Fig. 44.1
Ultrasound of the left thyroid lobe showing a hypoechoic nodule 25 × 16 mm in size
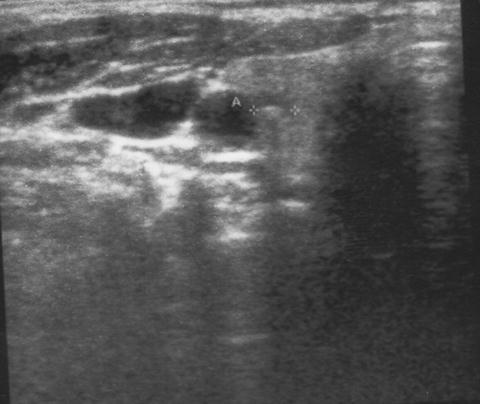
Fig. 44.2
Ultrasound of the right thyroid lobe showing a small calcified nodule 4.8 mm in size
Assessment and Literature Review
Is It Medullary Thyroid Cancer?
Medullary thyroid cancer affects 0.3–1.4 % of patients with thyroid nodules [1–4]. They synthesize and secrete calcitonin proportional to overall tumor mass into the bloodstream. In the setting of nodular thyroid disease, an elevated basal calcitonin ≤ 100 pg/mL can pose a diagnostic dilemma that becomes more problematic as the serum calcitonin levels move lower and lower. Because male thyroid glands contain larger numbers of parafollicular C cells than female thyroids, males have higher serum calcitonin levels. Thus, there are gender-specific basal calcitonin thresholds for thyroidectomy: 20 pg/mL for women (positive predictive value, PPV 88 %) and 80–100 pg/mL for men (PPV 100 %) [5]. Corresponding absolute calcitonin thresholds after stimulation with pentagastrin are 250 pg/mL for women and 500 pg/mL for men (PPV 100 % each) [5]. Interestingly, our patient’s calcitonin serum levels, ranging from 15.2 pg/mL to 25 pg/mL basally depending on the assay and reaching 256 pg/mL after stimulation with pentagastrin, crossed the absolute calcitonin thresholds for women of 20 pg/mL basally and 250 pg/mL after stimulation with pentagastrin by a narrow margin. Although it may be a more suitable provocative agent than calcium, pentagastrin has been unavailable since 2005 in many countries, including the USA. In the era of more sensitive immunochemiluminometric calcitonin assays, the need for provocative testing is dwindling. It is important to note that our patient required thyroid surgery for the cytological diagnosis of follicular neoplasia from the indeterminate left nodule, which is what prompted calcitonin screening in the first place.
If It Is Medullary Thyroid Cancer, Will It Be Confined to the Thyroid Gland?
The diagnosis of sporadic medullary thyroid cancer raises the question of whether the tumor is limited to the thyroid gland or has already spread beyond the thyroid capsule. On preoperative neck ultrasonography, more than one-third of patients with MTC have false-negative findings [6]. This is why basal calcitonin serum levels provide important clues as to the presence of occult lymph node metastases [7].
The overall risk of lymph node metastases is estimated at:
0 %—when basal calcitonin is ≤20 pg/mL
11 %—when basal calcitonin is 20.1–50 pg/mL
17 %—when basal calcitonin is 50.1–100 pg/mL
35 %—when basal calcitonin is 100.1–200 pg/mL
Lymph node metastases begin to appear in the:
Ipsilateral central and lateral neck—when basal calcitonin exceeds 20 pg/mL
Contralateral central neck—when basal calcitonin exceeds 50 pg/mL
Contralateral lateral neck—when basal calcitonin exceeds 200 pg/mL
Absent clinical and ultrasonographic evidence of suspicious lymph nodes, the patient’s most recent basal calcitonin of 16.5 pg/mL argued against the presence of lymph node metastases.
If Basal Calcitonin Fails to Normalize, Will Reoperation Be Worthwhile for Minimal Disease?
The prospect of biochemical cure after a second neck operation is contingent on the residual basal calcitonin level, as long as no more than five lymph node metastases were removed at the initial operation [8]:
75–77 % for a residual basal calcitonin <10 pg/mL
35–36 % for a residual basal calcitonin of 10.1–100 pg/mL
The pros and cons of reoperation in a scarred neck (high chance of definitive cure versus expectant observation of minimal residual disease) need to be detailed to the patient. Reoperations in a scarred neck, as a matter of principle, should not be embarked on outside specialist centers to keep surgical morbidity to a minimum. The one-time cost of reaching a definitive cure and the cost of daily levothyroxine supplementation may be smaller from a societal perspective than the need for continual biochemical follow-up and imaging studies, some of which may prompt additional operations at incremental costs [5].
Management of the Case
After informed consent, the patient opted for thyroidectomy under intraoperative nerve monitoring as a minimum procedure, with possible lymph node dissection depending on intraoperative evidence of nodal disease. Inside the dorsal portion of the right lobe, a small firm nodule was identified. The central neck was explored for suspicious nodes but none were found, as to be expected with a basal calcitonin level ≤20 pg/mL, so that no neck dissection was performed.
Histopathological examination revealed a 15 mm follicular adenoma in the left lobe and a 5 mm medullary thyroid cancer surrounded by normal thyroid parenchyma in the absence of C-cell hyperplasia.
The patient made an uneventful recovery. Video laryngoscopy confirmed normal vocal cord function after the operation. On the second postoperative day, basal and calcium gluconate-stimulated calcitonin levels were below the assay’s detection limit (<2 pg/mL; IMMULITE 2000, Diagnostic Products Corporation, USA) reflecting biochemical cure. Follow-up examinations 4 weeks later showed normal parathyroid hormone serum levels, whereas serum calcitonin remained below the assay’s detection limit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





