matching, source of stem cells, and GVHD prophylaxis) that result in very different infectious disease risk profiles. Early after HSCT, neutropenia and mucositis are the main host defense defects. Following engraftment, the most important risk factor for infection is the occurrence of severe GVHD and its treatment. Active GVHD is associated with immune dysregulation, may be accompanied by cytomegalovirus (CMV) reactivation or disease, and it is also an independent risk factor for mold infection (15). CMV disease delays immune reconstitution and is associated with an increased risk of bacterial and fungal infections (16).
TABLE 37.1 Selected risk factors for infection in patients with advanced cancer | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||
phagocytic function and cell-mediated immunity. Infections are a frequent complication of corticosteroid use, and differences in the type and frequency of infections are dependent on the dose and duration of treatment (19). Bacterial infections are most common (20); but opportunistic fungal, viral, and mycobacterial infections are also seen, particularly with high doses and long durations of systemic corticosteroids.
invasive diagnostic procedures. In this regard, it may be reasonable to continue prophylactic measures that are adequate to the clinical condition (e.g., antibiotics during neutropenia and opportunistic infection prophylaxis in recipients of stem cell transplantation) and administer the immunizations recommended by the American College of Physicians (ACP) to both patients and caregivers (http://www.acponline.org/clinical_information/resources/adult_immunization/).
A complete blood cell count (CBC) and differential cell counts. The presence of an elevated white blood cell count or a left shift increases the probability of an ongoing bacterial infection. Similarly, the presence of neutropenia significantly increases the risk of bacterial or fungal infection.
Urianalysis, and if abnormal a urine culture. Urine culture should be ordered in patients with unexplained fever, altered mental status, and/or typical signs and symptoms of urinary tract infection such as pyuria, hematuria, dysuria, worsening urinary incontinence, and/or suprapubic pain (43). Asymptomatic bacteriuria does not require treatment. A dipstick urine test with a positive leukocyte esterase, nitrites, and/or pyuria should also prompt a urine culture. Appropriately collected urine culture specimens include a midstream or clean catch urine, or in patients with urethral catheters, cultures should be drawn after the removal of the catheter and insertion of a new one (44).
Blood cultures. When available blood cultures should be drawn in all advanced cancer patients in whom an infection is suspected (2). Although, in general peripherally drawn blood cultures are more reliable, if a catheter is in place, blood for culture should be drawn from the catheter. Blood from peripheral sticks should be obtained in individualized cases in which the suspicion of a catheter-related infection is very high, and positive results would impact the management of the patient.
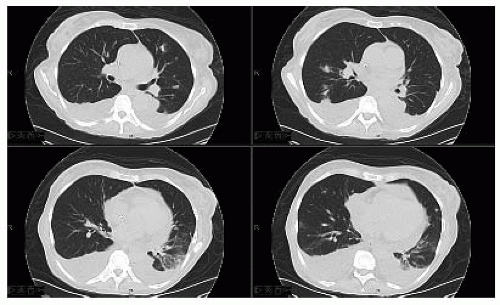
Pulse oximetry and chest x-ray. To evaluate for pneumonia, heart failure, and pulmonary embolism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree