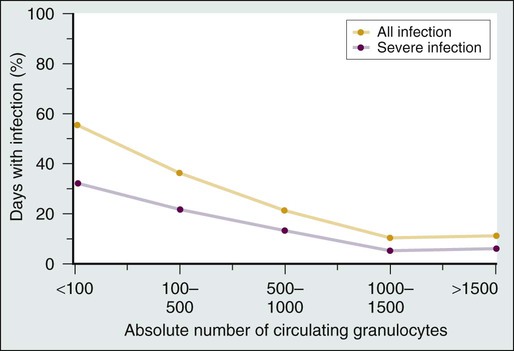
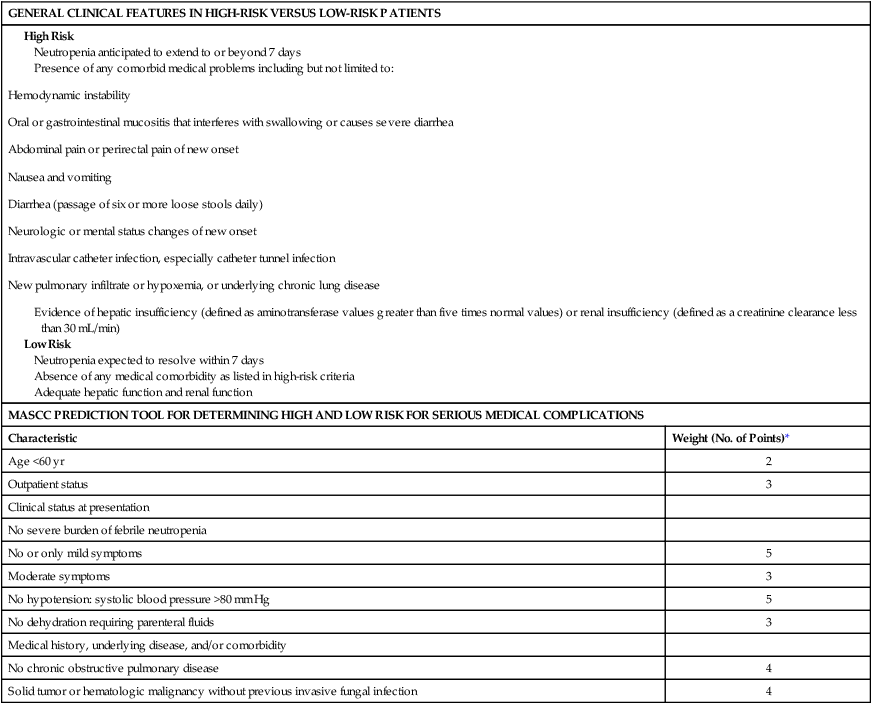
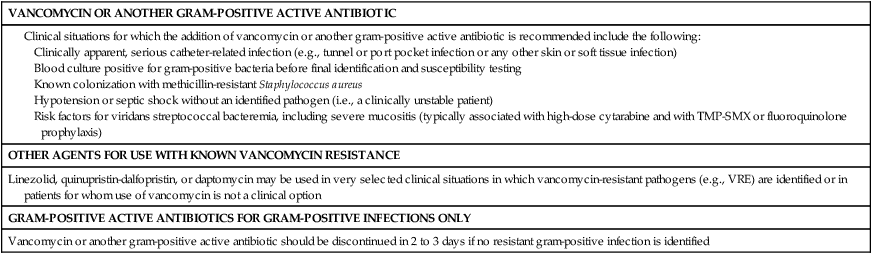
Alison G. Freifeld and Daniel R. Kaul • Risk assessment is an important tool for evaluation and treatment in patients with cancer who have fever and neutropenia. Patients who are expected to have neutropenia lasting more than 7 days, including those undergoing allogeneic stem cell transplantation or therapy for acute leukemia, are considered to be at high risk for infectious complications. Most patients with solid tumors will have neutropenia lasting fewer than 7 days and are considered to be at low risk. • Other risk factors for infection in patients with cancer, beside chemotherapy- and disease-related neutropenia, are the presence of indwelling catheters, comorbid medical conditions such as diabetes or chronic obstructive pulmonary disease, recent surgery, malnutrition, and cellular and humoral immune defects from an underlying tumor and its treatment. • Fever during neutropenia necessitates immediate evaluation, assessment of risk as high or low, appropriate cultures, and prompt institution of empirical broad-spectrum antibacterial therapy with a defined regimen that covers Pseudomonas aeruginosa and enteric gram-negative organisms, as well as common institutional pathogens. Gram-positive active agents are not a standard component of the empirical treatment regimen for fever and neutropenia. • Antibiotic prophylaxis with levofloxacin has been shown to decrease fever and infection in high-risk patients with acute leukemia or those undergoing stem cell transplantation, with neutropenia (<1000 neutrophils/mm3) lasting more than 7 days, although no morality benefit has been consistently shown. • Posaconazole prophylaxis reduces the incidence of invasive fungal infections and mortality in patients undergoing induction for acute leukemia and reduces fungal infections in patients treated for higher grade graft-versus-host disease. Voriconazole has been shown to be equivalent to fluconazole for prevention of fungal infections in allogeneic stem cell transplant recipients. • Newer agents used to treat a variety of lymphoproliferative disorders (e.g., alemtuzumab and purine analogs) result in prolonged suppression of cellular immunity and predispose persons to certain infections; patients receiving these agents may benefit from prophylaxis against opportunistic infections. • An epidemic strain of Clostridium difficile has emerged as a major cause of morbidity and mortality in many centers, and fluoroquinolone use is a risk factor. Metronidazole is recommended for mild disease, but oral vancomycin should be given for more severe symptoms of C. difficile infection. • Numerous antifungal agents may be used for empirical antifungal therapy after 4 to 7 days of broad-spectrum antibiotic use in patients who are still febrile; however, some debate continues regarding whether all patients definitely require empirical antifungal therapy. A high-resolution computed tomography scan of the chest and serial galactomannan assay results may identify possible mold infections and guide antifungal management. • Patients scheduled for allogeneic hematopoietic stem cell transplantation should be screened for evidence of latent herpesvirus and hepatitis virus infections, and prophylaxis should be instituted accordingly. Numerous disease-related and chemotherapy-induced factors render patients with cancer at increased risk for infection.1,2 These factors include the type of cancer (e.g., a solid tumor versus a lymphoma or acute leukemia), the severity and duration of neutropenia, and impairments in cellular function caused by cytotoxic or immunosuppressive drugs; breaches in the integument from surgical procedures, the presence of indwelling plastic venous catheters, or mucositis of the gastrointestinal tract as a result of chemotherapy; and comorbid conditions such as malnutrition, deconditioning, or medical problems such as chronic obstructive lung disease or diabetes. Approaches to prevention, diagnosis, and management of infectious complications in patients with cancer are greatly influenced by the cumulative burden of these risk factors. Neutropenia remains one of the most important predisposing factors for infection, overriding many of the others. This chapter addresses current standards for the management of fever during neutropenia and also highlights contemporary guidelines for the prevention and treatment of common infectious complications in patients with cancer. The association between neutropenia and increased infection risk was first demonstrated by Bodey and colleagues3 in 1966 in a study of leukemic patients undergoing cytotoxic therapy. The data show that the frequency of infectious complications is inversely related to the degree and duration of neutropenia (Fig. 36-1). Infection risk starts to increase when the absolute neutrophil count (ANC) decreases to less than 1000 cells/mm3 and increases dramatically when the ANC count is less than 500 cells/mm.3 Fewer than half of the neutropenic patients who become febrile will have an identified infection. In roughly 10% to 20% or more of patients with neutrophil counts less than 100 cells/mm3, a bloodstream infection will be identified. More than 50% of all episodes of fever and neutropenia represent “fever of undetermined origin,” with no clear infection source on physical and radiographic examination and cultures.3,4 In addition to the severity of the ANC nadir, the duration of neutropenia is also an important determinant of both infection risk and infection type. Brief durations of neutropenia, particularly for less than 7 days, are usually associated with a rapid and favorable response to empirical antibiotic therapy. Fever often may be of unknown origin during this early phase of neutropenia, but if a causative pathogen is identified, bacteria and viruses predominate. A neutrophil count persistently less than 500 cells/mm3 for more than 7 days is associated with greater risk for infection-related morbidity and mortality and is the setting in which Aspergillus and other invasive fungal infections most often occur. Other pathogens that may cause infection during the course of prolonged neutropenia (i.e., after 7 days) include antibiotic-resistant bacteria, Candida species, and other molds. Deaths during the state of neutropenia usually are due to these subsequent infections. Overall mortality rates during the state of fever and neutropenia are less than 1% for low-risk patients and approximately 5% for those with more prolonged duration of neutropenia.5–9 Disruption of integumentary, mucosal, and mucociliary barriers by cytotoxic therapies provides opportunities for invasion by colonizing bacteria on the skin, in the gastrointestinal tract, or in the mucous membranes.10 Shifts in normal colonizing microbial flora at these sites occur as a result of chemotherapy, antibiotic use, and nosocomial exposures, leading to increased colonization with gram-negative and antibiotic-resistant pathogens. Indwelling catheters create a significant breach in host defense, permitting direct access of skin flora and other pathogens to blood or subcutaneous tissue. Tumor growth can disrupt normal anatomic structures, and cancer surgery may result in anatomic alterations and wounds, providing local sites for pathogen entry. Steroid therapy induces a broad immunosuppressive effect, including impaired chemotaxis and killing by neutrophils, impaired T-cell function, and alterations in skin and mucosal barriers. Long-term or high-dose steroid therapy is a significant risk factor for invasive fungal infections in particular (i.e., Aspergillus and Cryptococcus), as well as P. jiroveci (usually seen with tapering of the steroid regimen). Steroid therapy also may predispose affected patients to development of bacterial infections and Mycobacterium tuberculosis reactivation. High-dose cytosine arabinoside therapy causes mucositis that may predispose to life-threatening streptococcal bacteremias.10 Fludarabine and alemtuzumab cause prolonged suppression of CD4+ lymphocytes and attendant susceptibility to infections with Listeria, P. jiroveci, and herpesviruses, as well as bacterial infections.11,12 The administration of temozolomide along with radiation for glioblastoma also is associated with increased susceptibility to P. jiroveci, as well as profound myelotoxicity.13 Patients with myeloma who are treated with the proteasome inhibitor bortezomib are at increased risk for herpes zoster, and prophylaxis should be administered.14 Colonization by pathogenic bacteria, fungi, or viruses generally is a prerequisite for infection. Accordingly, endogenous bacterial and fungal flora and latent herpesvirus infections account for a majority of initial infections in neutropenic patients with cancer.17–17 These infections include skin colonizers such as Staphylococcus aureus and coagulase-negative staphylococci, viridans streptococci, and herpes simplex from the oropharynx and gram-positive bacteria, as well as enteric gram-negative bacteria, from the gut. Candida albicans infections often are derived from the skin or the gastrointestinal or female genital tract. Latent infections that may reactivate during immunosuppression include those due to herpes simplex or varicella-zoster virus, Epstein-Barr virus (EBV), and cytomegalovirus (CMV), as well as hepatitis B and C viruses, M. tuberculosis, and Toxoplasma gondii. Exogenous sources of infection often are found in the hospital and home environments. Contaminated blood products, hospital equipment, water sources, and nosocomial spread of organisms from health care workers represent less common, albeit significant, sources of infection. Common nosocomially spread infections include those due to Clostridium difficile, respiratory viruses, vancomycin-resistant enterococci, and other multiresistant bacteria. Water sources such as faucets and shower heads have been implicated in the spread of Legionella and Aspergillus.18 Outbreaks of Klebsiella and Enterobacter infection related to intravenous solutions have been well documented.21–21 Foods can be a potential source of infection, particularly unwashed fruits and vegetables. Neutropenic patients generally are advised to follow safe food-handling guidelines, which include washing fruits and vegetables thoroughly, cooking eggs until the whites and yolks are completely hard, and cooking meat until it is well done.22 Potted plants, mulch, and excavation and building or renovation sites have been implicated as sources of Aspergillus and other molds that may cause disease.23 Fever often is the only reliable sign of significant underlying infection in the neutropenic patient. No specific clinical features, such as hypotension, chills or the magnitude of the increase in body temperature can accurately distinguish between fever due to an infection and that due to a noninfectious cause. Nor are laboratory tests such as C-reactive protein or procalcitonin levels considered specific or sensitive or enough to be relied on for making decisions about the use of antibiotics at the time of presentation.26–26 Therefore all febrile neutropenic patients should receive empirical broad-spectrum antibiotics, ideally within 1 hour of presentation. Although a clinically or microbiologically documented source of fever is not found in most febrile neutropenic patients, the rapid initiation of empirical antibiotic therapy remains an important standard of care for all patients in this setting. The choice of specific antibiotic regimens depends on an assessment of the patient’s infection risk during neutropenia, which depends on the duration of neutropenia, the underlying cancer, and comorbid medical conditions. Conditions and findings that may alter the empirical antibiotic regimen are shown in Table 36-1. Table 36-1 Approach to Management of Fever and Neutropenia Guidelines for evaluating antimicrobial therapy for fever and neutropenia have been developed by the Infectious Diseases Society of America and the National Comprehensive Cancer Network.2,26 Fever is defined as a single temperature measurement of 38.3°C (101°F) or greater in the absence of other obvious causes; a temperature of 38°C or greater for an hour or longer is considered to represent a “febrile state” that also requires prompt evaluation and intervention in the setting of neutropenia.2,26 Neutropenia is defined as an ANC less than 1000 cells/mm3 in some centers but more often is designated by a neutrophil count of less than 500 cells/mm3, which is a level associated with a much higher risk for infection. For practical purposes, an ANC less than 500 cells/mm3, or a count that is anticipated to fall below that level within 48 hours, constitutes a state of neutropenia. Initial laboratory evaluation should include a complete blood cell count and differential white cell count to determine the degree of neutropenia, liver and renal function tests, oxygen saturation determination, and urinalysis. Chest radiography should be reserved only for patients who have symptoms of respiratory tract infection. Note that radiographic findings may be minimal in neutropenic patients with pneumonia. At least two blood culture samples, each consisting of 20 to 40 mL of blood, should be obtained from both a peripheral vein and from each catheter lumen.2,4 An adequate volume of blood taken for culture will enhance the chances of recovering a pathogen.27 Drawing blood samples from both a vascular catheter and a peripheral vein can help determine whether the catheter is a source of infection. If the differential time to culture positivity between catheter- and venipuncture-derived cultures is greater than 2 hours, the catheter is implicated as a source.28 In patients with cancer, however, one study showed that catheter-drawn blood cultures without concomitant peripheral cultures do have very good negative predictive value and fairly good sensitivity (89%) and specificity (95%).29 A positive culture result for coagulase-negative staphylococci—a common contaminant—requires two positive blood culture sets to be considered a “true positive.”28 Patients who present with fever and neutropenia may have a variety of clinical outcomes. Most receive broad-spectrum empirical antibiotics and survive the episode without major incident. In a minority of patients, significant infections will develop or they will experience other life-threatening medical events. Numerous studies have sought to stratify patients at presentation into those with high versus low risk for complications.2,8,26,30–37 Risk assessment, using a scheme based on clinical criteria, should be performed as part of the initial evaluation to classify patients as high or low risk for serious complications during a febrile episode.2,26 This risk assessment will help determine which empirical antibiotics are appropriate and in what venue—that is, the hospital or outpatient clinic—the patient may be treated for fever and neutropenia. A patient’s risk is driven largely by the duration of neutropenia expected as a consequence of chemotherapy and by certain historical and physical characteristics of the neutropenic patient who presents with fever (Table 36-2). Clinical features of low-risk patients include neutropenia anticipated to last less than 7 days, absence of serious medical comorbidity, and outpatient status at onset of fever. Typically, these patients are receiving chemotherapy for solid tumors. Oral antibiotics given outside of the traditional hospital setting may be appropriate for a subset of low-risk patients. High-risk patients, in contrast, generally have an expected duration of neutropenia of 7 days or longer and/or have serious medical comorbid conditions. They should be always admitted for antibiotic therapy. Recipients of allogeneic hematopoietic stem cell transplants, patients with acute leukemia who are receiving induction or consolidation therapy, and patients with myelodysplasia or aplastic anemia are considered at high risk for complications during neutropenia. Persons who have received autologous hematopoietic stem cell transplants seem to be at intermediate risk for infections, even though they may have prolonged durations of neutropenia (i.e., longer than 7 days). Similarly, patients with lymphoma or CLL and recipients of purine analog therapy (e.g., fludarabine) or those undergoing mini-allogeneic transplantation may be considered to be at intermediate risk for severe infection because they tend to have only brief periods of neutropenia, or none at all, but they may acquire significant impairments of cellular immunity that make them susceptible to certain types of infections. Table 36-2 Risk for Infectious Complications after Cytotoxic Chemotherapy: Clinical Features Defining Risk Status and Risk Prediction in Patients with Fever and Neutropenia MASCC, Multinational Association for Supportive Care in Cancer. *If relevant, points are added to yield a sum score. If the score is >20, the patient is predicted to be at low risk (<10%) for the development of serious medical complications during the course of febrile neutropenia. Adapted from Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 2011;52(4):e56-93. Although many clinicians rely on the criteria shown in Table 36-2, these low- and high-risk features have not been clinically validated.2 The Multinational Association of Supportive Care in Cancer (MASCC) has carefully developed a validated clinical prediction rule that can distinguish high-risk from low-risk patients with substantial accuracy; this rule is shown in Table 36-2.8,35–37 Use of these MASCC prediction criteria should be considered a standard method of distinguishing between low-risk and high-risk patients.2,26 The criteria provide a summation of weighted risk factors, including patient age, history, outpatient or inpatient status, acute clinical signs, the presence of medical comorbid conditions, and severity of fever and neutropenia as assessed by “burden of illness.” Low-risk patients are identified by a cumulative score >21 points (Table 36-2). A fundamental difficulty with the MASCC system is the nebulous nature of one of its major criteria: the “burden of febrile neutropenia” and symptoms associated with that burden. This burden is interpreted to be a measure of how “sick” the patient appears to be on presentation.34 Nonetheless, in a validation study of the MASCC assessment tool, the rate of serious medical complications during the course of neutropenia was only 5% among 441 febrile neutropenic adult patients initially classified as low risk.8 Of the patients with episodes that were predicted to be low risk, 189 (43%) were eligible for oral treatment, but only 79 patients (18%) met additional stringent criteria for discharge from the hospital and receipt of outpatient therapy (clinically stable or improving and with an adequate home environment and psychosocial status) after at least 24 hours of observation in the hospital. Only three patients required readmission to the hospital for fever or other reasons, and no adverse events occurred among the carefully selected outpatient subgroup. Monotherapy with a broad-spectrum antipseudomonal agent such as an extended-spectrum antipseudomonal cephalosporin (e.g., cefepime or ceftazidime), piperacillin-tazobactam, or a carbapenem (e.g., imipenem-cilastatin or meropenem), constitutes a standard approach to the management of fever and neutropenia in both high-risk and low-risk patients with cancer.2,8,26,38–44 The choice of agent should be based on a review of local institutional bacterial susceptibility patterns. Reports of high rates of multidrug-resistant gram-negative bacteremias in patients with cancer underscores the need to select agents based on a review of local institutional bacterial susceptibility patterns.47–47 Some institutions routinely use combination therapy with either (1) an aminoglycoside plus either an extended-spectrum antipseudomonal cephalosporin or piperacillin-tazobactam or (2) ciprofloxacin plus an antipseudomonal penicillin. No clear benefit of combination therapy over monotherapy has been demonstrated, and increased renal toxicity has been observed with aminoglycoside use.2,8,26,38–44 In an era of increasing bacterial resistance, however, circumstances may arise in which initial empirical antibiotic combinations are advisable.48 With the possibility of infection as a result of methicillin-resistant S. aureus, for example, the addition of vancomycin is prudent. If a pneumonia is identified at the outset, then adding an antipseudomonal fluoroquinolone (i.e., ciprofloxacin or levofloxacin) ensures a broadened spectrum against potentially resistant gram-negative or atypical pathogens, as well as “atypical” organisms such as Legionella.49 The initial antibiotic regimen may be modified according to clinical, radiographic, or culture data available at the time of presentation, as outlined in Table 36-1. High-risk patients should receive intravenous antibiotics in the inpatient setting. Again, the choice of specific regimen is highly dependent on institutional profiles of pathogen susceptibility and on potential infection sites in a specific patient. Notably, many of these patients are receiving fluoroquinolone prophylaxis and are therefore at increased risk for resistant gram-negative and gram-positive infections.47 It is not clear, however, whether different antibiotic regimens are required for these patients at the onset of fever. Low-risk patient who can tolerate oral agents may be treated with a combination of oral ciprofloxacin plus amoxicillin-clavulanate. In two randomized double-blind trials, this combination proved as effective as intravenous broad-spectrum monotherapy in selected low-risk patients.33,34 Ciprofloxacin should not be used as a solo agent because of its poor coverage of gram-positive organisms.2,7 Levofloxacin has better activity against gram-positive organisms but less potent antipseudomonal activity than does ciprofloxacin, and it appears to be a reasonable alternative to combination oral empirical therapy in low-risk patients.50 An outpatient treatment course with oral or intravenous (IV) antibiotics may be considered after a brief inpatient stay, during which IV therapy is initiated, fulminant infection is excluded, the patient is deemed to be clinically stable and at low risk for complications, assessment of family support is completed, and the status of initial culture specimens may be ascertained.2,26,31,35 In one large series, oral outpatient treatment for low-risk fever and neutropenia was deemed to be successful in 80% of patients, with 20% of patients requiring readmission to the hospital, primarily for persistent fever. Factors predicting readmission included age greater than 70 years, grade of mucositis greater than 2, poor performance status, and ANC less than 100 cells/mm3 at the outset of fever.51 Vancomycin or other agents with potent activity against drug-resistant gram-positive pathogens are not recommended for routine inclusion in the initial empirical regimen. Although a predominance of gram-positive pathogens is isolated in blood cultures from febrile neutropenic patients, these organisms rarely cause life-threatening infections.52 A large, prospective, randomized trial from the European Organization for Research and Treatment of Cancer failed to show a clinical advantage for using a regimen containing vancomycin compared with one that did not contain vancomycin in adults with fever and neutropenia.53 Widespread use and prolonged courses of vancomycin are linked to the emergence of vancomycin-resistant organisms, especially enterococci. To limit the spread of vancomycin resistance, the Centers for Disease Control and Prevention has issued guidelines to limit vancomycin use.54 These guidelines suggest specific indications for vancomycin therapy in febrile, neutropenic patients with cancer (Table 36-3). Other agents active against gram-positive pathogens include daptomycin, quinupristin-dalfopristin, ceftaroline, and linezolid. Use of these drugs should be similarly limited to distinct indications, rather than broadly applied. Caution is advised when prescribing these agents because each has significant adverse effects; of note, linezolid may cause myelosuppression when used for a prolonged course. Myelotoxicity has been associated with prolonged linezolid use, primarily in the form of thrombocytopenia and occasionally neutropenia.55 However, an analysis of hematologic parameters after stem cell transplantation revealed no delay in the times to neutrophil or platelet engraftment between control patients and those receiving linezolid for a median of 16 days.56 Table 36-3 Appropriate Use of Gram-Positive Active Antibiotics in the Neutropenic Patient with Cancer TMP-SMX, Trimethoprim-sulfamethoxazole; VRE, vancomycin-resistant enterococci. Documented serious infections that are likely to be caused by gram-positive pathogens, such as cellulitis or obvious catheter-related infections, should be treated with vancomycin or another gram-positive active agent. Many catheter-related bloodstream infections are caused by coagulase-negative staphylococcal isolates with high-level beta-lactam antibiotic resistance, and thus vancomycin is indicated. Methicillin-resistant S. aureus (MRSA) has emerged as a major pathogen in hospitalized patients.57 If a neutropenic patient is known to be colonized with MRSA, it is reasonable to add vancomycin to the initial regimen until blood and other cultures are proved negative for this organism. Studies are lacking to confirm whether this strategy is effective. If vancomycin is started empirically for concerns about drug-resistant gram-positive infections but cultures and examination do not identify such an organisms within 2 or 3 days, then empirical vancomycin therapy should be discontinued.2,26,54,58 Substantial mucosal damage increases risk for infection with viridans streptococci, of which 18% to 29% of are beta-lactam resistant.59–62 High-dose cytarabine or intensive therapy that damages oropharyngeal mucosal barriers has been associated with an increased risk of such overwhelming sepsis due to viridans streptococcal infections. Prophylaxis with ciprofloxacin or trimethoprim-sulfamethoxazole (TMP-SMX) also has been associated with an increased risk of gram-positive infections, particularly those due to viridans streptococci.47,59–62 Viridans streptococcal breakthrough infections also have been observed with levofloxacin prophylaxis.61,62 Hypotension or septic shock in a neutropenic patient necessitates very broad empirical antibiotic coverage. Broad coverage is warranted in view of the high mortality rate in neutropenic patients with the systemic inflammatory response syndrome.2,26 Patients should receive multidrug therapy with an antipseudomonal beta-lactam (e.g., cephalosporin, carbapenem, or penicillin, depending on local susceptibilities) plus an aminoglycoside or ciprofloxacin (if the patient is not already receiving fluoroquinolone prophylaxis) and vancomycin or another gram-positive active agent with MRSA activity until culture results are available. No empirical antibiotic regimen initially administered for fever and neutropenia can be expected to cover all possible infections that may occur during the course of neutropenia. Therefore modifications of the initial regimen—that is, additions or changes of antimicrobial agents—sometimes are required. An important consideration in the management of cancer-related infection is that the mean time to defervescence for febrile patients with neutropenia who receive appropriate initial antibiotic therapy ranges from 2 to 7 days.2,5–7 Therefore at least 3 to 4 days of the initial antibiotic regimen should be given to otherwise stable patients, regardless of continued fever, to determine effectiveness. For patients with a documented infection, it is important to note that tissue-based infections such as pneumonia may take longer to respond to antimicrobial therapy.7 Patients who have a fever that persists beyond 4 days of initial antimicrobial therapy and who do not have an identifiable site or source of infection should undergo reassessment of their initial antimicrobial therapy. Any change in antimicrobial agents should be based on the patient’s clinical status, results of examination and cultures, and also the likelihood of early marrow recovery. Although resolution of fever may be slow, persistent fever may suggest a nonbacterial infection, a bacterial infection that is resistant to empirical antibiotics, the emergence of a secondary infection, a closed-space infection, inadequate antimicrobial serum levels, or drug fever. A careful search for these etiologic conditions should be conducted. Frequent and arbitrary antibiotic changes for persistent fever in an otherwise stable patient are to be discouraged. The clinically stable patient with persistent fever may be safely watched without altering the initial antibacterial therapy. If vancomycin was started earlier, it should be discontinued if the patient does not meet the criteria for its use.2,26,54 The addition of vancomycin without specific indications in a blind effort to suppress persistent fever has not been shown to be effective.58 If the fever persists beyond 4 to 7 days, initiation of empirical antifungal therapy should be considered (see the next section on Empiric Antifungal Treatment). Clinically unstable patients who are persistently febrile should be evaluated for changes in antibacterial antibiotics. Double gram-negative bacillary coverage, as reviewed earlier, is recommended. The addition of vancomycin should also be considered, particularly if the clinical indications outlined in Table 36-3 are present. Empiric antifungal therapy traditionally is started when neutropenic patients demonstrate continued or recrudescent fever after 4 days or more of an empiric antibacterial regimen because the risk of invasive fungal disease, particularly invasive aspergillosis, increases with prolonged duration of neutropenia.63,64 The empiric use of amphotericin B in early studies during the 1970s and 1980s showed a reduction in breakthrough fungal infections.38,65,66 Since then, numerous comparative studies have demonstrated that less toxic alternatives, including liposomal amphotericin B, itraconazole, and caspofungin, are not inferior to amphotericin B desoxycholate.67–72 Voriconazole is also effective in reducing breakthrough fungal infections.73 The other available echinocandins—anidulafungin and micafungin—are less well studied but presumably are effective in this setting. Itraconazole has been demonstrated to have efficacy in this setting as well, but concerns about liver and cardiac toxicities have discouraged use of this drug.67,72 Whether all patients with persistent fever require empiric antifungal therapy, and when it should be started, are subjects of long-standing debate. Invasive fungal infections are now relatively infrequent during neutropenia with the advent of more effective antifungal prophylaxis and the use of colony-stimulating factors to abbreviate duration of neutropenia. Furthermore, fever is obviously a nonspecific surrogate marker for fungal infection. Currently, guidelines suggest that an antifungal agent be started at day 4 to 7 in high-risk patients who are not receiving antifungal prophylaxis.2,26 Candidemia is the greatest concern in these patients, and fluconazole, amphotericin B preparation, caspofungin, itraconazole, or voriconazole are considered acceptable choices. If the patient is already receiving fluconazole prophylaxis (which is commonly the case), certain non-albicans species of Candida, including C. glabrata and C. krusei, along with mold infections such as invasive aspergillosis, must be considered. Fluconazole has reduced activity against these Candida species and lacks activity against molds. At present, no data are available to guide the use of empirical antifungal therapy in patients already receiving antimold prophylaxis, such as with voriconazole, posaconazole, or an echinocandin. In all cases, symptoms and signs of invasive fungal pneumonia or sinusitis should be sought; the workup may include computed tomography (CT) scans of chest or sinuses (or both), with follow-up nasal endoscopy or bronchoalveolar lavage as indicated. Biopsy and culture of any suspected lesions should be pursued aggressively to make a definitive mycologic diagnosis that can guide therapy. A CT scan of the chest is increasingly being used to evaluate the possibility of invasive aspergillosis in patients with prolonged fever and neutropenia; in one study, 90% of persons with proven active disease showed radiographic abnormalities by CT.74 Macronodules with or without a halo sign are characteristic of invasive aspergillosis, with the halo sign being an especially important early clue.75,76 Other manifestations include nodular, wedge-shaped, peripheral, multiple, and cavitary lesions. An air-crescent sign generally is a late finding. Initiation of antifungal agents on the basis of finding a halo sign has been associated with significantly better response to therapy and improved survival.76,77 Maertens and colleagues78 used intensive monitoring for clinical symptoms and signs, serial galactomannan testing (discussed later in this section), and early CT scanning to identify a group of patients with persistent fever while receiving fluconazole prophylaxis in whom antimold therapy did not appear to be required. These data, as well as increasing clinical experience, have led some experts to suggest withholding empiric antifungal therapy if the patient is clinically stable and has no clinical or chest CT scan signs of fungal infection, if no Candida or Aspergillus organisms are recovered from any site, and if neutrophil recovery is imminent. A high-resolution chest CT scan may be a useful screening tool in patients with persistent fever and neutropenia; any abnormalities should be investigated with nasal endoscopy or bronchoalveolar lavage; biopsy and culture of any suspected lesions should be pursued aggressively to make a definitive diagnosis; and treatment with an antimold agent should be initiated. The serum galactomannan assay specifically detects Aspergillus organisms but not other common fungal pathogens.79 Sensitivity varies widely in different patient populations. A recent metaanalysis reported sensitivities of 64% to 78% and specificities of 81% to 95% in patients with neutropenia or neutrophil dysfunction.80 Many conditions affect the performance of the galactomannan assay, especially the use of concomitant piperacillin-tazobactam (false-positive) or antimold antifungal agents (false-negative). Although prospective serial galactomannan monitoring may be useful for patients at high risk for Aspergillus infections, routine use in low-risk patients is not advised.79,80 Furthermore, a single negative test result is of little value in ruling out invasive aspergillosis, although a positive result in concert with abnormalities on the chest CT scan makes the diagnosis highly probable. Galactomannan testing of bronchoalveolar lavage fluid appears to be specific and more sensitive than culture for identifying invasive aspergillosis.79,81,82 It generally is recommended that empiric antibiotic therapy continue until recovery of the ANC to more than 500 neutrophilic cells/mm3 on one occasion, as long as the patient is clinically stable. In a stable patient who remains febrile despite the return of higher counts, it usually is safe to discontinue antimicrobial drugs and look for a source of fever. In patients who are afebrile and clinically stable but have continued neutropenia, some clinicians recommend a 2-week course of antibiotics at a minimum and then stopping the antibiotics, with close observation.2,26 Documented infections should be treated for a minimum duration of 7 to 14 days with an antibiotic regimen that is narrowed and directed toward any organisms that have been documented microbiologically. Activity against Pseudomonas aeruginosa should be maintained in most patients who remain neutropenic. Most experts prefer to continue antibiotics at least until the ANC returns to more than 500 cells/mm3. A longer course is given if clinically necessary (for example, if a documented infection is ongoing) regardless of neutrophil recovery. Persistent fever of unknown source is not a reason to continue empiric antibiotics beyond ANC recovery.2,26 For low-risk patients who typically have brief periods of neutropenia, some groups of investigators have examined the practice of stopping antibiotics before the ANC reaches 500 cells/mm3. With a clear and steady increase in the ANC or, alternatively, in the absolute phagocyte count (antigen presenting cells = polymorphonuclear neutrophils + bands + monocytes), it appears that the discontinuation of antibiotics before a count of 500 neutrophilic cells/mm3 is achieved can be safe as long as no complicating comorbid conditions are present.51,83–87 Prophylactic use of hemopoietic growth factors is common in the setting of intensive chemotherapy regimens such as stem cell transplantation. Treatment of fever or infection with growth factors, however, is not standard practice. No consistent benefit has been demonstrated in terms of morbidity (i.e., duration of fever and use of antimicrobial agents) or mortality among several randomized controlled trials of the addition of growth factors to an antibiotic regimen at the time of fever during neutropenia.90–90 The routine use of growth factors in treating febrile neutropenic patients is discouraged. Therapy with colony-stimulating factors, however, could be considered for severely neutropenic patients who have serious uncontrolled infections such as bacterial sepsis, pneumonia, severe cellulitis or sinusitis, systemic fungal infections, hypotensive episodes, or multiorgan dysfunction as a result of sepsis. Prophylactic use of the myeloid growth factors is recommended in patients at greater than a 20% risk of febrile neutropenia and in patients with important factors that increase the individual risk of neutropenic complications.90 Granulocyte transfusion may potentially increase the response to antimicrobial therapy in selected cases of uncontrolled fungal or gram-negative infection during prolonged neutropenia. Granulocyte colony-stimulating factor use in donors has increased the granulocyte yield approximately fourfold. Multiple recent studies have shown that granulocyte transfusions can be helpful in controlling the progression of severe infections despite the use of appropriate antibiotics, with a response rate of 40% to 80%.91 Variability in results is a consequence of patient characteristics. This benefit is limited to a select patient population, because the incidence of prolonged yet reversible neutropenia is relatively low. Rare adverse events associated with granulocyte transfusions include transmission of human CMV, alloimmunization associated with fever, graft-versus-host reactions if granulocytes are not irradiated, and progressive platelet refractoriness. Bloodstream infections occur in about 10% to 20% of febrile patients during neutropenia, most often when neutrophil counts are less than 100 cells/mm3.2,26,45–47,92 The risk of bacteremia is related to the depth of neutropenia, the presence of gastrointestinal mucositis or of an indwelling catheter, or the concomitant presence of a specific site of infection such as pneumonia or soft tissue process. Most bacteremias are due to gram-positive organisms, with coagulase-negative staphylococci and streptococci predominating. Gram-negative pathogens, including Escherichia coli, Enterobacter, Klebsiella, and P. aeruginosa, are important albeit less frequently occurring pathogens.16 A classification system for bacteremias in febrile neutropenic patients has been developed by Elting and colleagues,7 based on the size and presence of associated tissue involvement. Complex bacteremias were those associated with deep-tissue infections of the lung, the liver or spleen, the kidney, the colon, bone and joints, veins and the heart, meninges, and soft tissues with necrosis, or affected skin or soft tissue, wounds, or cellulitis greater than 5 cm in diameter. Simple bacteremias were associated with less tissue involvement (e.g., bacteruria, otitis, pharyngitis, and an affected area of soft tissue less than 5 cm in diameter). The prognostic significance of a complex infection associated with bacteremia on survival was dramatic. At 21 days, 20% of patients with complex infections were dead, compared with only 5% of patients with simple bacteremias (P < .0001). Profoundly neutropenic patients with simple bacteremias had a much higher response rate to antibiotics than was noted in patients with complex bacteremias (94% vs. 70%; P < .0001). The median time to defervescence for patients with simple bacteremias was half that observed for patients with complex bacteremias (2.5 days vs. 5.3 days; P < .0001). With increasing incidence of MRSA in hospitals and the community, it is recommended that vancomycin be added to standard empirical antibiotic coverage if gram-positive cocci in clusters are isolated from a blood culture, pending identification.16,48,52–54,57 Vancomycin-resistant enterococcus (VRE) also is common in high-risk cancer patients at some institutions. If gram-positive cocci in pairs and chains are identified in blood cultures in settings where VRE is prevalent, then empiric addition of an antimicrobial active against VRE (e.g., linezolid or daptomycin) is prudent, pending definite identification and susceptibility profile. Gram-negative bacteremias in the neutropenic patient are increasingly prevalent in some institutions and are associated with high mortality unless treated promptly and with appropriate antibiotics.95–95 A variety of resistance mechanisms are evolving among gram-negative organisms. Therefore if gram-negative rods are isolated in blood cultures during fever and neutropenia, an aminoglycoside (which is preferred if the patient was heavily pretreated with fluoroquinolones) or a fluoroquinolone should be added to empiric therapy regimens to ensure coverage of resistant strains until a full susceptibility report is available. Pulmonary infections are associated with the greatest morbidity and mortality, even when a specific pathogen is not identified. Approximately 25% of all febrile episodes in the neutropenic patient, and 50% of documented infections, are pneumonias.98–98 Numerous infectious and noninfectious causes of pulmonary infiltrates are found in patients with cancer who have fever and neutropenia. Noninfectious causes include the underlying disease itself, radiation therapy, drug toxicity, pulmonary hemorrhage, and leukostasis. Infectious involvement of the lungs may be caused by bacteria (pneumococci, members of Enterobacteriaceae, Pseudomonas spp., and Legionella spp.), fungi (Candida, Aspergillus, and Fusarium spp.), viruses (influenza virus, parainfluenza virus, respiratory syncytial virus [RSV], CMV, and HSV), and protozoa (Toxoplasma, Cryptococcus, and Strongyloides). Auscultatory abnormalities in the chest may be minimal or absent, and the chest radiograph appears normal at the onset of clinical manifestations in 30% of neutropenic patients with subsequently identified pneumonia.97 A CT scan of the chest is essential to better define a pulmonary process. Neutropenia will decrease the diagnostic advantage normally provided by the sputum examination, because purulent sputum production is rare in this setting. Bronchoalveolar lavage may increase the diagnostic yield, especially for P. jiroveci and viruses, but less so for bacteria once antibiotics are started.99 The yield for molds such as Aspergillus with this procedure has been mostly in the range of 50% for suspected cases, and thus a negative result on bronchoalveolar lavage sampling does not rule out an invasive fungal process. PCR assay or galactomannan testing of lavage fluid may increase these yields.7,79,81,82,92 If the clinical picture, radiographic appearance, and findings on lavage fluid analysis are nondiagnostic, a thoracoscopic or CT-guided lung biopsy should be considered if the patient’s platelet count is adequate. The radiographic appearance of a pulmonary infiltrate may give clues to the etiology (Table 36-4).74–77,98 Focal lesions are suggestive of bacterial etiology and should be treated accordingly with broad-spectrum antibiotics. Nodular lesions, particularly those with surrounding areas with a ground-glass appearance (i.e., halo lesions), are suggestive of mold infection, such as with Aspergillus. This presentation is of particular concern in the two patient groups that are at particularly high risk for mold infection: patients with graft-versus-host disease (GVHD) taking high-dose steroids and patients with prolonged neutropenia, such as those undergoing induction treatment for acute myelogenous leukemia. In these types of patients, even minimal symptoms of low-grade fever, pleuritic chest pain, or nasal stuffiness should prompt an immediate CT scan of the chest and sinuses to look for signs of invasive aspergillosis. Table 36-4 Pulmonary Infiltrates and Their Association with Specific Infectious and Noninfectious Disorders
Infection in the Patient with Cancer
Introduction
Infection Risk Factors
Neutropenia as a Risk Factor for Infection
Other Risk Factors for Infection
Sources of Infection
Approach to Fever in the Neutropenic Patient
History and Physical Findings
Indicated Modifications in Antimicrobial Coverage or Diagnostic Test
Fever during neutropenia
Empiric antibiotic regimen (see text); if the patient is receiving antibiotic prophylaxis, then empiric therapy must be based on an agent of a different class from that used for prophylaxis (e.g., if the patient is receiving fluoroquinolone-based prophylaxis, then switch to a beta-lactam–based regimen)
Hypotension, signs of sepsis
Broad-spectrum antimicrobial coverage: a triple-antibiotic regimen (e.g., carbapenem plus vancomycin plus an aminoglycoside) is recommended; if cultures are negative for gram-positive organisms, consider discontinuing vancomycin after 3 days
Fever that is persistent or recrudescent on or after day 5 of antibiotic therapy
Empirical antifungal therapy: add an amphotericin B product, an echinocandin, or voriconazole if the patient is not already receiving prophylaxis with a mold-active agent; a CT scan of the chest may help identify fungal infection; consider a CT scan of the chest and frequent galactomannan testing during neutropenia to guide preemptive treatment as an alternative strategy to empiric antifungal treatment
Severe oral or esophageal mucositis
Send a swab for viral (HSV) culture; add antiviral coverage (if not already being given); consider antiviral resistance to prophylaxis if esophagitis occurs late in the course of neutropenia; add an antifungal agent for possible Candida esophagitis; switch streptococcal coverage to vancomycin; esophagoscopy may be indicated
Catheter exit site or tunnel erythema, tenderness, or discharge or cellulitis at any site
Culture any discharge; add vancomycin; for tunnel infection (erythema and tenderness 2 cm above exit site), catheter removal and surgical débridement generally are required
Possible anaerobic infection
Add metronidazole if broad-spectrum antibiotics without activity against anaerobes are being used
Abdominal pain, especially right lower quadrant, suggestive of neutropenic enterocolitis; oropharyngeal or neck or soft-tissue swelling
Perform a CT scan of the affected area; supportive care: avoid surgical intervention if possible in a neutropenic patient
New pulmonary infiltrate
Bronchoscopy (with or without biopsy) is the preferred method for evaluating new infiltrates in high-risk patients;
Nodular: add mold coverage with voriconazole, posaconazole, or amphotericin B preparation;
Alveolar: broaden gram-negative coverage and add Legionella coverage (quinolone or macrolide);
Interstitial: send specimen for diagnostic studies for both respiratory viruses, PCP, and herpesviruses, particularly CMV;
Review patient history for risk factors for tuberculosis or infection with endemic fungi
Upper respiratory symptoms of coryza, congestion during fall/winter
Send nasal wash or swab for respiratory viral studies (e.g., culture, PCR, rapid antigen testing)
Hemorrhagic cystitis
Indicated studies include urine viral culture and BK virus PCR assay (for hematopoietic stem cell transplant recipients)
Definitions
Initial Evaluation
Risk Assessment
Empiric Antibiotic Therapy
Use of Vancomycin or Other Gram-Positive Agents
Initial Empirical Therapy for Patients Who Are Clinically Unstable
Subsequent Modifications of Empiric Antibiotic Regimens
Empiric Antifungal Therapy
Duration of Antibiotic Therapy
Adjunctive Therapies
Hematopoietic Growth Factors
Granulocyte Transfusions
Infections in the Patient with Cancer
Bacteremia
Pulmonary Infections
Radiologic Sign
Potential Etiologic Disorder(s)
Interstitial infiltrates
Pulmonary edema
Diffuse alveolar damage
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access