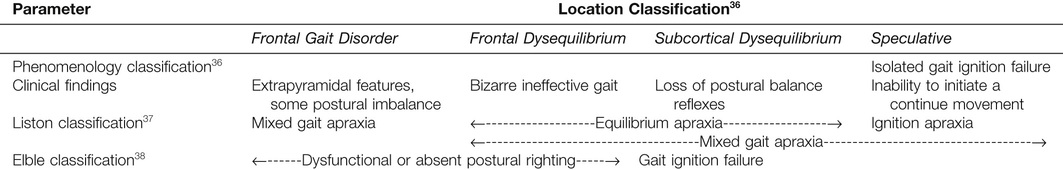
Nancy L. Low Choy, Eamonn Eeles, Ruth E. Hubbard Impaired mobility and balance dysfunction each become more common with aging. Acute changes in each (“off legs,” falls) remain among the “geriatric giants” or now, as they increasingly are called, acute geriatric syndromes. Whether slower changes in mobility and balance are physiologic (and inevitable) or pathologic (and potentially mutable) remains unclear. The accumulation of deficits, including those that affect motor performance, may be inevitable at an advanced age. However, factors such as sedentary behavior, emergence of chronic diseases, and low levels of physical activity, which all make significant negative contributions to mobility integrity, can be mitigated. This chapter addresses impaired mobility and the integral relationship with balance, but does not focus on the issue of falls, the theme of Chapter 103. We briefly review some essential features of how mobility changes with age. This is approached from a hierarchical perspective that includes higher order, executive function through gait speed to gait initiation, transitions from sitting to standing and, finally, from lying to sitting. Next, we describe some common gait disorders and how a structured approach to assessment can facilitate their classification. The clinical assessment of balance and mobility for older adults is reviewed to highlight strengths of specific tools for management in community and hospital settings. Finally, we explore the relationship between impaired mobility and frailty and appraise current interventions for impaired mobility across the frailty spectrum. Mobility is the term used to refer to a number of fundamental daily activities that range from walking to sitting and standing tasks to in-bed mobility. In this section, we explore the age-related changes that occur with each of these activities, providing a foundation for the assessment and management of balance and mobility. Walking was traditionally seen as an automatic task requiring little input from higher mental functions. However, an intricate interaction between gait and executive function is now recognized.1 Older healthy adults with the greatest declines in executive function, relative to cognition, exhibit impaired functional mobility2 and experience more falls.3 As executive function declines, an increase in the double support phase and step time of the gait pattern occurs.4 Studies investigating dual tasks, which are dependent on intact executive function, have demonstrated that older adults are less able to maintain normal walking while performing an additional task, particularly talking.5 Even in physically fit older adults, dual tasks influence balance during walking through a direct effect on body sway and stride variability and an indirect effect on gait velocity.6 Task shifting when multitasking is also impaired with aging, with inhibitory control, mental set shifting, and attentional flexibility predictive of functional mobility in older adults.7 The pathophysiology of these changes may originate in the prefrontal cortex, which plays a crucial role in executive functioning and is particularly vulnerable to microvascular damage.8 Hypoactivation of the medial frontal gyrus, a region involved in motor planning, is linked with falls in older adults7 although, intriguingly, frontal executive network disruption does not appear to be predictive of fallers.9 Pilot studies have shown that targeted executive function training is feasible and may improve gait parameters, including balance.10 Older adults tend to walk more slowly than young adults. In a nationally representative sample of community dwellers in Ireland, usual walking speed declined after the age of 50 years, with the most pronounced drop after age 65.11 Although this sample excluded patients with severe cognitive impairment, dementia, and Parkinson disease (PD) and those living in residential care facilities, individuals with chronic disease were included. This raises the question of whether declines in gait speed are secondary to pathologic processes rather than being age-related changes. Studies of the fittest older adults support the latter hypothesis. Cross-sectional investigations of elite athletes have shown reductions in speed and endurance of approximately 3.4%/year between 50 and 74 years, with notable acceleration after older adults 75 years.12 However, although some slowing of gait speed is to be expected with increasing age, there is a growing body of evidence to suggest that this may not be benign. Generally speaking, gait speed is reflective of overall health status. The mean walking speed of older community dwellers is significantly faster than their age-matched peers in the hospital13 or in residential care facilities.14 Slow gait speed is also associated with adverse outcomes. A systematic review of 27 different studies has concluded that slowness (measured by walking at a usual pace over 4 m) identified autonomous older adults at risk of future disability, cognitive impairment, and institutionalization.15 Similarly, in pooled data from 34,485 people older than 65 years followed for between 6 and 21 years, survival increased across the full range of gait speeds, with significant increments per 0.1 m/sec.16 Gait speed has therefore been advocated as a marker of frailty, either exclusively17 or in combination with other markers of strength and vitality.18 Indeed, in a study of seven potential frailty criteria, including weakness, weight loss, and exhaustion, slow gait speed was the strongest predictor of chronic disability and the only significant predictor of falls.19 The dynamic nature of frailty has also been explored and supported by the measurement of mobility changes in older adults.20 The cause of slow gait speed has not yet been fully elucidated, but cerebrovascular disease is likely to be the key pathophysiologic factor. Slow walking has been linked to white matter hyperdensities and with gray matter changes in the medial temporal area.9,21 A smaller volume of the prefrontal area seems to contribute to slow gait through slower information processing and motor planning.22 Similarly, the association between faster gait speed and larger cerebellar gray matter volume is significantly influenced by information-processing ability.23 Hypertension may also be a critical contributor. In the Cardiovascular Health Study, hypertension accelerated slowing of gait speed24 and mediated the association between the degree of white matter hyperintensities and mobility impairments.25 Gait initiation requires the integrated control of limb movement and posture and is achieved with purposeful postural shifts at toe off, including relaxation of the triceps surae for swing and synergistic contraction of ventral, hip abductor and quadriceps muscles for support, modulated by controlled knee flexion mid stance. These culminate in a forward step, with steady-state velocity being achieved in less than two steps.26 Gait initiation is well preserved in healthy older adults.27 Abnormalities of gait initiation are a sensitive but not specific sign of disease processes in older adults, such as those with PD, multiple cerebral infarcts, normal-pressure hydrocephalus, progressive supranuclear palsy, and cervical myelopathy. The ability to stand from a bed or chair is a critical aspect of mobility, independently predicting mobility disability and activities of daily living disability in community-dwelling older adults.28 The activity of standing up involves a number of phases, including the following: (1) a preparatory phase that positions the feet for weight acceptance, along with forward inclination of the trunk to shift the center of mass forward over the feet; (2) a peak force phase, enabling weight acceptance onto the feet to commence standing up; (3) a phase of controlled extension enabling attainment of upright stance; and (4) a stabilization phase in stance that enables the individual to remain steady.29 Inefficient preparatory patterns may occur when people are obese30 or present with chronic obstructive airway disease,31 along with PD or some other neurologic gait disturbance.27 Reduced range of motion in the hips, pelvis, knees, and spine is common with aging and impedes the initial shift of the total body center of mass over the feet. Weakness of the hip girdle muscles is also a frequent finding in older adults and is a manifestation of general deconditioning, and those affected may need to use their arms to help themselves up. Chair stands are sensitive to changes in postural control, strength, and coordination and thus are useful as a physical performance measure32 for frail and high-function older adults. One study of older adults has shown the importance of the start position in bed and strength in the upper limbs when weak trunk musculature makes it difficult for older adults to sit up over the bed edge.33 Preparatory positioning of the person (rolling the person onto his or her side or elevating the bed head), in conjunction with use of the upper limbs, can provide effective assistance during sitting over the bed edge when trunk muscles are weak.34 In addition, the lower limbs can be used for added momentum if well-timed with upper limb and trunk components. When trunk muscles are weak, ongoing reliance on the upper limbs for support during sitting up and sitting will be required.34 Thus, for an older adult to be independent in getting out of bed, muscles of the trunk and upper and lower limbs need to be targeted in intervention programs. Gait disturbances associated with aging are often multifactorial, a combination of sensory, neurodegenerative, and negative mental-cognitive biofeedback.35 Pragmatically, disorders of gait may be divided into those that are clinically obvious and others that are less apparent. The following gait patterns would be evident to experienced clinicians and are classified according to level of impairment and interaction with the nervous system36: Middle-level disorders include the following: Lowest level disorders include the following: Because these disorders are covered in other chapters, here we shall concentrate on gait disorders that may present more of a diagnostic challenge. The term gait apraxia has largely been superseded by the term higher level gait disorder. This is based on abnormalities of the highest sensorimotor systems and assumes integrity in basic sensorimotor circuitry.36 Gait pattern in higher level disorders is attributed to a motor programming failure comparable to the problems encountered in PD. These abnormalities can be classified according to their functional or neuroanatomic associations. Even so, their exact nature is still debated, and the present uncertainty is reflected by the many classification systems that have been proposed (Table 102-1).36–38 For locomotion, interrelated higher level structures (the corticobasal ganglia–thalamocortical loop) meet the demands of the personal desire to move and the maintenance of posture within the confines of environmental limitations.38 Pathology in any of these regions or their connections therefore results in an array of gait disorders, such as the following: • Suppression of conversion of personal will into task execution manifesting as hesitation or freezing and problems initiating gait or making turns (particularly affected by abnormalities of the supplementary motor area and its connections)38 • Dysfunctional processing with gait adversely influenced by emotional and environmental information • Dysfunctional or absent postural righting reflexes, resulting in injurious falls • In contrast to hypokinesis implicit in basal ganglia underactivity, disturbance in basal ganglia function may also lead to excessive, involuntary and uncontrolled limb movements.39 Classifications of gait have been criticized for their lack of consistency.37 The Nutt classification, for example, includes frontal gait disorder, cautious gait, frontal disequilibrium, and cortical disequilibrium as distinct entities.36 The older adult, with accumulation and overlap of pathology, may exhibit problems of higher gait that are not reducible to such discrete categories. Distinct gait parameters have been identified by Liston and colleagues according to their own clinically proposed subtypes.37 This allows for the theoretical inclusion of mixed pathology and gait subtypes. The amalgamation of disordered balance in conjunction with ineffective gait by Elble38 seems a sensible if not altogether precise way to overcome the lack of connection between the site of pathology and physical characteristics of the gait disturbance. The phenomenologic entanglement of cautious gait is worthy of consideration.40 Frequently multifactorial, a cautious gait may be more classically considered as a sensory disorder across locomotor afferent axes—vestibular, visual, or peripheral nervous system.41,42 The slower gait speed associated with loss of balance confidence and fear of falling implicates a compensatory consolidation of remaining locomotor sensorimotor processing. Cautious gait may be entirely appropriate in the setting of a recent fall, with loss of confidence or a perceived fear of falling.40 Cross-sectional studies have suggested that a cautious gait is common and is associated with poor standing balance, depression, anxiety, fear of falling, and reduced strength.41,43 It is these features that indicate a cautious gait as a marker of high risk but one potentially amenable to targeted interventions. The distinction between dysfunctional and excessive compensatory mechanisms and a primary disturbance of gait is important.44 Identification and attempted correction of underlying factors contributing to the syndrome of cautious gait should precede attribution of a primary gait disorder.43 In direct contrast to cautious gait, those with careless gait15–17 exhibit disinhibition of movement, with an inability to match their judgment to their physical limitations or the hazards posed by the external environment. Although many studies have reported that older adults with dementia walk slowly,45 if their overall degree of physical impairment is taken into account (e.g., use of walking aids, functional impairment), they may actually walk too quickly.46 Such recklessness implicates frontal lobe disturbance, as noted, and may account for the high incidence of injurious falls observed in those with dementia. Similarly, in hospitalized older adults, those with delirium are at increased risk of falls because of excessive ambulation and lack of insight into mobility problems.47 Conceivably a motor expression of dysexecutive syndrome, and therefore measurable, the development of tools to test ambulatory impulsivity would have clinical utility and the potential to predict risk. Drug burden exponentially challenges the vertical and multiple pathways involved. This may be less of a direct effect on the locomotor system, except in the case of extrapyramidal consequences of neuroleptics, and more an impact on the executive-cognitive hierarchy. Any drug or combination that impinges on sentient capability can affect mobility adversely and will make a preexisting mobility impairment even more precarious.48 Conversely, treating cognitive impairment may improve gait characteristics, showing that assessment and thoughtful pharmacologic management of cognition is the prerequisite of a holistic approach to the optimization of mobility.49,50 Community ambulation imposes challenges to mobility and balance through the demands of speed, distance, surface (e.g., cement, gravel, sand), terrain (e.g., slope, curb, and road challenges) and stairs that is further challenged by dual tasks (e.g., talking, carrying objects), objects in the environment (e.g., people, animals, physical structures), different lighting (e.g., dark, dim, shade, sunlight), and weather conditions.51 Balance is integral to mobility and may be associated with stabilizing activities (e.g., preserving upright posture while standing), more dynamic and adaptive responses to internal perturbations, or reactive responses to external perturbations.52 Balance and gait impairments can be quantified using different tests. These measure varying balance parameters, gait speed, and impact of other graded challenges, including secondary tasks that require attention and higher order executive function. A range of balance and mobility tools32,53–76 is summarized in Table 102-2 in relation to reliability, validity, performance norms for older adults, sensitivity to change across short (e.g., acute hospital stay) or longer time periods (e.g., subacute rehabilitation, community-based care), and ability to predict adverse health or fall outcomes. The functional gait assessment,72–77 BEST test and mini–BEST test,69–72 and timed up-and-go (TUG) test, with or without dual task components,60–64 have emerged as the stronger tools to consider in relation to outcomes and for predicting risk of falls in rehabilitation and community contexts. Evidence has also suggested that monitoring backward walking78 and stair climbing in conjunction with gender and fear of falling79 are critical elements indicating the risk of falls in home and community settings. TABLE 102-2 Measures of Balance and Gait for the Hospital, Rehabilitation, or Community Settings
Impaired Mobility
Introduction
Age-Related Changes in Mobility
Executive Function
Gait Speed
Gait Initiation
Transitions Into Standing from Sitting
Transitions from Lying to Sitting Over the Bed Edge
Common Disorders of Gait
Clinical Assessment of Balance and Mobility
Clinical Balance and Gait Measures
Items Rated or Measured by Scale or Test
Reliability and Validity for Older Adults
Normative Data for Older Adults
Predictive of Adverse Health or Falls and Fall Risk
Floor and Ceiling Effects
Clinical Test for Sensory Integration of Balance (CTSIB)53,54
Well established53
Pass-fail; 30-sec trials53
Failed trials on foam EO/EC linked to adverse health and fallers54
Ceiling effect with higher functioning older adults
Five times sit to stand (5×STS)32,55,56
Time to complete standing up and sitting down five times
Well-established acute and rehabilitation settings32,55
60-69 yr = 11.4 sec; 70-79 yr = 12.6 sec; 80-89 yr = 14.8 sec55
No ceiling effect; real change = 2.5 sec56
Berg Balance Scale (BBS): 0-56 points57–59
14 items rated 0-4—sitting, standing, transfers, stepping, 360-degree turn, pick up object on floor
Well established across settings
Ceiling effect with higher functioning older adults
Timed up-and-go (TUG) test—TUG manual; TUG cognitive60–64
Time to stand, walk, turn at 3 m, return to chair and sit down60,61
Well established across acute, rehabilitation, and community settings
60-69 yr < 8.5 sec; 70-79 yr < 9.5 sec63
10-m walk test (10MWT)65
10-m timed (sec) over 14-m walkway
Well established
Age-matched healthy adults = 1.36 m/sec
Not established
No ceiling effect
6-m walk test (6MWT)66
Distance walked over 30-m walkway
Well established
No ceiling effect defined
Dynamic Gait Index (DGI)—score 0-24; eight walking items rated 0-367,68
Standard—change walk speed; walk + head movements, pivot turn, step over and around obstacles, walk up and down stairs
Well established
Healthy older adults score = 21 ± 367,68
Ceiling effect with higher functioning older adults
BEST test—score 0-108; 36 items rated 0-3 (six categories of balance and gait tested)69–73
Biomechanical, stability, transitions anticipatory control, reactive control, sensory orientation, walking tasks and gait
Well established
Healthy older adults score >69%71
Predictive of fallers73
No ceiling effect established in older adults
Functional gait assessment—score 0-30; 10 items rated 0-373–77
Standard—change walk speed, walk + head movements, pivot turn, step over obstacles, heel-toe walk, walk with EC, backward walking, walk up and down stairs
Well established86,88
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Impaired Mobility
102