.9 with histology codes of 8260, 8310, 8312, 8316, 8317, 8319, and 8480 or diagnosed with in situ or malignant urinary bladder cancer cases using ICD-O-3 C67.0–67.9 with histology codes of 8020, 8031, 8082, 8120, 8122, 8130, and 8131 were included [ ]. While this code captures kidney cancer cases as defined by SEER registries during the study period, it may not encompass all possible subtypes or presentations of kidney cancer. This approach aligns with standard SEER classification practices for population-based cancer registries.
2.2
Outcome measures
Our primary outcome was a binary variable indicating whether patients received any integrated care services—including care coordination, multidisciplinary rounds, or supportive care—within 12 months postdiagnosis, as documented in their medical records. We used standardized questions to abstract this data (see Supplemental Document ) and measured the receipt of each specific type of integrated care service separately. Care coordination, as an integral component of integrated care, is an ongoing process that can occur before, during, and after specific treatments. Given this dynamic nature of care coordination, we did not assume or require that all instances of care coordination preceded treatment variables.
2.3
Independent variables
Patient-level independent variables encompassed sociodemographic and health factors, tumor characteristics, and treatment details. Sociodemographic factors included age, sex, race/ethnicity, marital status, smoking status, insurance status, Charlson Comorbidity Index scores, obesity, and census region. Insurance status was assessed 30 days postdiagnosis to reflect any changes after initial diagnosis. Tumor characteristics covered stage, size, extension, metastasis at diagnosis, and site of metastasis. Treatment variables for kidney cancer included surgery, radiation, and systemic therapy; for urinary bladder cancer, they included upper urinary tract involvement, surgery type, radiation, intravesical therapy, and oral/parenteral therapy. Hospital-level variables comprised bed count, residency programs, ownership, Total Performance Score (a Centers for Medicare & Medicaid Services (CMS) quality measure), Medicare Star Ratings, and average oncology patient stay (days).
2.4
Statistical analysis
Separate analyses were conducted for kidney and bladder cancer patients using Pearson’s chi-square tests to compare the distribution of independent variables and their association with receipt of integrated care services. Bivariate logistic regression assessed the impact of patient- and hospital-level factors on care receipt, informing the selection of variables for multivariable logistic regression models. However, we recognized that statistical significance alone might not capture all clinically relevant factors. Therefore, among the variables that did not show significant associations with each outcome in bivariate analyses, we selectively included some based on our understanding of patient- and hospital-level barriers to care/access to care and care pathways or quality of care [ , ]. This allowed us to incorporate important factors that might influence our outcomes, even if their effects were not immediately apparent in simpler statistical tests.
The first multivariable regression models adjusted for patient- and hospital-level factors. The second multivariable regression models adjusted for tumor characteristics and treatment information. For patients with kidney cancer, these were: vital status at last follow-up; stage at diagnosis; whether patients had a treatment protocol registration (i.e., clinical trial participation); receipt of surgery; receipt of any radiation therapy; and receipt of any systemic therapy. For patients with bladder cancer, these were: stage at diagnosis; type of surgery; receipt of any radiation therapy; receipt of any intravesical therapy; and receipt of any oral and parenteral systemic therapy. The final model adjusted for patient, hospital, tumor, and treatment factors: age; sex; race/ethnicity; insurance status; obesity; vital status at last follow-up; region; stage at diagnosis; receipt of any surgery for kidney cancer and type of surgery for urinary bladder cancer; receipt of any radiation therapy; receipt of any systemic therapy for kidney cancer and receipt of any systemic therapy by modality (intravesical and oral and parenteral) for urinary bladder cancer; hospital bed size; and oncology inpatient average length of stay. To focus on the population that potentially benefits most from integrated care, we conducted sensitivity analyses examining patterns and predictors of integrated care specifically among stage III to IV kidney cancer patients (N = 976) and stage II to IV urinary bladder cancer cases (N = 357). All analyses used POC sampling weights to provide estimates generalizable to the SEER population and were conducted in Stata 18.0.
3
Results
The study population includes 2,305 kidney cancer patients and 1,814 with urinary bladder cancer. Table 1 presents the frequency of care coordination, multidisciplinary rounds, and supportive care services. About 63% of kidney cancer and 44% of urinary bladder cancer patients received integrated care services. The most common combination was care coordination and supportive care. Care coordination was primarily provided by case managers or care managers, often with nursing degrees. Urologists were the predominant physicians treating both cancers, but medical oncologists, radiation oncologists, and non-urologist surgeons were more involved in kidney cancer treatment. Interdisciplinary team conferences were the most common multidisciplinary rounds. Physical therapy/exercise therapy/rehabilitation and nutrition counseling were the most frequent supportive care services for both cancers.
| Kidney (%) | Urinary bladder (%) | |
|---|---|---|
| Unweighted N | 2,305 | 1,814 |
| Pattern of integrated care services | ||
| No integrative care | 36.96 | 56.40 |
| Care coordination alone | 13.59 | 8.98 |
| Multidisciplinary rounds alone | 3.10 | 3.43 |
| Supportive care alone | 6.99 | 4.94 |
| Care coordination and multidisciplinary rounds | 4.30 | 4.15 |
| Care coordination and supportive care | 17.89 | 9.78 |
| Multidisciplinary rounds and supportive care | 1.90 | 3.82 |
| Care coordination, multidisciplinary rounds, and supportive care | 15.27 | 8.35 |
| Number of care coordination services received | ||
| 0 | 48.95 | 68.74 |
| 1 | 40.49 | 24.03 |
| 2+ | 10.56 | 7.22 |
| Types of providers for care coordination services 1 | ||
| Coordinators | 17.97 | 17.05 |
| Navigators | 14.76 | 21.13 |
| Managers | 64.98 | 57.67 |
| Other | 2.29 | 4.15 |
| Degree or credentials of individuals who completed the first care coordination services in medical record | ||
| Nurse/nurse specialist/nurse practitioner | 43.87 | 25.78 |
| Social worker | 8.43 | 4.71 |
| Pharmacy/pharmacy technician | 0.98 | 0.68 |
| Physician assistant | 1.97 | 2.17 |
| Physician | 11.00 | 10.58 |
| Financial counselor | 0.15 | 0.00 |
| Nonhealthcare provider/lay person/other 2 | 1.65 | 1.54 |
| Unknown | 1.72 | 0.66 |
| Types of physicians involved in the treatment | ||
| Urologist | 88.68 | 95.88 |
| Medical oncologist | 36.13 | 22.53 |
| Radiation oncologist | 12.33 | 7.22 |
| Surgeon other than a urologist | 9.69 | 2.86 |
| Other 3 /unknown | 8.52 | 3.41 |
| Types of multidisciplinary rounds at which the case was presented in the 12 months following diagnosis | ||
| Multidisciplinary care rounds/conference/team meeting | 5.81 | 4.61 |
| Interdisciplinary team conference/meeting | 21.62 | 17.70 |
| Molecular tumor board | 0.20 | 0.24 |
| Virtual tumor board | 0.46 | 0.64 |
| Other type of tumor board, including in-person | 3.46 | 2.22 |
| Other 4 | 2.14 | 2.41 |
| Types of supportive care services provided in the 12 months following diagnosis | ||
| Physical therapy/exercise therapy/rehabilitation | 26.81 | 16.58 |
| Occupational therapy | 12.06 | 7.52 |
| Enterostomal therapy/ostomy care | 0.84 | 4.54 |
| Mental health/psychosocial therapy | 5.48 | 2.87 |
| Nutrition counseling | 20.31 | 13.26 |
| Financial counseling | 4.34 | 1.77 |
| Spiritual counseling/spiritual support/pastoral care | 10.07 | 4.70 |
| Other 5 | 12.06 | 7.52 |
1 Coordinators = care coordinator and client coordinator. Navigators = care navigator, patient navigator, nurse navigator, clinical navigator, cancer navigator, lay navigator, financial navigator, and financial counselor Managers = case manager and care manager. Other = action personnel, social worker, clinical care liaison/hospital liaison, genito-urinary (GU) Navigator, infusion nurse, nurse coordinator, personal health partner/coordinator, physician, planning navigator, postacute navigator, program coordinator, research coordinator, research nurse, shift coordinator, support coordinator, transition care coordinator, unit coordinator, admission navigator, clinic coordinator, home care, housing coordinator, patient assistance, patient educator, transplant coordinator, and wellness coordinator.
2 Certied therapeutic specialist, clinical research coordinator, licensed mental health counselor, case manager, chaplain, master of science, and clinical care liaison.
3 Anesthesiologist, cardiologist, neurologist, pulmonologist, diagnostic radiologist, emergency department, nephrologist, gastroenterologist, internal medicine, gynecologist, infectious disease, interventional radiologist, primary care provider, orthopedics, palliative medicine, dermatologist, endocrinologist, psychiatrist, ophthalmologist, and radiologist, NOS.
4 Quality control conference, structural heart conference, committee review, conference, divisional conference, expert committee, gitb conference, radiology conference, and transplant selection conference.
5 Pain management/palliative care, respiratory therapy, music therapy, speech therapy, well-being support, wound care, acute pain services, and supportive dermatology-oncology clinic.
Table 2 compares characteristics of kidney cancer patients by receipt of integrated care services. Patients receiving services were more often non-Hispanic White or Hispanic, with Medicare or Private/Tricare insurance, and less likely to have Medicaid or no insurance. A larger proportion of these patients were former smokers, overweight, or from the West Census region, while fewer were current smokers, obese, or from the Northeast or South. Patients receiving services were more likely diagnosed with stage IV disease, participated in clinical trials, and less often underwent surgery, compared to those with stage I disease. About half received care coordination, 24% received multidisciplinary rounds, and 40% received supportive care ( Supplemental Table 1 ). Characteristics of patients receiving care coordination, multidisciplinary rounds, or supportive care closely resembled those receiving any integrated care, but those receiving multidisciplinary rounds were more often Hispanic, Medicare beneficiaries, under- or healthy weight, from the West, and treated in hospitals with higher Total Performance Scores. Those receiving supportive care more frequently underwent radiation therapy and more systemic therapy treatments.
| Total study population (%) | No integrated care services (%) | Any integrated care services (%) | P -value | |
|---|---|---|---|---|
| Unweighted N (weighted %) | 2,305 (100.00) | 856 (36.96) | 1,449 (63.04) | |
| Patient characteristics | ||||
| Age at diagnosis (years) | 0.151 | |||
| < 50 | 14.51 | 16.84 | 13.14 | |
| 50–59 | 21.91 | 20.22 | 22.90 | |
| 60–69 | 33.72 | 33.84 | 33.65 | |
| 70–79 | 23.57 | 24.16 | 23.23 | |
| ≥ 80 | 6.30 | 4.94 | 7.09 | |
| Male | 61.07 | 60.39 | 61.47 | 0.733 |
| Race/ethnicity | < 0.001 | |||
| Non-Hispanic White | 64.89 | 60.75 | 67.31 | |
| Non-Hispanic Black | 10.03 | 13.34 | 8.09 | |
| Hispanic | 15.93 | 14.12 | 16.99 | |
| Other | 9.15 | 11.78 | 7.61 | |
| Married | 60.03 | 58.30 | 61.05 | 0.382 |
| Insurance status > 30 days of diagnosis | 0.006 | |||
| Medicare | 39.29 | 36.25 | 41.07 | |
| Medicaid | 16.00 | 17.28 | 15.26 | |
| Private/tricare | 38.31 | 37.00 | 39.09 | |
| VA/IHS/other | 1.26 | 1.61 | 1.03 | |
| Missing/no insurance | 5.15 | 7.66 | 3.56 | |
| Number of comorbid conditions | 0.280 | |||
| None | 63.29 | 65.01 | 62.29 | |
| 1 | 26.31 | 26.31 | 26.04 | |
| ≥ 2 | 10.56 | 8.68 | 11.67 | |
| Smoking status | < 0.001 | |||
| Never smoked | 48.76 | 48.52 | 48.89 | |
| Current smoker | 15.95 | 17.34 | 15.13 | |
| Former smoker | 32.94 | 28.40 | 35.61 | |
| Unknown | 2.36 | 5.74 | 0.37 | |
| Obesity | 0.001 | |||
| Underweight or Healthy weight | 23.78 | 22.51 | 24.53 | |
| Overweight | 29.58 | 23.89 | 32.92 | |
| Obese | 46.64 | 53.60 | 42.55 | |
| Vital status at last Follow-up | 0.057 | |||
| Alive | 89.00 | 91.42 | 87.59 | |
| Dead | 11.00 | 8.58 | 12.41 | |
| Region | < 0.001 | |||
| Northeast | 6.81 | 10.16 | 4.85 | |
| Midwest | 6.74 | 6.41 | 6.94 | |
| South | 26.78 | 33.26 | 22.97 | |
| West | 59.67 | 50.17 | 65.23 | |
| Tumor characteristics | ||||
| Stage at diagnosis | < 0.001 | |||
| Stage I | 46.01 | 58.37 | 38.77 | |
| Stage II | 5.37 | 6.15 | 4.91 | |
| Stage III | 13.05 | 12.34 | 13.46 | |
| Stage IV | 35.57 | 23.14 | 42.85 | |
| Site of metastases | ||||
| Bone | 15.47 | 9.40 | 19.03 | < 0.001 |
| Distant lymph Nodes | 8.84 | 5.01 | 11.08 | 0.001 |
| Liver | 7.26 | 3.95 | 9.20 | 0.003 |
| Lung | 23.46 | 16.23 | 27.70 | < 0.001 |
| Other | 13.31 | 6.58 | 17.25 | < 0.001 |
| Treatment characteristics | ||||
| Treatment protocol registration 1 | 0.010 | |||
| No/refused/unknown | 96.95 | 98.74 | 95.90 | |
| Yes | 3.05 | 1.26 | 4.10 | |
| Primary surgery type 2 | < 0.001 | |||
| None | 26.84 | 19.50 | 31.15 | |
| Partial or subtotal nephrectomy (kidney or renal pelvis) or partial ureterectomy (ureter) | 23.50 | 29.09 | 20.22 | |
| Complete/total/simple nephrectomy for kidney parenchyma; nephroureterectomy; radical nephrectomy | 42.83 | 43.76 | 42.20 | |
| Other | 6.83 | 7.65 | 6.35 | |
| Any radiation therapy | 11.30 | 7.43 | 13.57 | 0.006 |
| Number of systemic Therapy agents received | < 0.001 | |||
| 0 | 70.00 | 80.34 | 63.93 | |
| 1–2 | 20.42 | 14.59 | 23.84 | |
| 3+ | 9.58 | 5.07 | 12.22 | |
| Hospital characteristics | ||||
| Bed size 3 | 0.984 | |||
| 1–299 beds or Other | 35.64 | 35.38 | 35.79 | |
| 300–499 beds | 27.24 | 27.17 | 27.19 | |
| ≥ 500 beds | 37.12 | 37.45 | 36.92 | |
| Approved residency training | 0.166 | |||
| No/unknown | 28.42 | 30.83 | 27.01 | |
| Yes | 71.58 | 69.17 | 72.99 | |
| Hospital ownership 4 | 0.007 | |||
| Government, nonfederal | 17.18 | 14.49 | 18.75 | |
| Non-government, not-for-profit | 70.15 | 69.39 | 70.60 | |
| Non-government, for-profit; physician office | 11.62 | 14.02 | 10.21 | |
| Government, federal | 0.76 | 1.47 | 0.34 | |
| Unknown | 0.29 | 0.64 | 0.00 | |
| TPS | 0.494 | |||
| 0–28.5 or unknown | 31.77 | 33.13 | 30.98 | |
| > 28.5–34.2 | 25.66 | 25.62 | 25.68 | |
| > 34.2–39.7 | 22.87 | 23.82 | 22.32 | |
| > 39.7 | 19.70 | 17.44 | 21.02 | |
| Star rating | 0.108 | |||
| 1–2 or unknown | 14.47 | 11.94 | 15.93 | |
| 3 | 59.49 | 62.54 | 57.72 | |
| 4–5 | 26.05 | 25.52 | 26.35 | |
| Oncology average length of stay (days) | < 0.001 | |||
| 0–5.25 | 30.04 | 29.17 | 30.55 | |
| > 5.25–8.48 | 45.38 | 48.44 | 43.59 | |
| > 8.48 | 13.66 | 8.54 | 16.67 | |
| Unknown | 10.92 | 13.86 | 9.19 |
1 Other = Patient or patient’s guardian refused treatment protocol; Treatment protocol participation recommended, unknown if registered; Unknown, not stated.
2 Partial or subtotal nephrectomy (kidney or renal pelvis) or partial ureterectomy (ureter) include but are not limited to segmental resection and wedge resection. Complete/total/simple nephrectomy for kidney parenchyma and nephroureterectomy include bladder cuff for renal pelvis or ureter. Radical nephrectomy may include removal of a portion of vena cava, adrenal gland(s), gerota’s fascia, perinephric fat, or partial/total ureter. Other surgery types include local tumor destruction or excision, or any nephrectomy in continuity with the resection of other organ(s) (colon, bladder), which can be partially or totally removed; nephrectomy, NOS or ureterectomy NOS; surgery NOS; unknown if surgery performed; death certificate ONLY.
3 Other = outpatient department (OPD), including doctor’s office or other nonhospital outpatient setting, including facilities with zero beds OR unknown.
4 Government, nonfederal includes state, county, city, city/county, or hospital district/hospital authority. Non-government, not-for-profit includes church-operated, or other not-for-profit hospitals. Non-government, for-profit hospitals include individual, partnership, or corporation hospitals. Government, federal includes air force, army, navy, public health service, veterans administration, public health service Indian service, department of justice, other federal facilities.
Table 3 presents patient-, treatment-, and hospital-level characteristics among individuals diagnosed with urinary bladder cancer by receipt of integrated care services. Patients who received any services were significantly older, more likely to have Medicare coverage, and less likely to have missing/no insurance. A significantly larger proportion of patients who received integrated care services were former smokers; from the West census region; diagnosed with stage III or IV (14.2% vs. 2.7% of those who received no integrated care services); and participated in clinical trials (4.0% vs. 0.7% with no integrated care services). Almost all patients with urinary bladder had surgery; however, a significantly smaller proportion of patients who had any integrated care services had electrocautery or excisional biopsy, while a larger proportion received radiation therapy. Supplemental Table 2 shows characteristics by care type, like those receiving any integrated care. About 31% and 27% received care coordination and supportive care, respectively, with 20% undergoing multidisciplinary rounds. Those in multidisciplinary rounds often were overweight, former smokers, from the West, received intravesical therapy, and were treated in not-for-profit non-government hospitals with higher performance scores and shorter oncology stays. Patients receiving care coordination or supportive care more frequently had oral or parenteral systemic therapy.
| Total study population (%) | No integrated care services (%) | Any integrated care services (%) | P -value | |
|---|---|---|---|---|
| Unweighted N (weighted %) | 1,814 (100.00) | 1,146 (56.56) | 668 (43.44) | |
| Patient characteristics | ||||
| Age at diagnosis (years) | 0.035 | |||
| < 59 | 12.05 | 13.86 | 9.69 | |
| 60–69 | 26.24 | 28.53 | 23.26 | |
| 70–79 | 35.10 | 33.15 | 37.65 | |
| ≥ 80 | 26.60 | 24.45 | 29.40 | |
| Male | 62.71 | 59.57 | 66.80 | 0.054 |
| Race/ethnicity | ||||
| Non-Hispanic White | 83.67 | 83.00 | 84.54 | 0.522 |
| Non-Hispanic Black | 4.26 | 4.04 | 4.53 | |
| Hispanic | 6.29 | 7.02 | 5.33 | |
| Other | 5.79 | 5.94 | 5.60 | |
| Married | 56.14 | 54.24 | 58.61 | 0.260 |
| Insurance status > 30 days of diagnosis | 0.001 | |||
| Medicare | 59.22 | 56.25 | 63.07 | |
| Medicaid | 8.57 | 7.89 | 9.46 | |
| Private/tricare | 25.43 | 25.93 | 24.79 | |
| VA/IHS/other | 1.49 | 1.76 | 1.14 | |
| Missing/no insurance | 5.29 | 8.17 | 1.55 | |
| Number of comorbid conditions | 0.174 | |||
| 0 | 62.54 | 65.32 | 58.92 | |
| 1 | 25.92 | 24.66 | 27.56 | |
| 2+ | 11.54 | 10.02 | 13.52 | |
| Smoking status | 0.002 | |||
| Never smoked | 33.70 | 34.77 | 32.30 | |
| Current smoker | 17.03 | 18.17 | 15.56 | |
| Former smoker | 45.66 | 41.45 | 51.15 | |
| Unknown | 3.60 | 5.61 | 0.99 | |
| Obesity | 0.139 | |||
| Underweight or healthy weight | 32.42 | 31.15 | 34.09 | |
| Overweight | 34.37 | 32.56 | 36.73 | |
| Obese | 33.21 | 36.30 | 29.19 | |
| Vital status at last Follow-up | < 0.001 | |||
| Alive | 94.49 | 97.28 | 90.86 | |
| Dead | 5.51 | 2.72 | 9.14 | |
| Region | < 0.001 | |||
| Northeast | 9.00 | 12.13 | 4.92 | |
| Midwest | 7.36 | 7.58 | 7.07 | |
| South | 22.13 | 25.98 | 17.11 | |
| West | 61.52 | 54.31 | 70.90 | |
| Tumor characteristics | ||||
| Stage at diagnosis | < 0.001 | |||
| Stage 0 | 55.94 | 67.01 | 41.54 | |
| Stage I | 23.82 | 23.50 | 24.23 | |
| Stage II | 12.53 | 6.76 | 20.04 | |
| Stage III or IV | 7.70 | 2.72 | 14.19 | |
| Upper urinary tract involvement | 1.89 | 1.20 | 2.79 | 0.086 |
| Site of metastases | ||||
| Bone | 0.56 | 0.37 | 0.80 | 0.600 |
| Distant lymph nodes | 1.00 | 0.00 | 2.20 | < 0.001 |
| Lung | 0.82 | 0.12 | 1.73 | 0.009 |
| Other | 0.63 | 0.00 | 1.41 | < 0.001 |
| Treatment characteristics | ||||
| Treatment protocol registration 1 | < 0.001 | |||
| No/refused/unknown | 97.88 | 99.31 | 96.01 | |
| Yes | 2.12 | 0.69 | 3.99 | |
| Primary surgery type 2 | < 0.001 | |||
| Other OR no surgery | 4.13 | 3.25 | 5.27 | |
| Radical cystectomy | 6.09 | 1.61 | 11.91 | |
| Local excision by electrocautery | 16.56 | 17.86 | 14.87 | |
| TURBT | 73.22 | 77.27 | 67.94 | |
| Any radiation therapy | 6.06 | 3.31 | 9.64 | 0.001 |
| Number of intravesical therapy agents received | 0.938 | |||
| 0 | 51.12 | 51.73 | 50.34 | |
| 1 | 35.18 | 34.72 | 35.77 | |
| 2+ | 13.70 | 13.55 | 13.89 | |
| Number of oral or parenteral systemic therapy agents received | < 0.001 | |||
| 0 | 85.44 | 92.15 | 76.71 | |
| 1 | 6.17 | 4.57 | 8.26 | |
| 2+ | 8.39 | 3.28 | 15.03 | |
| Hospital characteristics | ||||
| Bed size 3 | 0.055 | |||
| 1–299 beds | 46.74 | 49.11 | 43.56 | |
| 300–499 beds | 20.17 | 21.91 | 17.82 | |
| ≥ 500 beds | 27.87 | 23.70 | 33.47 | |
| Other | 5.22 | 5.29 | 5.14 | |
| Approved residency training | 0.136 | |||
| No/unknown | 34.68 | 37.14 | 31.48 | |
| Yes | 65.32 | 62.86 | 68.52 | |
| Hospital ownership 4 | 0.014 | |||
| government, nonfederal | 15.96 | 15.66 | 16.35 | |
| Non-government, not-for-profit | 68.20 | 65.38 | 71.88 | |
| Non-government, for-profit; physician office | 14.98 | 17.48 | 11.73 | |
| Government, federal | 0.51 | 0.91 | 0.00 | |
| Unknown | 0.34 | 0.57 | 0.00 | |
| TPS | 0.120 | |||
| 0–28.5 or unknown | 30.10 | 31.61 | 28.13 | |
| > 28.5–34.2 | 21.12 | 18.97 | 23.92 | |
| > 34.2–39.7 | 21.09 | 19.22 | 23.53 | |
| > 39.7–47.3 | 15.57 | 17.99 | 12.42 | |
| > 47.3 | 12.12 | 12.21 | 12.00 | |
| Star rating | 0.774 | |||
| 1–2 or unknown | 12.35 | 12.69 | 11.91 | |
| 3 | 61.99 | 60.79 | 63.51 | |
| 4–5 | 25.66 | 26.51 | 24.58 | |
| Oncology average Length of stay (days) | 0.069 | |||
| 0–5.25 | 33.14 | 30.81 | 36.17 | |
| > 5.25–8.48 | 39.25 | 40.03 | 38.24 | |
| > 8.48 | 9.08 | 7.83 | 10.72 | |
| Unknown | 18.52 | 21.33 | 14.87 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree