The National Cancer Data Base (NCDB) provides feedback on adherence to National Quality Forum (NQF)–endorsed measures to promote best outcomes in colorectal cancer. We examined the care delivered to patients with colorectal cancer at our institution and developed a protocol to enhance nodal retrieval and to ensure that patients with fewer than 12 nodes are considered for adjuvant chemotherapy. Few patients met the NQF criteria for adjuvant radiation. A protocol was developed to address this issue, and this provides a model for use in a multidisciplinary effort to improve adherence to measures associated with best outcomes in colorectal cancer.
Winthrop-University Hospital is a 591 bed community based teaching hospital affiliated with the State University of New York at Stony Brook (SUNY-SB). The hospital provides clinical clerkships and fourth year electives for students from SUNY-SB and will soon become a clinical campus of the medical school with full responsibility for the final 2 years of education for a cohort of these students. The hospital offers independent residencies in internal medicine, obstetrics-gynecology, pathology, pediatrics, and radiology, and has integrated residencies with SUNY-SB in general surgery and orthopedics. Fellowships are available in many medical and pediatric subspecialties, as well as in colorectal surgery and vascular surgery.
Most faculty members, particularly in surgery, are community physicians. In General Surgery, there are 40 practicing surgeons, of whom 9 are full time. Eight of the general surgeons have also been fellowship trained in colorectal surgery and all of these are community surgeons. Most of the colorectal surgeons work for 1 of 2 groups, but there are solo practitioners as well, which leads to a diversity of practice settings and styles for those surgeons engaged in the resection of colorectal cancers.
Winthrop has had a cancer program accredited by the Commission on Cancer (COC) since 1966. The COC began to provide information to its accredited programs in 2005 on the degree to which these programs were adhering to standards of care associated with best outcomes. Initially this program, called the Cancer Program Practice Profiles Reports (CP3R), focused on the use of adjuvant chemotherapy after resection of node positive (stage III) colon cancer. Data from the National Cancer Data Base (NCDB) on the use of chemotherapy after resection of node positive colon cancer was reported back to each accredited center with a ranking of its performance as concordant if the center was in the top 25% of centers in the use of chemotherapy, or nonconcordant if it was in the bottom 75%. If they were nonconcordant, centers were provided with registry accession numbers for the patients who did not receive the recommended therapy to enable them to review and update their records. Winthrop’s data, at the time of initial reporting, was concordant for this measure, ( Tables 1 and 2 ) so there was little incentive to change treatment patterns.
| Performance Rates and Reported Cases | |||||
|---|---|---|---|---|---|
| 2004 | 2005 | 2006 | 2007 | All | |
| Radiation therapy is considered or administered within 6 mo (180 d) of diagnosis for patients <80 y with clinical or pathologic AJCC T4N0M0 or stage III receiving surgical resection for rectal cancer: | |||||
| Estimated performance rates (%) | 100 | 100 | 100 | 100 | 100 |
| Performance rate (numerator/denominator) | 4/4 | 1/1 | 4/4 | 3/3 | 12/12 |
| Total number of rectum cancer cases reported to NCDB | 25 | 27 | 31 | 19 | 102 |
| Performance Rates and Reported Cases | |||||
|---|---|---|---|---|---|
| 2004 | 2005 | 2006 | 2007 | All | |
| At least 12 regional lymph nodes are removed and pathologically examined for resected colon cancer: | |||||
| Estimated performance rates (%) | 73.3 | 88.9 | 73.9 | 85.4 | 79.9 |
| Performance rate (numerator/denominator) | 44/60 | 40/45 | 34/46 | 41/48 | 159/199 |
| Total number of colon cancer cases reported to NCDB | 142 | 112 | 104 | 124 | 482 |
Beginning in 2008, the COC expanded its CP3R measures to 6, 4 of which were endorsed by the National Quality Forum (NQF). The new measures focused on 3 parameters in the treatment of breast cancer and 3 parameters in the treatment of colorectal cancer. For colorectal cancer, the measures continued the assessment of chemotherapy use for stage III colon cancers and added an assessment of the number of lymph nodes removed during resection of colon cancers and the use of radiation in the treatment of rectal cancer. These added measures provided an opportunity to study the quality of care provided by surgeons caring for colorectal cancer at our institution and form the basis for this report.
Materials and methods
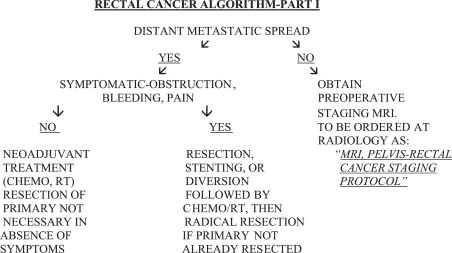
Data on the use of radiation for rectal cancer and the numbers of lymph nodes removed during colon resection for treatment of colon cancer for the years 2004 to 2007 were obtained from the CP3R information provided online to Winthrop by the NCDB ( Fig. 1 ). Review of the NCDB CP3R data on the use of radiation for patients less than 80 years of age with T4N0M0 or stage III rectal cancer showed that all 12 eligible patients at Winthrop for the years 2004 to 2007 were treated with radiation within the 180 days of diagnosis considered appropriate. However, only 12 of 102 patients with rectal cancer during these 4 years fitted the eligibility criteria for radiation treatment. Treating physicians considered that greater numbers of patients who had rectal cancers were receiving radiation and that further scrutiny of the registry data was in order.
Review of the NCDB CP3R data on the numbers of nodes harvested during resection of colon cancer for the years 2004 to 2007 showed, on average for the 4 years, that 79.9% of patients had at least 12 nodes removed. The year-to-year average varied from 73.3% for 2004 to 88.9% for 2005. Although these percentages seemed good, our surgeons did not think that they were as high as they would like them to be. Furthermore, the effect on patient care was uncertain, because the NCDB numbers did not indicate the frequency of nodal involvement for those patients having fewer than 12 nodes removed. If all these patients had negative nodes and did not receive chemotherapy for this reason, the potential effect on outcome would be greater than if the reverse were true.
To better assess the implications of the CP3R data provided by the NCDB, registry abstracts and charts were reviewed for rectal and colon cancer cases for the years 2004 to 2007. Additional colon cases for the years 2008 and 2009 were examined for more current information on the harvest of nodes during colon resection.
To evaluate whether deficiencies in nodal harvest were related to the use of laparoscopic colon resection, we performed a retrospective chart review of all colon resections, both laparoscopic and open, performed for cancer for the years 2008 and 2009. Parameters analyzed included specimen length, mesenteric length and height ( Table 3 ), and the number of harvested lymph nodes ( Table 4 ). The rank-sum test was used to compare groups, because the data were skewed. The Fisher exact test was used to find differences in rates between the groups having 12 or more nodes examined ( Table 5 ).
| Laparoscopic Right Colectomy (n = 43) | Open Right Colectomy (n = 59) | Laparoscopic Left Colectomy (n = 26) | Open Left Colectomy (n = 68) | |
|---|---|---|---|---|
| Mean | Mean | Mean | Mean | |
| Total length (cm) | 27.4 | 35.5 | 22.5 | 23.5 |
| Ileal length (cm) | 6.46 | 8.54 | NA | NA |
| Colon length (cm) | 21.2 | 27.3 | NA | NA |
| Mesenteric length (cm) | 21.8 | 26.9 | 22.3 | 22.4 |
| Mesenteric width (cm) | 5.88 | 7.15 | 6.1 | 6.6 |
| Side | Lap Surgery | Open Surgery | Both Methods | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | |
| Right | 43 | 20.5 a | 8.9 | 59 | 20.6 a | 9.2 | 102 | 20.6 a | 9.0 |
| Left | 26 | 13.8 | 8.3 | 68 | 17.0 | 7.9 | 94 | 16.1 | 8.1 |
| Both Sides | 69 | 18.0 | 9.2 | 127 | 18.7 | 8.7 | 196 | 18.4 | 8.8 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree