I. ETIOLOGY OF INFECTIONS IN PATIENTS WITH CANCER
A. General considerations
Infections develop in patients with cancer as the result of quantitative or qualitative defects in their innate or adaptive host defense systems. Among these components are circulating phagocytic cells, cell-mediated immunity (CMI), circulating immunoglobulins, the reticuloendothelial system (RES), endogenous cytokines, intact mucocutaneous barriers, and patency of hollow visci. Defects commonly occur in more than one system of innate and adaptive host defenses due to a multitude
of etiologies, including the underlying malignancy and its treatment. Alterations of these host defense systems increase the risk for development of specific infections. The relationship between altered host defenses and infections caused by specific pathogens is delineated in Table 27.1.
B. Circulating phagocytic cells
Neutrophils (PMNs) and monocytes are key effector cells of the innate host defense system against most bacterial and fungal pathogens encountered in patients with cancer. Neutropenia (defined as an absolute neutrophil count [ANC] of < 500 PMNs/μL) increases the risk of infection in direct relation to its duration and depth. Patients with persistent neutropenia (defined as > 10 days) or those with profound neutropenia (<100 PMNs/μL) have a markedly increased risk of developing serious bacterial and fungal infections. Neutropenia may develop as the direct result of a leukemic process infiltrating normal bone marrow with suppression of myelopoiesis or following cytotoxic chemotherapy. Development of mucositis in association with chemotherapy-induced neutropenia further increases the risk of infection. Neutropenia is associated with an increased risk of development of life-threatening infections caused by the endogenous mucocutaneous bacterial flora, as well as Candida spp. from the alimentary tract and Aspergillus spp. and other filamentous fungi from the external environment.
C. Cell-mediated immunity (CMI)
Altered CMI may result from the primary neoplastic process, such as Hodgkin lymphoma or hairy cell leukemia, or from therapeutic interventions, such as corticosteroids and fludarabine. Although fludarabine may induce a profound depletion of CD4 lymphocytes (T-helper cells), corticosteroids have less of an effect on the absolute number while still profoundly compromising their function. Altered CMI is associated with an increased risk of infections caused by intracellular bacterial pathogens (e.g., Listeria monocytogenes, Mycobacterium spp., and Salmonella spp.), many fungal organisms (e.g., Pneumocystis, Cryptococcus neoformans, Histoplasma capsulatum), and DNA viruses (e.g., varicella zoster virus [VZV], cytomegalovirus [CMV], Epstein-Barr virus [EBV]). As corticosteroids also affect PMN, monocyte, and macrophage function, invasive aspergillosis may also develop in patients receiving sustained and elevated dosages.
D. Circulating immunoglobulins
Hypogammaglobulinemia or dysimmunoglobulinemia may develop in patients with multiple myeloma or chronic lymphocytic leukemia. These defects in adaptive immunity are strongly associated with infections caused by encapsulated bacteria, particularly Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis.
TABLE 27.1 Relationship Between Altered Host Defenses and Organisms Causing Infection in Patients with Cancer
Altered Host Defense
Gram-Positive Bacteria
Gram-Negative Bacteria
Fungi
Viruses
Other Pathogens
Neutropenia
Staphylococcus species (e.g., S. aureus, coagulase-negative staphylococci)
α-hemolytic streptococci (e.g., Streptococcus mitis)
Enterococcus faecalis and E. faecium
Enterobacteriaceae (e.g., Escherichia coli, Klebsiella spp., Enterobacter spp.)
Pseudomonas aeruginosa
Candida species (e.g., C. albicans, C. tropicalis, and C. glabrata)
Aspergillus, spp.
Mucorales
Fusarium spp.,
Scedosporium spp.
Trichosporon spp.
HSV (associated with chemotherapyinduced mucositis)
Decreased cell-mediated immunity
Nocardia spp.
Listeria monocytogenes
Salmonella spp.
Legionella spp.
Pneumocystis, Cryptococcus neoformans
Histoplasma capsulatum
Coccidioides spp.
HSV
VZV
CMV
EBV
Mycobacterium spp. (e.g., M. tuberculosis, M. avium complex)
Toxoplasma gondii
Strongyloides stercoralis
Hypogammaglobulinemia, dysimmunoglobulinemia, or asplenia
Streptococcus pneumoniae
Haemophilus influenzae
Neisseria meningitidis
Capnocytophaga canimorsus
—
—
Plasmodium falciparum
Ehrlichia chaffeensis
Anaplasma phagocytophilum
Babesia microti
Disruption of mucocutaneous barriers
Vascular catheters
Coagulase-negative staphylococci
S. aureus
P. aeruginosa Acinetobacter baumannii
Stenotrophomonas maltophilia
Candida species*
—
—
Mucositis of the alimentary tract
α-hemolytic streptococci (e.g., S. mitis)
Enterococcus spp.
Clostridium septicum
E. coli
Klebsiella spp.
Enterobacter spp.,
P. aeruginosa
Candida species
—
—
Postoperative wounds
Coagulase-negative staphylococci
S. aureus
Group A streptococci
Enterobacteriaciae
—
—
—
Urinary tract catheters
Enterococcus spp.
Enterobacteriaciae, P. aeruginosa
—
—
—
Obstruction of hollow visci
Aerobic and anaerobic respiratory, gastrointestinal, and genitourinary bacterial flora
Aerobic and anaerobic respiratory, gastrointestinal, and genitourinary bacterial flora
—
—
—
CMV, cytomegalovirus; EBV, Epstein-Barr virus; HSV, herpes simplex virus; VZV, varicella zoster virus.
* The portal of entry of Candida spp. in most neutropenic patients is thought to be the gastrointestinal tract.
E. Reticuloendothelial system (RES)
Alterations of the RES most commonly develop as the result of splenectomy. Among its important functions, the spleen serves as a mechanical filter for removing opsonized or nonopsonized bacterial pathogens, as well as a setting for IVIG production. There is an increased risk in splenectomized patients for development of fulminant infections caused by S. pneumoniae, H. influenzae, Capnocytophaga canimorsus, Babesia microti, Ehrlichia chaffeensis, Anaplasma phagocytophilum, and Plasmodium falciparum.
F. Endogenous cytokines and chemokines
An elaborate network of immunoregulatory cytokines and chemokines regulates the effector cells of the innate host defense systems. These molecules mediate their effect through an intricate system of cell surface receptors. The expanding use of monoclonal antibodies to inhibit immunoregulatory molecules and their receptors has resulted in new forms of immunosuppression. For example, infliximab, which binds to tumor necrosis factor (TNF)-α, is associated with an increased risk of tuberculosis and histoplasmosis.
G. Intact mucocutaneous barriers
Cytotoxic chemotherapy, particularly regimens containing cytarabine, high-dose methotrexate, and etoposide, may cause severe mucosal disruption, which may result in the translocation of pathogenic endogenous bacterial and fungal pathogens, such as Escherichia coli, Klebsiella pneumoniae, and Candida spp., from the intestinal tract or Streptococcus mitis from the oral cavity. Vascular catheters disrupt the normal cutaneous barriers and provide a conduit for staphylococci to enter the bloodstream.
Normal bacterial flora further contribute to mucosal host defense by suppressing the growth of more pathogenic organisms. Use of broad-spectrum antibacterial agents may reduce the normal bacterial flora and allows more resistant organisms to fill the void on mucosal surfaces. Normal gastrointestinal flora also protect against the emergence of Clostridium difficile colitis. Prior use of broad-spectrum antibiotics is the strongest predictive variable for the development of C. difficile colitis in numerous studies.
H. Obstruction of hollow visci
Solid tumors or lymphoid malignancies that obstruct the upper and lower respiratory tract, biliary tree, intestines, and urinary tract result in accumulation of bacteria that are normally cleared by these structures. Obstructions in the upper respiratory tract may result in sinusitis and in the lower respiratory tract as postobstructive pneumonia caused by respiratory flora, including anaerobes. Obstructions of the gastrointestinal and biliary tract may result in polymicrobial bacteremia and ascending cholangitis. By comparison, obstruction of the urinary tract is more often associated with aerobic gram-negative bacteremia.
II. DIAGNOSIS OF INFECTIONS IN PATIENTS WITH CANCER
A. General overview
The initial assessment of possible infection in a patient with cancer includes a careful history assessing risks and symptoms, physical examination assessing for hemodynamic stability and localizing signs, and prompt completion of a laboratory diagnostic evaluation. As early symptoms and signs of infection are attenuated in immunocompromised patients, attention to subtle details in history and physical exam are important. Any clinical features suggesting infection in an immunocompromised patient with cancer should prompt initiation of broad-spectrum antibiotics. For example, the presence of localizing abdominal pain in a neutropenic patient in the absence of fever should prompt the initiation of empirical antibacterial therapy. The clinical assessment of immunocompromised febrile patients with cancer should attempt to localize the possible source of infection. Clinical localization helps to guide therapy for likely pathogens.
B. Clinical history
The clinical history is directed toward elucidating risk factors for infection and localizing symptoms. Immunocompromised patients may have minimal symptomatic findings. Deep-seated infection may present as simply fever and malaise. Pneumonia in a neutropenic patient may present initially with only mild dyspnea or cough. Patients should be queried for any history of localizing pain.
Suspected infection in neutropenic patients constitutes a medical emergency. Understanding the patient’s current immune deficits is important and can guide therapy.
1. Cancer treatment. Understanding the current underlying neoplastic process and current therapy will help to assess a patient’s immune status.
a. Chemotherapeutic and biologic agents. Many commonly used chemotherapeutic drugs are cytotoxic, resulting in significant lymphopenia and/or neutropenia. The duration, severity, and type of myelosuppression can be related to the type of chemotherapeutic agent, the amount of drug exposure, and the underlying degree of myelosuppression.
(1) Neutropenia. Alkylating agents, anthracyclines, cytarabine, methotrexate, carboplatin, busulfan, 5-fluorouracil, and nitrosoureas are examples of drugs that commonly cause dose-dependent neutropenia, depending on the protocol.
(2) Cluster of differentiation 4 (CD4) and 8 cell suppression (cellular immune system suppression). The following chemotherapeutic agents may result in prolonged suppression of the T-helper/suppressor arm of the immune system:
Alemtuzumab: median duration of lymphopenia is 28 days
Corticosteroids: severe T-cell function suppression can be seen with a dose equal to or more than 15 mg prednisone/day for a month or more.
Purine analogs (cladribine, fludarabine, and pentostatin) may result in CD4 cell count suppression to 200 or less for several years after therapy.
(3) Suppressed B-cell function (altered humoral immunity). The following chemotherapeutic and biologic agents may cause suppression of antibody production by B cells:
Alkylating agents (cyclophosphamide, chlorambucil, melphalan)
Corticosteroids: use of greater than 40 mg/day of prednisone equivalent may decrease antibody production
Methotrexate
Rituximab
(4) Cytokine suppression. Infliximab, adalimumab, and etanercept may be used in autoimmune diseases or for graft-versus-host disease in recipients of hematopoietic stem cell transplantation (HSCT). Such agents result in altered TNF-α response with an increased risk of infections with conditions such as tuberculosis, histoplasmosis, and aspergillosis.
2. Type of malignancy
a. Solid tumors. These malignancies can cause significant obstruction in affected tissues, leading to infection behind the obstruction. For example, postobstructive pneumonias are common in patients with bronchogenic carcinomas. Colonic carcinomas may cause obstruction or perforation and may simulate diverticular abscesses. Tissue necrosis secondary to malignancy may also create an area of potential sequestrum, which can become infected during an episode of bacteremia or from translocation of bacteria from a normally nonsterile area to a sterile area. For example, hepatic metastases may serve as a nidus for recurrent bacteremias of enteric gram-negative bacteria. Some solid tumors may mimic an infectious etiology without any microbial involvement, such as the presence of fever and malaise in a patient with renal cell carcinoma.
b. Hematologic malignancies. Leukemias and lymphomas may cause severe immunodysregulation. Lymphoblastic leukemias and lymphomas also may cause B symptoms, including fever. In contrast, fever associated with nonlymphocytic leukemias is usually caused by an infection complicating neutropenia rather than B symptoms.
C. Clinical evaluation
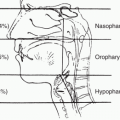
The physical examination should be thorough with special emphasis on areas of symptomatology and likely mucocutaneous portals
of entry. Like the clinical history, the review of systems and clinical examination can present with subtle or atypical findings in the presence of severe infection. Special attention should be directed to the following areas and potential infectious etiologies.
1. Review of systems/symptoms of infection
Head, eyes, ears, nose, and throat (HEENT): changes in vision, ear or sinus discomfort, oral lesions, changes in dentition
Lungs: cough, hemoptysis, shortness of breath, pleuritic chest pain
Abdomen: dysphagia, odynophagia, abdominal pain, perianal pain or pruritus, bleeding, diarrhea, nausea or vomiting
Skin: any new skin lesions or skin changes
Genitourinary (GU) system: urinary frequency, dysuria, urinary urgency, hematuria, GU discharge, flank tenderness, decreased urination
Central nervous system (CNS): altered mental status, new onset focal deficits, seizures
Catheter sites: redness, tenderness at the insertion site including along the subcutaneous tract of the catheter.
2. Signs of infection in immunocompromised patients with malignancy may be subtle or atypical, so a thorough physical examination focusing on changes or alteration in function is essential. Special attention should be directed to the areas listed in Table 27.2 and the associated potential etiologic agents.
a. HEENT
(1) Ophthalmic assessment. Hemorrhages; necrosis of the retina; yellow lesions adjacent to scarred retina (“headlight in fog”); white, infiltrative lesions on the retina; chorioretinitis with retinal detachment; or fulminant endophthalmitis are all signs of serious infection. New anisocoria or extraocular muscle palsy suggests a space-occupying lesion, cavernous sinus infection, or orbital infiltrative process.
(2) Paranasal sinuses. Sinus tenderness, orbital cellulitis, or edema can indicate bacterial or fungal infection of the sinuses. Black material along the nasal turbinate mucosa may indicate mucormycosis.
(3) Oropharynx and dentition. Bacterial infections, especially anaerobic infections, may present with marginal gingivitis, loosened teeth, pain or discomfort in the teeth or gums, or referred pain to the sinus area in addition to frank abscess formation. The presence of a draining sinus tract may be significant for Actinomycosis. Hemipalatal erythema suggests ipsilateral maxillary sinus infection involving the palatine blood vessels. Ulcerations can be caused by a variety of infectious agents, including viruses, fungi, and Mycobacterium tuberculosis. Viral ulcerations
are generally shallow and painful, and may have extensive oropharyngeal involvement in the patient with cancer. The viruses that usually cause ulcerations are the herpes viruses and coxsackie viruses (herpangina). Fungal infections such as histoplasmosis may present with painful, deep ulcers with heaped up edges. Candida can present with characteristic white plaques on the buccal mucosa (thrush) or, less commonly, erythema of the mucosal surfaces or angular cheilitis.
TABLE 27.2 Potential Etiologic Agents of Infection and Associated Signs and Symptoms in Immunocompromised Oncology Patients
Clinical Change
Potential Etiologic Agent
HEENT
Changes in vision
Retinal hemorrhage
Staphylococcus aureus (endocarditis), CMV, and in neutropenic hosts Candida spp. or Aspergillus spp.
Retinal necrosis
HSV, VZV
Retinal exudate with scarring
Toxoplasmosis
Vitreal opacities (non-neutropenic patients), chorioretinitis, or endophthalmitis
Candida spp., Trichosporon spp., Histoplasma capsulatum
Sinus tenderness
Black discharge or orbital cellulitis/edema
Mucormycosis (zygomycosis)
Oropharynx
Painful, bleeding gums, marginal gingivitis
Oral anaerobes
Ulcerations
Shallow, painful
HSV, coxsackievirus
Deep, painful
Histoplasmosis
Erythema or white plaques
Candida
Cardiovascular
Murmur or line infection
Staphylococcus epidermidis, S. aureus
Chest pain, dyspnea, pleural rub, pericarditis
Aspergillus spp., Streptococcus pneumoniae, S. aureus, coxsackievirus
Pulmonary
Consolidation
S. pneumoniae, Legionella spp., Haemophilus influenzae, Pseudomonas aeruginosa, Aspergillus spp., or other angioinvasive mold
Diffuse interstitial pattern/patchy alveolar infiltrate
CMV, PCP, Mycoplasma, other viruses (e.g., influenza, adenovirus)
Nodule, halo sign, wedge-shaped infiltrate, crescent sign
Aspergillus spp, Mucorales, Fusarium spp., Scedosporium spp., other angioinvasive mold, P. aeruginosa
Postobstructive
Anaerobes + gram-negative bacilli S. aureus, P. aeruginosa
Abdomen
Pain, nausea/vomiting—suspect typhlitis
Polymicrobial: gram-positive cocci, gram-negative bacilli, anaerobes
Perianal or rectal discomfort—suspect anorectal infection
Polymicrobic; gram-positive cocci, gram-negative rods, anaerobes
Diarrhea
Clostridium difficile
Skin
Petechiae/purpura
Coxsackievirus, echovirus, CMV, Neisseria meningitidis, Haemophilus spp., Rickettsia spp., S. aureus, S. pneumoniae, Capnocytophaga canimorsus, Listeria monocytogenes
Macules/papules
Pseudomonas and other gram-negative rods, S. aureus, Rickettsia spp., Candida, Aspergillus, endemic mycosis, viral infections (multiple), mycobacterium
Vesicles/bullae
VZV, HSV
Ecthyma gangrenosum
Pseudomonas spp., Aspergillus spp., Mucorales, Fusarium spp., Scedosporium spp., Vibrio vulnificus and other gram-negative bacilli, S. aureus
Lines
Pain, swelling, erythema
S. aureus, Candida, Gram-negative bacilli (e.g., Pseudomonas), coagulasenegative Staphylococcus spp.
CMV, cytomegalovirus; HEENT, head, eyes, ears, nose, and throat; HSV, herpes simplex virus; PCP, Pneumocystis pneumonia; VZV, varicella zoster virus.
b. Cardiovascular system. The presence of new murmurs or suspected line infections should prompt an evaluation for endocarditis. The most common cause of endocarditis in this population is Staphylococcus aureus. Pericarditis and pericardial tamponade are uncommon, but should be suspected in patients with chest pain, shortness of breath, fever, and/or pericardial rub. A variety of infectious agents can cause pericarditis, including common agents such as S. aureus, S. pneumoniae, and coxsackie viruses and less common agents such as Candida spp. and Aspergillus spp., and the Mucorales in patients with cancer with prolonged neutropenia or corticosteroids.
c. Lungs. Signs of consolidation and/or pleural effusion may indicate the presence of pneumonia (including postobstructive pneumonia). In neutropenic hosts, pneumonia may present with minimal changes on examination. Also, atypical pulmonary infections such as Pneumocystis pneumonia (PCP) can present initially with minimal or no changes on pulmonary examination.
Infections: Etiology, Treatment, and Prevention
Infections: Etiology, Treatment, and Prevention
Thomas J. Walsh
Joan M. Duggan
Infectious diseases are an important cause of morbidity and mortality in immunocompromised patients with cancer. Advances in the diagnosis, treatment, and prevention of these infections have been critical in improving outcome of oncology patients, particularly those with hematologic malignancies. The critical components of infectious disease supportive care include the following: recognition of risk factors that impair host defenses, understanding of the likely pathogens and their resistance patterns within one’s own institution, meticulous diagnostic evaluation of symptomatic or febrile patients, and prompt initiation of a rationally based antimicrobial regimen that is active against the most likely microorganisms.