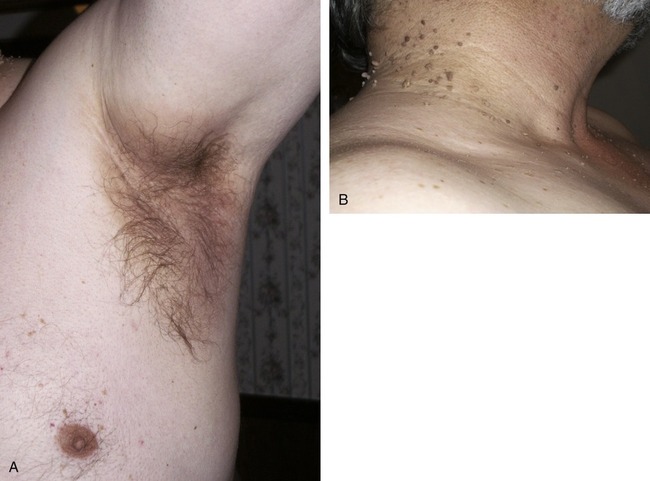
After completing this chapter, you should be able to: • Describe the metabolic syndrome. • Identify individuals at risk for the metabolic syndrome. • Recognize an appropriate lifestyle plan for preventing and managing insulin resistance. • Explain the application of the Dietary Guidelines in managing insulin resistance. Obesity, associated with the metabolic syndrome, is now an epidemic throughout the world. The medical community faces an emerging epidemic of health problems found with the metabolic syndrome, including type 2 diabetes developing among children and adolescents and early cardiovascular morbidity and mortality. In a group of obese children, 40% were found to have hyperinsulinemia (see below), and over 10% had impaired glucose tolerance (elevated blood glucose level) based on an oral glucose tolerance test. The metabolic syndrome was found in 30% of children under 12 years of age (Viner and colleagues, 2005). An estimated 41 million individuals in the United States have prediabetes (high levels of blood glucose, but not in the diabetes range [see Chapter 8], a risk factor found with the metabolic syndrome). About one third of persons with insulin resistance go on to develop type 2 diabetes. The World Health Organization (WHO) has estimated that there will be around 300 million persons with diabetes by 2025. It is anticipated that Asia will be at the forefront of high rates of diabetes in years to come because of a genetic tendency for insulin resistance along with changing lifestyles. One study found Chinese adolescents currently have metabolic syndrome at a rate of less than half of the estimated 10% of U.S. adolescents. However, among overweight Chinese adolescents living in the United States the rate of insulin resistance is the same (Li and colleagues, 2008). The rate of insulin resistance in some populations is as high as 60% but is generally lower in the United States at large, with an estimated 25% of the population with insulin resistance. Insulin resistance is sometimes referred to as the common gene theory. This is because it is the underlying cause of many chronic health problems. Costs associated with the metabolic syndrome run into billions of dollars to the U.S. economy in lost work hours alone (Sullivan and colleagues, 2007). 1. Central obesity (waist size equivalent to greater than 40 inches in men; greater than 35 inches in women) 2. Hypertension (high blood pressure) 3. Dyslipidemia (altered blood lipids with high levels of triglycerides and low levels of high-density lipoprotein (HDL) cholesterol; see also Chapter 7) There are several definitions, and health conditions, used to diagnose the metabolic syndrome, the differences being primarily for accurate reporting of research outcomes. It has been suggested the term be applied to persons without type 2 diabetes or cardiovascular disease with the goal to prevent these conditions. The metabolic syndrome can be a better predictor of future diabetes than fasting blood glucose (FBG) levels alone (Lorenzo and colleagues, 2007). The National Cholesterol Education Program’s (NCEP’s) Adult Treatment Panel (ATP) III definition of metabolic syndrome uses the easily measured clinical finding of increased waist size. Similar criteria of the ATP III guidelines are used by the American Association of Clinical Endocrinologists (see below). The 2005 International Diabetes Federation (IDF) definition of the metabolic syndrome was designed to be useful worldwide. It is similar to the definition of the NCEP. WHO has another, but similar, definition. Four primary elements identified by the IDF are as follows: • Glucose intolerance (fasting glycemia greater than or equal to 5.6 mmol/L; greater than 100 mg/dL) • Obesity or overweight body mass index (BMI) greater than 25 (the BMI is a mathematical formula used to describe level of body fatness; especially with central obesity or metabolic obesity—carrying weight in the abdomen; see measurements above or having a high waist-to-hip ratio; see Chapter 6 for use of BMI) • Elevated triglycerides: 150 mg/dL (1.69 mmol/L) • Elevated blood pressure greater than or equal to 130/85 mm Hg • 2-hour postglucose challenge greater than 140 mg/dL to 199 mg/dL (prediabetes) • Fasting glucose between 110 and 126 mg/dL (6.15 and 7.05 mmol/L; prediabetes) • Family history of type 2 diabetes, hypertension, or cardiovascular disease (CVD) • Polycystic ovary syndrome (PCOS) —see section later in this chapter Diagnosis depends on clinical judgment of a health provider based on risk factors. Other conditions are being attributed in some manner to the metabolic syndrome. Increased inflammation as evidenced by elevated levels of the laboratory value high-sensitivity C-reactive protein (CRP) is found with the metabolic syndrome. In obese children and adolescents elevated CRP appears related to the cause of diabetes development (Yang and colleagues, 2006). Another laboratory value that may be used in diagnosing insulin resistance is to measure the level of hyperinsulinemia present. This can be determined with a high level of insulin production in relation to FBG level (FBG/insulin ratio less than 7). Fasting insulin level was found to be the best predictor of the metabolic syndrome among a study of European and African women, although for other conditions found with the metabolic syndrome dyslipidemia was more associated with European heritage and hypertension with African heritage (Gower and colleagues, 2007). An indirect measure of insulin production is C-peptide level. Acanthosis nigricans is a skin condition with dark patches that is related to diabetes (see Figure 5-1, A, and Chapter 8). Cutaneous papillomas, or “skin tags,” are also found with insulin resistance and type 2 diabetes (Figure 5-1, B). This is due to hormonal changes found with the metabolic syndrome. A decreased plasma level of the hormone adiponectin was found associated with insulin resistance in nondiabetic relatives of an African American family with a strong family history of diabetes (Osei, Gaillard, and Schuster, 2005). Nerve disease is known to occur with uncontrolled diabetes. It appears there is an increased risk of nerve disease even without diabetes, but with low levels of HDL-C. This has been noted as a form of neuropathy with reduced length of dendrite nerve fibers (Pittenger and colleagues, 2005). Mild and moderate renal insufficiency (see Chapter 9) is relatively common in the United States. Chronic renal insufficiency is now considered a public health priority, and the number of components of the metabolic syndrome is proportional to the prevalence of chronic renal insufficiency (Zoccali, Caridi, and Cambareri, 2007). Increased rates of depression have long been known among persons with diabetes. Newer evidence is linking increased inflammation, as found with the metabolic syndrome, with depression. It appears there is a changed metabolism of the amino acid tryptophan related to altered enzyme functioning, resulting in less serotonin production. This altered metabolism of tryptophan seems to be the cause of major depression, postnatal depression, and anxiety states commonly found with conditions associated with the metabolic syndrome (Maes and colleagues, 2007). A study of persons with Meniere’s disease found the majority had hyperinsulinemia. It is suggested a 5-hour glucose tolerance test using 100-g glucose load and insulin levels be routinely included when investigating Meniere’s disease (DAvila and Lavinsky, 2005). Certain cancers have been associated with the metabolic syndrome. Known cancers related to the metabolic syndrome include cancers of the breast, pancreas, liver, and colon and uterine (endometrial) cancer. Newer research has linked prostate and ovarian cancers with the metabolic syndrome (see Chapter 10). Another health problem that has been connected with the metabolic syndrome and insulin resistance includes nonalcoholic fatty liver disease (NAFLD)—a condition of fat buildup in the liver (Brea and colleagues, 2005). This is a major form of chronic liver disease in adults and children. It is one of the consequences of the current obesity epidemic and can progress to nonalcoholic steatohepatitis (NASH), characterized by steatosis (fatty degeneration), inflammation, and progressive fibrosis, ultimately leading to cirrhosis and end-stage liver disease. The factors implicated in this progression are poorly understood. NASH is closely associated with obesity and the metabolic syndrome. An elevated liver enzyme, alanine transaminase (ALT) (a marker of NAFLD), was observed in about 5% of adolescents of African heritage, in over 7% of white adolescents, and in 11% of Mexican American adolescents. Males had the highest levels, at over 12%, with females at 3.5%. A high waist circumference, evidence of inflammation, and high triglyceride levels were associated. Screening for NAFLD is advised for adolescents exhibiting evidence of the metabolic syndrome (Fraser and colleagues, 2007). A person with a genetic predisposition to insulin resistance tends to have an altered insulin response. With insulin resistance there is often a delayed production of meal-related insulin. This can result in a transient state of hyperglycemia (high levels of blood glucose). When the body does respond to the hyperglycemia, it is often with excess insulin production over a prolonged period. Persons with insulin resistance have been noted to produce up to 10 times the amount of insulin to control blood glucose levels as compared with other insulin-sensitive individuals. This hyperinsulinemia can result in symptoms of hypoglycemia (low levels of blood glucose; see Chapter 8) if meals are delayed. The symptoms of reactive hypoglycemia are common among persons with insulin resistance, but medically the condition is rarely diagnosed. The blood glucose criteria for diagnosis of reactive hypoglycemia are more stringent than for persons with diabetes on medication. Physicians generally will not make the diagnosis unless blood glucose levels are below 50 mg/dL. Symptoms of hypoglycemia, however, may occur years before the onset of diabetes and are likely because of hyperinsulinemia and excess release of counterregulatory hormones (see Chapter 4). The symptoms of hypoglycemia affect the quality of life. However, most persons with hypoglycemia symptoms are not in an immediate health emergency. Severe hypoglycemia requiring medical assistance is usually limited to persons taking insulin or insulin-stimulating medications such as the sulfonylurea medications (see Chapter 8). Hyperinsulinemia is found with central obesity. It is still, however, a bit of a chicken-and-egg question. Which came first? Hyperinsulinemia and central obesity are known to worsen insulin resistance. However, it may be that the genetic predisposition to insulin resistance is what first sets up excess production of insulin in relation to carbohydrate intake. Some health care professionals suggest that hyperinsulinemia encourages the gain of abdominal weight in the first place. This is the basis of the low-carbohydrate diets (see Chapter 6). With regard to dyslipidemia (see Chapter 7), it has been clearly shown that the enzyme lipoprotein lipase (an enzyme that helps the breakdown of triglycerides) is altered in the presence of hyperinsulinemia. This results in reduced breakdown of triglycerides, leading to high serum triglyceride levels. Thus elevated triglyceride levels in the blood are generally associated with hyperinsulinemia, especially if the person also has central obesity. This occurs even in childhood, with triglyceride levels correlating with insulin levels in children (Reinehr, Kiess, and Andler, 2005). Triglycerides can reach very high levels. Once the level is over 3000 mg/dL, distinct visual demarcation can be found between the red blood and the white fat in the blood (Figure 5-2). Reduction of hyperinsulinemia generally improves dyslipidemia. It may be helpful for persons with type 2 diabetes and CVD to understand the common connections of insulin resistance and hyperinsulinemia. Because atherosclerosis (see Chapter 7) generally is noted before the diagnosis of diabetes, it is believed that hyperinsulinemia related to insulin resistance promotes the plaque buildup. Hypertension is now a well-recognized aspect of insulin resistance and the metabolic syndrome. There are still unanswered questions regarding the specific mechanism related to hypertension and the underlying cause of insulin resistance. The role of hyperinsulinemia is being suggested as the link, as a result of altered vasodilation. In a study of rats it was found acute hyperglycemia and hyperinsulinemia caused constriction of blood vessels that may be related to hypertension (Zamami and colleagues, 2008). Advice to follow a low-glycemic index diet may contribute to management of hypertension (Kopp, 2005
Insulin Resistance and the Metabolic Syndrome
INTRODUCTION
WHAT IS THE METABOLIC SYNDROME?
WHAT IS THE ROLE OF HYPERINSULINEMIA IN THE METABOLIC SYNDROME?
REACTIVE HYPOGLYCEMIA
OBESITY
HYPERTENSION
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Insulin Resistance and the Metabolic Syndrome