Number of new cases
Number attributable to infection
Attribute fraction (%)
Worldwide
14,000,000
2,200,000
15.4
Africa
Sub-Saharan Africa
630,000
200,000
31.3
North Africa and west Asia
540,000
70,000
13.1
Asia
Central Asia
1,500,000
290,000
19.4
East Asia
4,900,000
1,100,000
22.8
America
Latin America
1,100,000
160,000
14.4
North America
1,800,000
72,000
4.0
Europe
3,400,000
250,000
7.2
Oceania
160,000
7600
4.9
Human development index
Very high
5,700,000
430,000
7.6
High
2,200,000
290,000
13.2
Medium
5,200,000
1,200,000
23.0
Low
940,000
240,000
25.3
Level of development
More developed regions
7,900,000
730,000
9.2
Less developed regions
6,200,000
1,400,000
23.4
The frequency of infection-related cancer however differs with the SSA regions (Fig. 3.1). In East Africa, Kaposi sarcoma was the most common cancer in men at 17%, while in Southern Africa, it is 5.6% and less than 2% in West Africa. In East African females, Kaposi sarcoma was the third commonest cancer (6.5%) after cervix uteri and breast. Liver cancer was the second most common cancer in West African men at 22%, while its incidence was 3.9% and 3.4% in East and Southern African men respectively (Ferlay et al. 2010, IARC; Fig. 3.1). In females, cancer of the cervix uteri is the most common in East Africa compared to breast cancer in West and Sothern Africa. Viruses are the most common organisms related to cancers, accounting for 10–15% of all cancers worldwide. Bacteria and parasitic organisms also contribute to tumor burden.
3.2 Viruses
The oncogenes of small DNA tumor viruses (polyomaviruses, papillomaviruses, adenoviruses) are viral, and are not cellular in origin compared to cellular-derived oncogenes of transforming retroviruses. While retroviruses induce tumors by activating cellular proto-oncogenes by insertional mutagenesis, DNA viruses need cellular tumor suppressor genes from the host for cancer development (Butel 2000). Human papilloma virus (HPV) oncoproteins (E6, E7) target human p53, DLG, MAGI-1 MUPP1 and pRb proteins, while those of Epstein-Barr virus (LMP1) interact with human TRAFs, and those of Hepatitis B virus (HBx) target human p53 and DDB1 (Butel 2000). Human cancer viruses are all replication competent, and establish long-term persistent infections in various cell types. Cancer is an accidental side-effect of viral replication. Both RNA and DNA viruses that cause cancers have different genomes, life cycles, and the path from viral infection is slow and inefficient and only a minority of infected individuals progress to cancer, usually years or decades after the primary infection (Liao 2006).
Of the various onco-viruses associated with cancer, those of particular interest in SSA include Human Papilloma virus (HPV), Hepatitis B virus (HBV), Hepatitis C virus (HCV), Epstein Barr virus (EBV), Human immunodeficiency virus (HIV), and Kaposi Sarcoma Herpes virus (KSHV) also known as Human Herpes virus 8 (HHV-8; Fig. 3.2).
Fig. 3.2
Incidence of infection related cancers in sub-Saharan Africa in 2012 with causative organisms (Ferlay et al. 2010)
Of infection-related cancers, 100% of cases of carcinoma of the cervix, Kaposi’s sarcoma and adult T-cell leukaemia and lymphoma are attributable to infectious agents (Plummer et al. 2016; Table 3.2). Overall worldwide, 56.5% of all infection-related cancers are attributable to infectious agents. In both less developed and more developed countries, cancers attributable to infectious agents were generally higher in younger age groups, peaking in people aged 40–45 years. However, in women in more developed countries, the peak was in people younger than 40 years (Plummer et al. 2016).
Table 3.2
Number and proportion of new cancer cases in 2012 attributable to infectious agents (Plummer et al. 2016)
Number of new cases | Number of new cases attributable to infectious agents | Attributable fraction | |
|---|---|---|---|
Carcinoma | |||
Non-cardia gastric | 820,000 | 730,000 | 89.0% |
Cardia gastric | 130,000 | 23,000 | 17.8% |
Liver | 780,000 | 570,000 | 73.4% |
Cervix uteri | 530,000 | 530,000 | 100.0% |
Vulva | 34,000 | 8500 | 24.9% |
Anus | 40,000 | 35,000 | 88.0% |
Penis | 26,000 | 13,000 | 51.0% |
Vagina | 15,000 | 12,000 | 78.0% |
Oropharynx | 96,000 | 29,000 | 30.8% |
Oral cavity | 200,000 | 8700 | 4.3% |
Larynx | 160,000 | 7200 | 4.6% |
Nasopharynx | 87,000 | 83,000 | 95.5% |
Bladder | 430,000 | 7000 | 1.6% |
Lymphoma and leukaemia | |||
Hodgkin’s lymphoma | 66,000 | 32,000 | 49.1% |
Gastric non-Hodgkin lymphoma | 18,000 | 13,000 | 74.1% |
Burkitt’s lymphoma | 9100 | 4700 | 52.2% |
HCV-associated non-Hodgkins lymphoma | 360,000 | 13,000 | 3.6% |
Adult T-cell leukaemia and lymphoma | 3000 | 3000 | 100.0% |
Sarcoma | |||
Kaposi’s sarcoma | 44,000 | 44,000 | 100.0% |
All infection-related cancer types | 3,800,000 | 2,200,000 | 56.5% |
3.2.1 Human Immunodeficiency Virus (HIV) and Cancers
Globally, about 35.0 million people were living with HIV as at the end of 2013. Sub-Saharan Africa remains most severely affected, with nearly 1 in every 20 adults living with HIV and accounting for up to 71% of the global burden. (WHO 2015). It has been established that HIV is not able to induce malignant transformation, but it promotes the effects of oncogenic viruses (Fig. 3.1). This is achieved through compromising the body’s immune surveillance against infectious agents as well as against the cells displaying malignant characteristics. Another contribution is by the chronic hyperactivity of the immune system seen in the initial stages of HIV infection. The excessive proliferation of the immune cells is associated with an increased replication of the oncogenic viruses within those cells (Flint et al. 2009).
HIV is associated with an increased incidence of various cancers, notably in the most advanced stages of immunosuppression. KS and NHL are increased >10,000 and 50–600 times, respectively, with HIV, and are designated AIDS defining cancers (ADC). Cervical cancer, increased 5–10 times, is also an ADC. The incidence of a few other cancers are increased with HIV, including Hodgkin lymphoma (10 times), anal cancer (15–30 times), and lung cancer (4 times) though these are designated as non-AIDS defining cancers (Mbulaiteye et al. 2011). 84% of the estimated 44,000 worldwide cases of Kaposi sarcoma occurred in SSA with the majority of cases occurring in patients with HIV-AIDS. About 70% of cases are in East Africa and it is the leading cancer in men and third in women after breast and cervical. 93% of the estimated 27,000 worldwide deaths from KS were in SSA and 84% of these from East Africa (Ferlay et al. 2015).
3.2.2 Human Papilloma Virus (HPV) and Cervical Cancer
Cervical cancer is the fourth most commonly diagnosed cancer and the fourth leading cause of cancer death in females worldwide, accounting for 9% of the total new cancer cases and 8% of the total cancer deaths among females in 2008 (Ferlay et al. 2010). Over 85% of these cases and deaths occur in developing countries with SSA countries recording the highest incidence and mortality rates. Sub-Saharan African countries account for 15 of the top 20 countries worldwide with highest incidence of cervical cancer in 2012 (Fig. 3.3; (Ferlay et al. 2015).
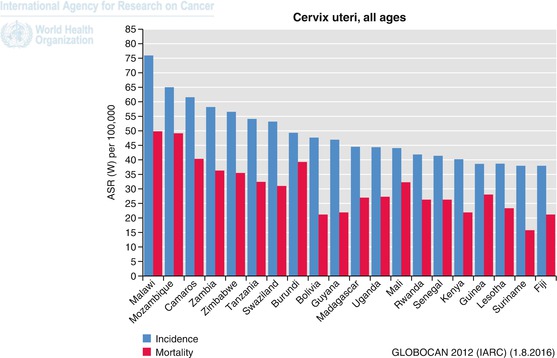
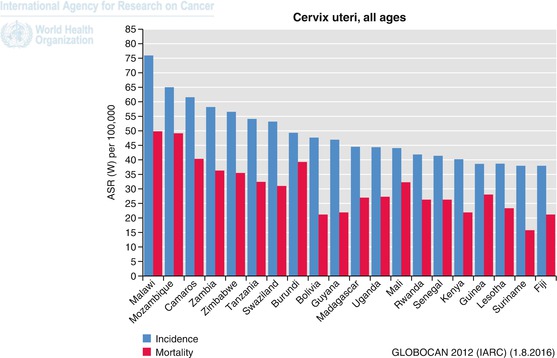
Fig. 3.3
Top 20 countries with highest incidence of cervical cancer worldwide in 2012 (Ferlay et al. 2010)
HPV is a recognized cause for cervical cancer development of epithelial origin, well accommodating the established rules of causality (Walboomers et al. 1999; Munoz et al. 1992). Over 90% of the cervical cancer cases not only harbour viral HPV DNA but also show detection of transcripts encoding the viral E6 and E7 oncoproteins supporting the cell transformation step necessary for carcinogenesis (Smotkin et al. 1989; Halec et al. 2014). Among cervical cancer cases, 70% are attributable to HPV 16 and/or 18. HPV 6 and 11 are considered low-risk types and non-carcinogenic and more commonly responsible for genital warts.
The transmission of human papillomaviruses is mostly sexual but may entail shared objects; perinatal transmission is also possible. HPV 16, mostly, and HPV 18 can also cause squamous cancers of the anus, penis, vulva, and vagina and cancers of the oropharynx (de Martel et al. 2012).
Worldwide women of low socio-economic status have a greater risk of cervical cancer (Palacio-Mejía et al. 2003). A recent study in Mali in West Africa showed that within a population widely infected with HPV, poor social conditions, high parity and poor hygienic condition were the main co-factors for cervical cancer (Bayo et al. 2002). The high prevalence of HPV in sub-Saharan Africa may be attributed to impairment in cellular immunity as a result of chronic cervical inflammation, parasitic infection, micronutrient deficiency and HIV, which are very prevalent in the region (Clifford et al. 2005; Kamal and Khalifa 2006).
3.2.3 Hepatitis B Virus (HBV) and Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is the leading form of primary tumours of the liver (90%). Liver cancer is a major problem in developing regions where 83% of the estimated new liver cancer cases occurred in 2012 (Fig. 3.4). Associated with a poor prognosis, liver cancer is the second most common cause of death from cancer, responsible for approximately 750,000 deaths in 2012 (9.1% of total death due to cancer). Indeed, the overall ratio of mortality to incidence is 0.95. HCC rates are very high in Eastern/South-Eastern Asia and sub-Saharan Africa where the endemic of hepatitis B virus (HBV) is the highest.
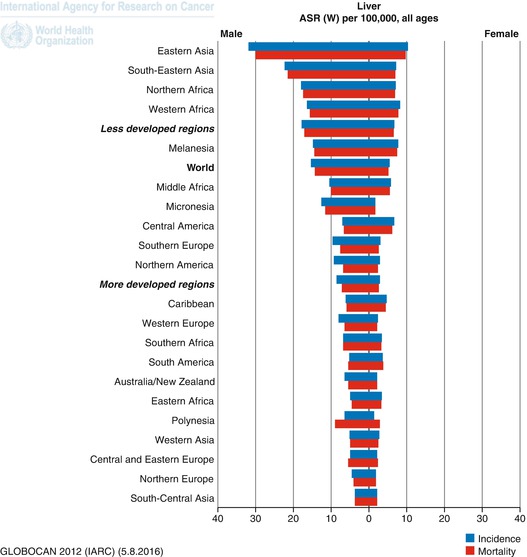
Fig. 3.4
Age standard rates of incidence and mortality of liver cancer worldwide in 2012 (Ferlay et al. 2010)
Hepatitis B viruses are responsible for 340,000 cases of hepatocellular carcinoma globally, which represents nearly 60% of all primary cancers of the liver. 303,000 (89%) of these occur in developing countries (Bray et al. 2012, 2013). In developing countries, the prevalence of hepatitis B chronic infection is still very high in Africa and South East Asia, with up to 10% of the population being chronically infected, which favors the transformation into hepatocellular carcinoma.
The unrelated hepatitis C virus is also involved in the aetiology of hepatocellular carcinoma. Hepatitis C virus causes 25% of hepatocellular carcinomas worldwide, and as high as 40% in Africa (Bray et al. 2012, 2013). Alcohol additionally plays a role in cirrhosis in many cases. Other factors also incriminated in tropical areas include the carcinogen aflatoxin, a metabolite of the fungus Aspergillus, which frequently contaminates grain such as maize, cereals, and spices that represent major staple foods in many parts of the tropics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree