Fig. 1
Da Vinci Si® system
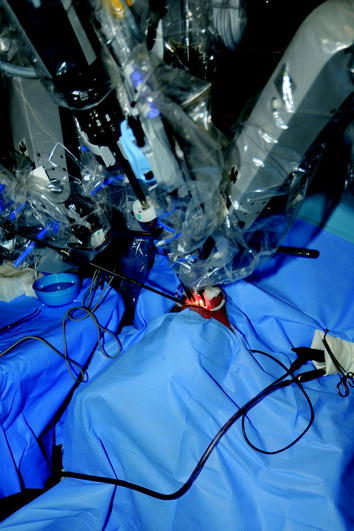
Fig. 2
3D HD endoscope camera
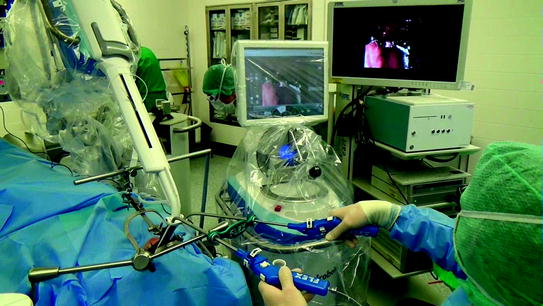
Fig. 3
Three-dimensional movement capacity
With the Flex® Robotic System—developed specifically for transoral head and neck resections—the surgeon is able to insert a flexible endoscope into the pharynx. The endoscope can be advanced and steered in a sequential manner, alternating between a flexible and rigid state. Thus, the surgeon can define a path of approach that is not limited by line-of-sight access. Ultimately, the surgeon creates a self-supporting, stable platform from which he or she may visualize and operate (Fig. 4). An HD camera can transmit the pictures on a touch screen and on an external monitor. The surgeon controls the motion of the endoscope with a joystick on the Flex® Console which allows the surgeon to reposition or stabilize the endoscope anytime during the surgery (Fig. 5). There are two different, non-crossing, flexible working channels aside the endoscope for direct manipulation of flexible, fully articulating and rotating operating instruments. These instruments include a Flex® Laser Holder, Flex® Monopolar Maryland Dissector and Flex® Fenestrated Grasper for retraction and tissue manipulation, a Flex® Needle Driver for suturing, and a Flex® Monopolar Needle Knife, Flex® Monopolar Spatula, and Flex® Monopolar Scissor to cut tissue. When operating this system, the instruments provide the surgeon with direct tactile feedback.
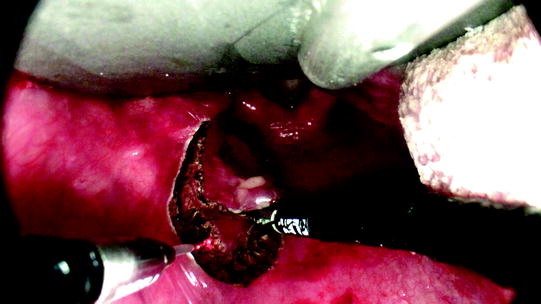

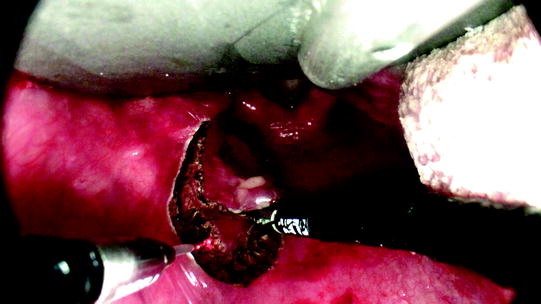
Fig. 4
Self-supporting, stable platform

Fig. 5
Flex® Console
5 The Use of TORS in Head and Neck Surgery
The goal of the surgical treatment of HNSCC is complete resection of the cancer with simultaneous preservation of the complex organ functions. Over the past few decades, transoral laser microsurgery (TLM) has been established as an important surgical concept and has become the gold standard for many HNSCC surgeons (Steiner 1994). This was due to comparable oncological outcomes after TLM treatment with reduced comorbidities and loss of function in comparison with classic open surgery techniques. After the introduction of robotic surgery, the systems were investigated with regard to surgical and patient benefits, including length of hospital stay, operating time, quality of surgical resection and quality of life for the patient compared to conventional surgery.
Over the past several years, the development of robotic systems has improved, and therefore, its use in the surgical treatment of HNSCC has become a relevant treatment modality for many patients.
After 2005, indications for TORS started to include the base of tongue (O’Malley et al. 2006), larger tumors of the pharynx (Weinstein et al. 2007) and the parapharyngeal space (O’Malley et al. 2010), tumors of the supraglottic area (Solares and Strome 2007) and the glottis (Desai et al. 2008). Choby and colleagues were able to demonstrate similar quality of life data in patients with OPSCC after TORS in comparison with other transoral surgical approaches and improved results in comparison with open surgery (Choby et al. 2015). Other data indicate an improved swallowing functionality for stage III and IV OPSCC after TORS in comparison with chemoradiotherapy (More et al. 2013). Additionally, different groups suggest the introduction of the TORS-assisted removal of base of tongue tonsil tissue for screening purposes in patients with cancer of unknown primary (CUP) syndrome (Mehta et al. 2013). Since CUP originating from oropharyngeal carcinomas is strongly correlated with HPV positivity, this becomes a particularly interesting aspect in regard to HPV-positive patients (Zengel et al. 2012). For resections of malignant lesions from the supraglottic and epiglottic regions using TORS, a local recurrence rate below 20 % has been reported (Mendelsohn and Remacle 2015).
Despite the enlarged spectrum of indications for TORS in HNSCC, there are limitations: One important factor is the accessibility of the region of interest. Although there have been reports about several glottic procedures (Smith 2014), the exposition of the narrow as well as delicate endolaryngeal structures is limited. Especially in comparison with conventional small endoscopes, the rigid, straight robotic arms, the bulky instruments and the short and broad retractors impair the accessibility (Mattheis et al. 2012). Additionally, in comparison with the crystal clear microscope-based visualization offered by TLM, the current cameras provide lower resolution and lower magnification resulting in reduced visualization of endoluminal structures. With the introduction of the Flex® Robotic System, some of these restrictions have been addressed. The combination with flexible instruments allows for a better accessibility of the relevant structures. Regions of the hypopharynx, especially the pyriform sinus, and regions of the larynx, e.g., the supraglottic region, can be simultaneously visualized, which helps in the assessment of possible infiltration of anatomical structures. The visual resolution remains inferior to the microscope of TLM. Surgeons positively report about the gained tactile feedback. Nevertheless, the system needs prospective clinical trials in order to validate its value and certify improvement in comparison with other established modalities, i.e., TLM.
With the technical advancements over the past few years, many of the early restrictions could be set aside leading to contraindications comparable to those for TLM procedures. Weinstein et al. grouped the contraindications into vascular, functional, oncologic and non-oncologic reasons (Weinstein et al. 2015): Vascular contraindications of TORS for oropharyngeal cancer include close vicinity to important arterial structures such as the carotid artery (e.g., by tumor encasement, or retropharyngeal course of the carotid artery in case of tonsillar cancer) or both lingual arteries (midline tongue base cancer). Functional contraindications include a required resection of more than 50 % of functional relevant structures such as deep tongue base musculature. Oncologic contraindications can result because of size and/or infiltration (T4b, prevertebral fascia), unresectable neck disease or distant metastases and neoplastic-related trismus. Finally, any non-oncologic conditions that prevent either any surgical approach in general or the specific transoral approach such as trismus or cervical spine disease limit the procedure. In our department, we are performing two-thirds base of tongue resections—irrespective of TORS—in selected cases.
Another important factor that potentially limits the use of TORS is the availability of these cost-intensive devices at the surgical centers. One of the main initial critiques of TORS was the high cost. This important factor in modern health care remains an issue. Dombrée and colleagues demonstrated that even in the case of well-trained surgical teams with short surgical times, the costs of the da Vinci system remain higher as compared to conventional surgical strategies in larynx procedures (Dombree et al. 2014). Other sources, however, report shorter periods of hospitalization and treatment-related costs, as well as patient morbidity, partially depending on the tumor location (Richmon et al. 2014; Chung et al. 2015). However, these results are from retrospective studies and their validity may be threatened by biases in areas such as patient selection. In general, additive to the costs of open surgery or TLM, which are mainly determined by personnel, surgical time and hospitalization, the costs of TORS-assisted procedures are also determined by high acquisition costs and the maintenance. This aspect potentially limits the distribution in institutions that are involved in the primary care of HNSCC patients.
6 TORS in HPV-Positive Patients
TORS has demonstrated advantages for a better visualization of the pharynx, especially at the base of tongue. In HPV-related carcinoma, the base of tongue as part of the oropharynx is frequently involved. Surgeons (and therefore patients) potentially benefit from an increased mobility and a better overview in comparison with conventional TLM. In comparison with chemoradiotherapy, TORS has been associated with lower morbidity rates and better functional outcomes. Still, the decision for or against the surgical treatment lies at the end of an interdisciplinary team-based approach including the patient’s individual wishes and needs. Therefore, after the decision for surgical treatment has been made, it must then be determined if TORS is indicated. So far, HPV testing is not yet a prognostic predictive marker for a certain established therapeutic alternative and therefore should not change management decisions except in the context of a trial, yet a majority of US physicians report an influence of HPV testing on their treatment approach for OPSCC (Maniakas et al. 2014). As reasons were not given in this survey, one can only speculate that HPV testing may lead to a de-intensification of therapy in the case of HPV-positive test results. To what extent that the TORS procedures will play a role in de-intensification for HPV-positive patients needs to be further evaluated, as the technical development will continue and trials for de-intensification strategies are ongoing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree