The difficulties in establishing and delivering reliable clinical hematology and laboratory services in resource-limited settings are well recognized. However, much can be achieved by better use of existing resources through a concerted quality improvement approach. The recommendations of this article are based in part upon work in the thalassemias, inherited disorders of hemoglobin that are widely prevalent in Asia, which may serve as a model that is applicable to other common, chronic disorders in resource-poor settings. Available resources are highlighted and recommendations made regarding approaches to improving services. Over the last few years, a number of low and middle-income countries, obtaining support from appropriate governmental sources, have identified and overcome difficulties and significantly improved clinical services for patients with thalassemia.
Key points
- •
Every step in the sample journey, from initial request to timely delivery of results, needs to be considered to improve services.
- •
Quality improvement approaches offer opportunities to improve service delivery even within existing resources.
- •
Approaches to improve clinical services should benefit from focus on establishing continuity of care.
- •
National patient registries may serve to inform governments about the demands for increased resources for management.
Background
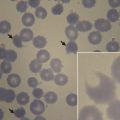
The recommendations of this article are based in part upon work in the thalassemias, inherited disorders of hemoglobin that are widely prevalent in Asia, which may serve as a model that is applicable to other common, chronic disorders in resource-poor settings. The decline in childhood mortality rates in Asian countries over the past four decades has resulted in substantial proportions of many countries’ health-care budgets now being consumed in the management of surviving patients. We had previously estimated that in Sri Lanka, the management of thalassemia could shortly require about 5% of the country’s health budget. Therefore, even in Sri Lanka where care has reached a commendable standard, it remains critical to continue to plan not only for programs for screening and counseling in thalassemia, but for improvements in clinical and laboratory services in patients whose lengthening survival is often associated with increasingly complex care.
Background
The recommendations of this article are based in part upon work in the thalassemias, inherited disorders of hemoglobin that are widely prevalent in Asia, which may serve as a model that is applicable to other common, chronic disorders in resource-poor settings. The decline in childhood mortality rates in Asian countries over the past four decades has resulted in substantial proportions of many countries’ health-care budgets now being consumed in the management of surviving patients. We had previously estimated that in Sri Lanka, the management of thalassemia could shortly require about 5% of the country’s health budget. Therefore, even in Sri Lanka where care has reached a commendable standard, it remains critical to continue to plan not only for programs for screening and counseling in thalassemia, but for improvements in clinical and laboratory services in patients whose lengthening survival is often associated with increasingly complex care.
Improving clinical services in resource-poor settings
The approaches suggested here to improve clinical services include education to increase the knowledge base about thalassemia, including approaches to long-distance education. Improvements in the delivery of care will include those in clinical facilities as well as in the organization of health care, with emphases on continuity of care and on accountability. Meticulous approaches to history and physical examination and to record keeping in local clinics may assist development of national programs of data management. Extending the access to essential medicines is a critical issue in almost all Asian countries. As well, there is a view — not usually overtly expressed — in many countries that thalassemia is a hopeless disease in which a substantial investment is wasted. This requires efforts to change attitude s within health care systems and governments who may not provide many basic health services to their citizens. South-South partnerships may be critical in many of these approaches (See Fucharoen S, Weatherall DJ: Progress towards the control and management of the thalassemias , in this issue).
Expansion of Medical Education
Early investment to increase the knowledge base in the thalassemias, beginning in medical school and including training in pediatrics and hematology, would represent a long term positive investment in improving clinical management of these complex disorders. Examples are illustrated from Sri Lanka.
Medical school
In Sri Lanka exposure to thalassemia in medical school includes a few lectures on hematologic disorders, including thalassaemia, two practical laboratories including one during the later clinical rotation and, during clinical clerkship, opportunities to manage patients.
Pediatrics
As in many other countries in Asia, in Sri Lanka thalassemia patients are generally managed by pediatricians, many of whom may have received limited exposure to thalassemia following medical school. Over 4 years of pediatric training, including one as a registrar, a week-long, largely laboratory-based, rotation in hematology is provided. During a mandatory subsequent year of training overseas, there may be opportunities to manage patients with thalassemia (Professor Sanath Lamabadusuriya, personal communication, 2015).
Hematology
Thalassemia patients in Sri Lanka are not managed by hematologists, whose training, as per the traditional British model, focuses primarily on laboratory experience with less extensive clinical training. During 4 years of formal laboratory training and a relatively shorter period of clinical training, there may be no experience in thalassaemia, although there may be clinical exposure during years as a registrar, or overseas (Dr Senani Williams, personal communication, 2015).
The upshot of all this is that a newly-qualified pediatrician may be charged with responsibility of hundreds of patients in a rural setting, despite limited expertise and experience in either laboratory or clinical problems of thalassaemia; in parallel, individuals who have extensive hematology training in thalassemia may possess limited understanding of clinical issues. Similar situations exist in other emerging countries, but may be evolving, as they are in Sri Lanka. In Sri Lanka at present approximately ten pediatricians and a few consultant hematologists are trained annually. The doctor-patient ratio in 2010 in Sri Lanka was 0.7/1000 population (compared to 2.7 in the UK, 2.4 in the United States, and 2.1 in Canada); in many emerging countries, this ratio is much lower. Yet even in countries where chronic understaffing may be accepted as inevitable, the optimal arrangement and one that would improve care without additional extensive financial outlay is a network of dedicated clinicians, working with designated laboratories, in a few expert centers.
Possible approaches to change
Expansion of the medical school curriculum to include exposure to the evidence for current practices in thalassemia, with emphasis on independent guidelines of management, may stimulate early scientific interest in this fascinating disease. Following medical school, more comprehensive laboratory training for pediatric trainees and extended clinical rotations for those in hematology might usher in a new era of cooperative care. Some of the country’s prominent pediatricians have suggested that in future, defined periods spent in dedicated thalassemia units be mandated as part of pediatric training. These units need to be expanded to more centers, given that in many emerging countries many patients live hours from the closest center of excellence with a potential inaccessibility to expert care. Efforts to expand the expertise that is often concentrated in urban centers have been assisted over the last decade with advances in communication technology, including the potential for telemedicine to play a potential role.
Improved Delivery of Care
Organization of clinical facilities
In many emerging countries, in the absence of hemoglobin screening programs, thalassemia patients are often first diagnosed during an admission to an emergency department, where a variable range of understanding of thalassemia care may be encountered. In Sri Lanka, if admission is required, a patient aged older than 13 years (the age after which a child is registered as an “adult”) will be admitted to an adult ward. If a pediatrician trained in thalassemia management (or if expert “on call” advice was available), a child could be reviewed and if necessary admitted to a pediatric ward, improving continuity of care. With respect to thalassemia outpatient management, a separate facility need not be a freestanding structure. Two or three dedicated rooms, including a transfusion and treatment area, a (private) patient consultation area and, if possible a waiting area, are sufficient.
Re-organization of the structure of the health care team
Arguably the most effective approach to improve clinical services for this disorder would be to ensure continuity of care . Efforts to establish dedicated expert centers in which interested, motivated pediatricians and hematologists act as Thalassemia Center Directors with extended terms of appointment, who supervise all care and mentor junior staff, would improve a common arrangement by which senior staff relocate every few years. Prior to taking up a post as a Thalassemia Center Director, dedicated short courses could be provided to consultants interested in thalassemia management, who would then be assigned ultimate responsibility for all patients, if not permanently, for extended periods.
Management guidelines providing evidence-based recommendations for clinical assessment, medication use, and patient monitoring that is tailored to the center can be provided. Regular review of all clinical and laboratory data on each patient, at not longer than 3-month intervals, and seminars and meetings focusing on evidence-based management, will maintain compliance with management guidelines. Interest can thereby be promoted in trainees, for whom a process should be established for regular attendance at each center. Because ongoing assessment of complications including those in the cardiac, hepatic and endocrine systems is critical in thalassaemia care, relationships with consultants in the relevant sub-specialities should be established, and may help to expand sub-networks of interested and expert care. Related to continuity is accountability in care. The concept of a minimum standard of care, even in rural settings, is of critical importance. Regular mortality/morbidity rounds to document causes of death, complications, and parameters of iron control can evaluate the compliance with management guidelines, and direct optimization of care. The use of quality assessments by impartial independent reviewers can help guide physicians in appropriate practices.
In parallel, it is equally important that staff morale be maintained. Efforts toward academic work should be encouraged and promoted. Not only Center Directors, but others including nursing staff, should be provided with opportunities for continuing medical education, both locally and abroad.
Emphasis on clinical skills and ‘low tech’ approaches to care
Clinical care may be facilitated by encouraging what could be termed “low tech” approaches with a targeted meticulous approach to history and physical examination and careful record keeping. Boxes 1 and 2 highlight some important points from the history and physical examination, using the example of thalassemia, which when documented over time allow substantial understanding of the patient’s status.
Date of diagnosis
Presenting symptoms and signs at diagnosis
Hemoglobin prior to first transfusion
Date of first transfusion
Date of initiation of regular transfusions (8 or more transfusions/year)
Reasons for initiation of regular transfusions, if applicable
Transfusion history including regular update of number of transfusions received to date
Year of initiation of iron-chelating therapy if applicable
Initial clinical parameters at initiation of iron-chelating therapy
Year of, and indication for, splenectomy if applicable
Compliance with medication
Age at menarche (and mother’s age at menarche if available)
Documented meticulously in the clinical record on each visit, the following allows substantial understanding of the patient’s status.
- •
In children, height and weight and comparison with healthy siblings to identify potential growth attenuation commonly observed in thalassaemia; in adults, comparison to parental height;
- •
Spleen size to permit evaluation of extramedullary activity, indications for increased intensity of transfusions, and/or consideration of splenectomy;
- •
In older patients, Tanner staging to permit identification of pubertal delay and failure and interpretation of growth pattern;
- •
In all patients, hematocrit and date of each unit of packed cells administered, to estimate annual iron accumulation and the cumulative body iron burden;
- •
In all, pre-transfusion hemoglobin (by automated counters) including to identify early hypersplenism, evaluate growth difficulties, interpret marrow expansion;
- •
In children greater than 4 years, bone age to interpret potential delays of linear growth;
- •
In all patients annual facial photography to record potential bony expansion.
Data management
In our experience at the National Thalassemia Center in Sri Lanka, the presence of an efficient, dedicated, multi-tasking clinic manager with broad responsibility but above all that for organizing data and charts, has been extremely valuable. Data does not have to be recorded electronically; indeed, this is often not practical in many settings. Where sufficient staff are available there is value in developing a local data base which among other goals, permits tracking of numbers and of local statistics; a uniform country-wide system of recording clinical and laboratory data assists in evaluation of national trends. It is a common but, in our view, inadvisable practice to have the patient keep even limited medical records at home as these may often be misplaced. Finally, as identified in other chronic disorders maintenance of a national registry by a trusted source may assist the understanding by the government of the necessity to increase resources for care.
Increased access to essential medicines
In many cases high drug prices, often the result of intellectual property “protection”, are a serious barrier to access to essential medicines. Efforts to reduce drug prices are opposed by many industrialized countries and the pharmaceutical industry. The potential solutions to this are complex, including alliances with Health Directors and ministries, education and organization of parents’ groups, and continued resistance from humanitarian organizations.
Changes in attitude
Changes in the perception of thalassemia is critical to the success of the initiatives outlined above. There remains a contrast between the expectations of care in richer countries for thalassemia and many other once predictably-fatal disorders which have evolved to a chronic disease, and emerging countries, in which many patients remain under-diagnosed and under-treated. However, even in countries lacking the public health system of Sri Lanka, survival in thalassemia has almost doubled over the past four decades, due primarily to the wider availability of iron-chelating therapy. Given recent initiatives in India, the previously discouraging general lack of access to chelation therapy may be changing.
Governments, companies interested in corporate social responsibility, and interested charities may be accessed to provide resources with varying success. As an example, our charity, Hemoglobal in cooperation with a private health facility in Sri Lanka, recently was able to begin quantitative testing to evaluate iron overload in vivo . Following this effort, the Sri Lankan Director General of Health reinforced the commitment to make such monitoring available annually for a cohort of patients. Similar approaches may be feasible in other countries.
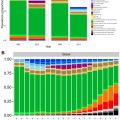
Of course, as long as governments do not support basic health priorities including sanitation and immunization, thalassaemia — whatever its prevalence — will not be conceived as a high national priority. But there is no doubt that continued lack of attention leading to poor physical, psychological and social functioning, as these patients survive but develop irreversible complications, is increasingly costly in social and economic terms. Furthermore, experience in other diseases also shows that governments respond to pressure and that individual efforts to improve care and awareness may have long-lasting impact. Our own experience in Sri Lanka emphasizes that even one dedicated individual, over years of effort, can increase the involvement of a government willing to listen. One example includes the observed doubling over the past 20 years, in Sri Lanka, of the use of iron-chelating therapy. Still another is the initiation of a screening, education and prevention program in Sri Lanka, where the government has recognized that such approaches are key to reducing the burden of disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree