Although several cytokines have shown antitumor activity in renal cell carcinoma (RCC), the most consistent results have been reported with interleukin-2 (IL-2) and interferon (IFN). Recent insights into how the immune response to a tumor is regulated hold the promise of allowing patients to obtain a durable response to immunotherapy, perhaps without the significant toxicity associated with conventional approaches. This review describes how improvements in patient selection, combination therapy, and investigational agents might expand and better define the role of immunotherapy in metastatic RCC.
The ability of some renal tumors to evoke an immune response and the lack of benefit seen with standard chemotherapy and radiation led to the application of immunotherapy for patients with metastatic renal cell carcinoma (RCC). In an attempt to reproduce or accentuate this response, various immunotherapeutic strategies have been used, including adoptive immunotherapy, the induction of a graft-versus-tumor response via allogeneic hematopoietic stem cell transplantation, and the administration of partially purified or recombinant cytokines.
Although several cytokines have shown antitumor activity in RCC, the most consistent results have been reported with interleukin-2 (IL-2) and interferon-α (IFN-α). In contrast to the results seen with molecularly targeted therapies (eg, sunitinib), the administration of high-dose bolus IL-2 (HD IL-2) has consistently produced durable responses in a small percentage of patients with advanced renal cell cancer. However, the substantial toxicity and limited efficacy that is associated with HD IL-2 limits its application to highly selected patients treated at specialized centers.
Once the standard of care, the advent of novel therapies that target angiogenesis and signal transduction pathways has produced significant clinical benefits and prompted a reassessment of the role of immunotherapy for metastatic RCC. Recent insights into how the immune response to a tumor is regulated holds the promise of allowing patients to obtain a durable response to immunotherapy, perhaps without the significant toxicity associated with conventional approaches. This review describes how improvements in patient selection, combination therapy, and investigational agents might expand and better define the role of IL-2 in metastatic RCC.
Cytokine therapy
Although several cytokines have shown antitumor activity in RCC, the most consistent results have been reported with IL-2 and IFN-α. In contrast to the results seen with molecularly targeted therapies (eg, sorafenib, sunitinib), which lead to tumor shrinkage in most treated patients but do not produce remissions of cancer when therapy is discontinued, the administration of HD IL-2 has consistently produced durable responses in a small percentage of patients with advanced RCC. However, the substantial toxicity and limited efficacy that are associated with IL-2 have narrowed its application to highly selected patients treated at specialized centers. Although IFN-α has produced modest benefits in unselected patients, randomized clinical trials have revealed a small survival benefit with manageable toxic effects when compared with non–IFN-α control arms. As it became the de facto standard of care worldwide, regulatory agencies have supported the use of IFN-α as the control arm for randomized trials with targeted therapies that are described elsewhere in this issue. The results of these investigations have, in general, established the superiority of targeted agents in previously untreated patients, thereby narrowing the future use of IFN-α as a single agent in this setting.
In recent years, the relative merits of these low-dose and high-dose cytokine regimens have been clarified by the results of 4 randomized trials ( Table 1 ). In the most consequential trial, the French Immunotherapy Group randomized patients with an intermediate likelihood of response to IL-2 and IFN-α to receive medroxyprogesterone (control group), subcutaneous IFN-α, subcutaneous IL-2, or the combination of IFN-α and IL-2. Although significant toxicity was more common in the IL-2 and IFN-α arm, median overall survival did not differ between the arms. The investigators concluded that subcutaneous IFN-α and IL-2 should no longer be recommended in patients with metastatic RCC and intermediate prognosis.
| Trial | Treatment Regimens | N | Response Rate (%) | Durable Complete Response (%) | Overall Survival (mo) a |
|---|---|---|---|---|---|
| French Immunotherapy Group | CIV IL-2 | 138 | 6.5 | 1 | 12 |
| LD SC IFN-α | 147 | 7.5 | 2 | 13 | |
| CIV IL-2 + IFN-α | 140 | 18.6 | 5 | 17 | |
| MPA | 123 | 2.5 | 1 | 14.9 | |
| French Immunotherapy Group | LD SC IFN-α | 122 | 4.4 | 3 | 15.2 |
| LD SC IL-2 | 125 | 4.1 | 0 | 15.3 | |
| SC IL-2 + IFN | 122 | 10.9 | 0 | 16.8 | |
| National Cancer Institute Surgery Branch | HD IV IL-2 | 156 | 21 | 8 | NR |
| LD IV IL-2 | 150 | 13 | 3 | NR | |
| HD IV IL-2 | 95 | 23 | 7 | 17.5 | |
| CWG | LD SC IL-2/ IFN-α | 91 | 10 | NR | 13 |
| HD IV IL-2 | 95 | 23 | NR | 17.5 |
a The overall survival difference was not statistically significant in all cases.
Taken together, these studies suggest that high-dose intravenous (IV) bolus IL-2 is superior in terms of response rate and possibly response quality to regimens that involve low-dose IL-2 and IFN-α, intermediate-dose or low-dose IL-2 alone, or low-dose IFN-α alone. Consequently, although low-dose single cytokine therapy has a limited role in patients with metastatic RCC, high-dose IV IL-2 remains a reasonable option for appropriately selected patients with access to such therapy. More significantly, correlative biomarker investigations associated with these trials suggest that the potential exists for identifying predictors of response (or resistance) and limiting IL-2 therapy to those most likely to benefit.
Pathologic and molecular predictors of response to IL-2
Influence of Histologic Subtype
Responses to immunotherapy are most frequently seen in patients with clear cell RCC. This observation was detailed in a retrospective analysis of pathology specimens obtained from 231 patients (163 primary and 68 metastatic tumor specimens) who had received IL-2 therapy in Cytokine Working Group (CWG) clinical trials. For patients with primary tumor specimens available for review, the response rate to IL-2 was 21% (30 of 146) for patients with clear cell histologic primary tumors compared with 6% for patients with nonclear cell histologic tumors (1 responder in 17 patients). Among the patients with clear cell carcinoma, response to IL-2 was also associated with the presence of good predictive features (eg, more than 50% alveolar and no granular or papillary features) and the absence of poor predictive features (eg, more than 50% granular or any papillary features). As a result of these data, it may be appropriate for patients whose primary tumor is of nonclear cell histologic type or of clear cell histologic type but with poor predictive features to forgo IL-2–based treatment altogether.
Immunohistochemical Markers
Carbonic anhydrase IX (CAIX) has been identified as an immunohistochemical marker that might predict the outcomes of patients with RCC. In an analysis by Bui and colleagues, CAIX expression in more than 85% of tumor cells (high CAIX expression) has been associated with improved survival and a higher objective response rate in IL-2–treated patients. Building on this work, Atkins and colleagues developed a 2-component model that combined pathology analysis and immunohistochemical staining for CAIX. In a retrospective analysis, this model was able to identify a good risk group that contained 26 (96%) of 27 responders to IL-2 compared with only 18 (46%) of 39 nonresponders (odds ratio, 30; P <.01). A significant survival benefit was also seen for this group ( P <.01).
Molecular Markers
Through gene expression profiling of tumor specimens, Pantuck and colleagues were able to identify a set of 73 genes the expression of which distinguished complete responders from nonresponders after IL-2 therapy. In their hands, complete responders to IL-2 have a signature gene and protein expression pattern that includes CAIX, PTEN, and CXCR4. A similar analysis identified loss of chromosome 4, 9, and 17p as possible predictors of IL-2 nonresponse. Further investigation into these regions may improve our understanding of the molecular basis of an effective immune response in RCC. Although this approach requires prospective validation, it may become a powerful aid for clinicians in selecting appropriate treatment options.
Pathologic and molecular predictors of response to IL-2
Influence of Histologic Subtype
Responses to immunotherapy are most frequently seen in patients with clear cell RCC. This observation was detailed in a retrospective analysis of pathology specimens obtained from 231 patients (163 primary and 68 metastatic tumor specimens) who had received IL-2 therapy in Cytokine Working Group (CWG) clinical trials. For patients with primary tumor specimens available for review, the response rate to IL-2 was 21% (30 of 146) for patients with clear cell histologic primary tumors compared with 6% for patients with nonclear cell histologic tumors (1 responder in 17 patients). Among the patients with clear cell carcinoma, response to IL-2 was also associated with the presence of good predictive features (eg, more than 50% alveolar and no granular or papillary features) and the absence of poor predictive features (eg, more than 50% granular or any papillary features). As a result of these data, it may be appropriate for patients whose primary tumor is of nonclear cell histologic type or of clear cell histologic type but with poor predictive features to forgo IL-2–based treatment altogether.
Immunohistochemical Markers
Carbonic anhydrase IX (CAIX) has been identified as an immunohistochemical marker that might predict the outcomes of patients with RCC. In an analysis by Bui and colleagues, CAIX expression in more than 85% of tumor cells (high CAIX expression) has been associated with improved survival and a higher objective response rate in IL-2–treated patients. Building on this work, Atkins and colleagues developed a 2-component model that combined pathology analysis and immunohistochemical staining for CAIX. In a retrospective analysis, this model was able to identify a good risk group that contained 26 (96%) of 27 responders to IL-2 compared with only 18 (46%) of 39 nonresponders (odds ratio, 30; P <.01). A significant survival benefit was also seen for this group ( P <.01).
Molecular Markers
Through gene expression profiling of tumor specimens, Pantuck and colleagues were able to identify a set of 73 genes the expression of which distinguished complete responders from nonresponders after IL-2 therapy. In their hands, complete responders to IL-2 have a signature gene and protein expression pattern that includes CAIX, PTEN, and CXCR4. A similar analysis identified loss of chromosome 4, 9, and 17p as possible predictors of IL-2 nonresponse. Further investigation into these regions may improve our understanding of the molecular basis of an effective immune response in RCC. Although this approach requires prospective validation, it may become a powerful aid for clinicians in selecting appropriate treatment options.
Current investigation in patient selection
The CWG conducted the high-dose IL-2 Select trial to determine, in a prospective fashion, if the predictive model proposed by Atkins and colleagues can identify a group of patients with advanced RCC who are significantly more likely to respond to high-dose IL-2–based therapy (good risk) than a historical, unselected patient population. The preliminary clinical results of this trial revealed a response rate (28%) that was significantly higher that the historical experience with high-dose IL-2. However, analysis of proposed tumor biomarkers (eg, central pathology review and staining for CAIX) was unable to confirm hypotheses generated in retrospective studies and limit the application of HD IL-2. Efforts to confirm other proposed biomarkers (eg, CAIX SNPs, B7-H1 expression) are ongoing to understand tumor and host factors that predict for remissions after IL-2 therapy. An improved model for IL-2 patient selection will likely emerge from these efforts and improve its therapeutic index. Lessons from this work should guide the development of targeted immunotherapies (eg, CTLA-4, PD-1 antibodies) in solid tumors. As the list of effective therapies for metastatic RCC grows, improvements in patient selection will be necessary to ensure that patients who might attain a durable remission with immunotherapy do not miss this opportunity.
Combination of immunotherapy and targeted/antiangiogenic therapy
Although the role of low-dose single-agent cytokines is limited, combinations of immunotherapy with vascular endothelial growth factor (VEGF) targeted therapy may have merit. Two recently completed, large phase III trials of IFN plus bevacizumab versus IFN alone have shown superior efficacy with the combination regimen compared with cytokine monotherapy and suggest the potential of an additive effect.
Soon after bevacizumab became the first VEGF targeted agent to show efficacy as monotherapy in metastatic RCC, investigators explored the value of combining it with the de facto standard of care, IFN. Two phase III trials of IFN plus bevacizumab versus IFN (AVOREN and CALGB 90,206) were initiated in Europe and the United States for first-line treatment of patients with metastatic RCC. In both trials, patients were randomized bevacizumab plus IFN versus IFN alone. Unlike the CALGB trial, AVOREN (N = 649) was placebo-controlled, double-blind, and mandated previous nephrectomy. Compared with IFN alone, the combination arm in the AVOREN trial showed significantly better median progression-free survival (PFS) (10.4 vs 5.5 months; P = .0001), overall response rate (ORR) (31% vs 13%; P = .0001), and median time to progression (10.2 vs 5.5 months; P = .0001). The overall survival data analysis was subsequently published in 2010 and showed no significant survival difference between 2 arms (23.3 vs 21.3 months; P = .1291).
Further confirmation of the superiority of bevacizumab plus IFN to IFN alone came from the CALGB 90,206 trial. Unlike AVOREN, CALGB 90,206 was an open-labeled study and did not require previous nephrectomy. Relative to IFN alone, therapy with bevacizumab plus IFN significantly improved ORR (25.5% vs 13.1%, P <.0001) and median PFS (8.4 vs 4.9 months, P <.0001.) On the other hand, overall survival was similar in both arms: 18.3 months in the combination arm and 17.4 months in the IFN-only arm ( P = .097). Although the AVOREN and CALGB trials led to the regulatory approval of this combination of VEGF pathway inhibition with immunotherapy in patients with RCC, clarification of the relative contribution of IFN to this regimen requires a randomized trial comparing the combination with bevacizumab alone.
Bevacizumab has also been combined with high-dose IL-2 in a CWG phase II trial. Investigators reported a response rate of 28% and a median PFS of 9 months. These results suggest that these 2 agents may be given safely in combination and produce efficacy improvements that are additive but not synergistic. Sorafenib and IFN have been combined in 2 separate single-arm phase II trials. These trials showed objective response rates of 18% and 35%. Toxicity observed was typical of that observed with each single agent with a notable reduction in hand-foot syndrome compared with sorafenib monotherapy data. The benefit/toxicity ratio of this combination regimen awaits further investigation in randomized trials.
Investigational immunotherapy in RCC tumor vaccines
Metastatic RCC is a setting in which there has been great interest in testing novel immunotherapies. Several such approaches, including vaccination and allogeneic bone marrow transplantation, have been tested over the past 2 decades. The initial reports evaluating allogeneic bone marrow transplantation were encouraging; however, further clinical trials have highlighted the potential toxicity and limited applicability of this approach.
The use of tumor vaccines has been explored in RCC, in an effort to limit treatment-related toxicity and enhance tumor-specific immune responses. A variety of antigens associated with RCC have been identified, including MAGE-A6, MAGE 9, PRAME, and MUC1. Therefore, early clinical trials evaluated irradiated tumor cells or tumor lysate as a means of inducing antitumor responses. In the first published clinical trial reporting results of 120 patients, no improvement in PFS or overall survival was observed with treatment with irradiated autologous tumor cells given BCG. In contrast, results of a large multicenter randomized controlled trial evaluating an autologous tumor lysate-based vaccine in patients with high-risk nonmetastatic kidney cancer showed an improvement in PFS in vaccinated patients (5-year PFS 77.4% in vaccinated patients vs 67.8% in controls, P = .02). In a recent study, May and colleagues published results of 495 patients treated with an autologous tumor lysate-based vaccine in the adjuvant setting after undergoing radical nephrectomy for high-risk disease. Results were compared with a control group of 495 matched patients treated with nephrectomy alone. Overall survival at 5 and 10 years was 80.6% and 68.9%, respectively, in vaccinated patients, and 79.2% and 62.1%, respectively, in the control group ( P = .066). A statistically significant increase in overall survival was observed in the subset of patients with pT3 tumors (5-year overall survival 71.3% in vaccinated patients vs 65.4% in controls, P = .022). These data have yet to be confirmed in a randomized, controlled phase III trial.
Despite the presence of tumor-specific antigens, tumor cells lack appropriate costimulatory molecules and stimulatory cytokines to elicit an effective immune response. Therefore, in an attempt to augment effective immune response to vaccination, the use of renal carcinoma cells that have been genetically engineered to encode stimulatory cytokines and/or costimulatory molecules have been evaluated in phase I and II studies. Vaccination was well tolerated, and both complete and partial responses were observed, although in a minority of patients. Recently, tumor antigens have been engineered into vaccinia virus vectors. Trovax, a modified vaccinia Ankara (MVA) encoding the human oncofetal antigen 5T4, has been studied in phase I and II trials, which revealed suggestions of clinical efficacy. In a recent phase III clinical trial, 733 patients with metastatic RCC were randomized to receive Trovax versus placebo in combination with either sunitinib, IL-2, or IFN-γ. However, no difference in overall survival was observed in the Trovax-treated cohort. The magnitude of immune response to vaccination was associated with improved survival.
An alternative means of augmenting tumor antigen presentation and reversing tumor-induced anergy lies in the use of dendritic cell-based vaccines. Dendritic cells are potent antigen-presenting cells, uniquely capable of eliciting primary immune responses. Dendritic cell vaccines present tumor antigens in the context of dendritic cell-derived costimulatory molecules, resulting in effective antitumor immune responses. Several clinical studies have evaluated the ability of dendritic cell-based vaccines to elicit immunologic and clinical responses in patients with metastatic RCC. In a recent study, 18 patients with metastatic RCC were treated with autologous ex vivo generated dendritic cells loaded with autologous tumor lysate. Patients were treated with 5 cycles of intranodal injection with vaccine, in conjunction with a day continuous infusion of IL-2 (18 MiU/m 2 ) and 3 injections of IFN-α 2a every other day. Three patients showed a complete response, 6 patients showed a partial response, and 6 patients showed stable disease. Avigan has conducted studies evaluating a dendritic cell/tumor fusion vaccine, in which ex vivo generated dendritic cells are fused to patient-derived tumor cells. In 1 study, 23 patients were treated (10 patients with breast cancer, 13 renal patients with renal cancer) with escalating doses of dendritic cell /tumor fusion cells, ranging from 1 × 10 6 – 4 × 10 6 fusion cells. No significant treatment-related toxicity was observed. Tumor-specific immunity was assessed by measuring IFN-γ secretion by T cells after ex vivo exposure to autologous tumor lysate. Immunologic responses, defined as a 2-fold or greater increase in IFN-γ secretion by CD4 and or CD8 T-cell populations, was observed in more than half of patients. Five patients with renal cancer showed disease stabilization. In a subsequent study, patients with metastatic RCC underwent vaccination with allogeneic dendritic cell/tumor fusions. Of 24 patients who underwent vaccination, 2 patients showed a partial response, and 8 patients showed stable disease. A correlation between clinical and immunologic response was observed.
Although dendritic cell-based vaccines show promise, clinical responses are observed in a minority of patients. This finding may be in part because of the paradoxic increase in regulatory T cells that is observed in response to vaccination. In a recent study, peripheral blood mononuclear cells were isolated from 25 patients enrolled in a clinical trial in which patients with metastatic RCC were treated with autologous dendritic cells pulsed with tumor antigens given in conjunction with low-dose IL-2. The proportion of regulatory T cells increased more than 7-fold after vaccination compared with pretreatment levels. Strategies to deplete regulatory T cells and inhibit the effect of inhibitory pathways may be required to augment clinical response to vaccination strategies.
Overcoming obstacles to effective immunotherapy in RCC
An improved understanding of the molecular mechanisms that govern the interaction between a tumor and host immune response has provided insight into why immunotherapies too often fail to achieve satisfactory results. In RCC, obstacles to effective immunotherapy likely include the physiologic downmodulation of the immune response through the increased expression of molecules such as cytotoxic T-lymphocyte antigen 4 (CTLA-4) on the surface of activated T cells, the proliferation of regulatory (CD4+CD25+) T cells (T-regs) in response to nonspecific cytokine administration, and the immunosuppressive effects of increased circulating VEGF levels and myeloid-derived suppressor cells (MDSC). These insights have encouraged investigators to pursue agents that block T-cell regulation (eg, programmed death 1 [PD-1] and CTLA-4 antibodies), inhibit tumor-induced immunosuppression (eg, transforming growth factor beta [TGF-β] antibody, PD ligand 1 [PD-L1] antibody) and more specifically activate T cells (eg, CD137 antibody, IL-21), and dendritic cells (eg, toll-like receptor agonists) ( Table 2 ). Several of these approaches have shown encouraging efficacy in early trials both as single agents and in combination with standard therapies.
| Target | Drug | Class | Development Phase |
|---|---|---|---|
| Blockade of T-cell regulation | |||
| PD-1 antibody CTLA-4 antibody | BMS-936558 Ipilimumab | Fully human mAb Fully human IgG1 mAb | Phase I Phase III (melanoma) |
| Inhibition of tumor-induced T-cell function | |||
| TGF-β TGF-β2 | GC1008 AP12009 | Fully human mAb Fully human mAb | Phase I Phase I |
| T-cell activation | |||
| CD137 Cytokines | BMS-663,513 IL-21 | mAb Recombinant molecule | Phase I Phase II (melanoma) |
| Dendritic cell activation | |||
| Toll-like receptor Dendritic cell-tumor fusions | HYB2055 AGS-003 | TLR9 agonist Dendritic cell based immunotherapy | Phase II Phase III |
Investigational targeted immunotherapy
In a single-institution phase II trial, the CTLA-4 antibody ipilimumab produced major tumor regressions but also significant toxicities in patients with metastatic RCC who had failed previous immunotherapy. Toxicities associated with CTLA-4 antibodies, including enteritis, skin rash, and hypophysitis, have occasionally been life threatening and have also been associated with tumor response. Combination of cytokines and agents that block immune downregulation may prove particularly effective in select patients. A recent report of high-dose IL-2 and ipilimumab (CTLA-4 antibody) in patients with metastatic melanoma revealed manageable toxicity with a complete response rate of 17%, suggesting a potential role for this combination in patients with RCC. However, the combination of another CTLA-4 antibody (tremelimumab) and a VEGF tyrosine kinase inhibitor (TKI; sunitinib) proved more toxic than expected, in large part because of acute renal toxicity. Investigators at the Dana-Farber Harvard Cancer Center have recently launched a phase I trial of the combination of ipilimumab and bevacizumab in patients with metastatic melanoma. Should this combination prove tolerable, it should represent a rational combination for investigation in patients with RCC.
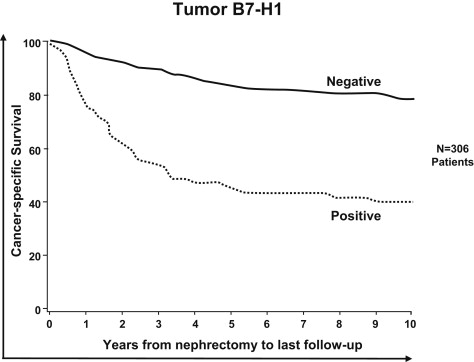
One of the most critical and promising pathways responsible for tumor-induced immune suppression in RCC is the interaction between B7-1, otherwise known as PD-1, and its ligand B7-H1 (PD-L1) interaction, which serves to restrict the cytolytic function of tumor-infiltrating T lymphocytes. Renal tumors that express B7-H1 have been shown to behave more aggressively, which leads to a shorter survival ( Fig. 1 ). Blocking the receptor (PD-1)/ligand (PD-L1) interaction with monoclonal antibodies (eg, PD-1 antibody BMS-936558, PD-L1 antibody MDX–1105), may facilitate immunotherapy and represents one of the most promising therapeutic strategies being studied in patients with RCC. These agents have recently completed phase I testing.
PD-1/PD-L1 biology
The PD-1/PD-L1 pathway is an important inhibitory pathway that regulates T-cell activation and mediates T-cell tolerance ( Fig. 2 ). The PD-1 receptor is expressed on T cells, B cells, monocytes, and natural killer T cells after activation. PD-L1 (B7-H1) and PD-L2 (B7-dendritic cell), the 2 ligands for PD-1, are expressed on antigen-presenting cells, including dendritic cells and macrophages. In addition, PD-L1 is expressed on nonhematopoietic cells, including pancreatic islet cells, endothelial cells, and epithelial cells, and they play a role in protecting tissue from immune-mediated injury.
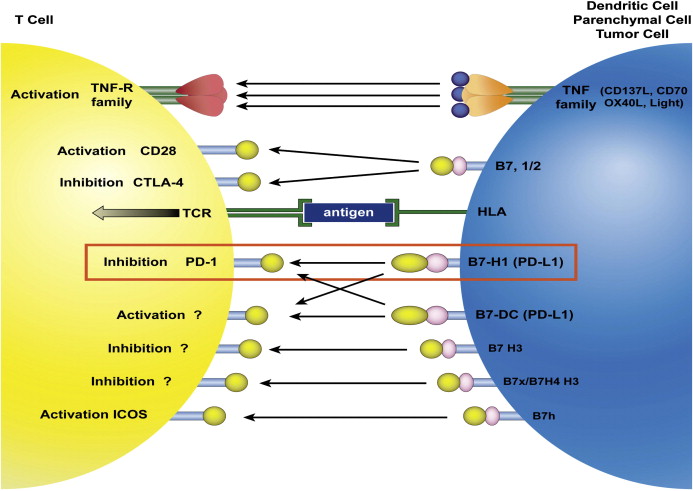
The critical role that PD-1 plays in blunting activated T-cell responses was first shown by the autoimmune phenotypes that develop in PD-1 knockout mice, including cardiomyopathy, diabetes, glomerulonephritis, and arthritis. PD-L1 expression on nonhematopoietic cells, including renal tubular epithelial cells, inhibits immune-mediated tissue damage, which indicates that the PD-1/PD-L1 pathway is a critical mediator of tissue tolerance. The PD-1/PD-L1 pathway plays an important role in modulating immune response to infection. T-cell expression of PD-1 is upregulated during chronic viral infection, which results in an exhausted T-cell phenotype. The lymphocytic choriomeningitis virus model was the first to show the impact of the PD-1/PD-L1 pathway in limiting clearance of virally infected cells.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






