- 18.1 Introduction
- 18.2 Pregnancy and maternal infection
- 18.3 Protection of the fetus and neonate against infection
- 18.3.1 Development of fetal immune responses
- 18.3.2 Placental transfer of IgG
- 18.3.3 Immunological value of breastfeeding
- 18.3.4 Reducing particular risks to the fetus/neonate from maternal infection
- 18.3.1 Development of fetal immune responses
- 18.4 Disorders of pregnancy
- 18.4.1 Recurrent abortions
- 18.4.2 Outcome of pregnancy in systemic lupus erythematosus
- 18.4.3 Pre-eclampsia
- 18.4.4 Fetal diseases due to alloimmunization
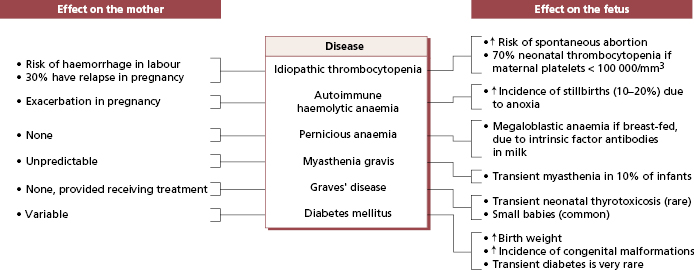
- 18.4.5 Organ-specific autoimmune diseases in pregnancy
- 18.4.1 Recurrent abortions
- 18.5 Clinical relevance of antibodies to reproductive components
- 18.5.1 Antibodies to hormones
- 18.5.2 Antibodies to sperm
- 18.5.1 Antibodies to hormones
 Visit the companion website at www.immunologyclinic.com to download cases with additional figures on these topics.
Visit the companion website at www.immunologyclinic.com to download cases with additional figures on these topics.
18.1 Introduction
In pregnancy, one-half of the transplantation antigens of the fetus are of paternal origin and, in an outbred species such as humans, these are different from those of the mother. The mother therefore carries a ‘mismatched’ fetus but, despite this, the fetus is not rejected. The reasons for this remain controversial and so the relationship between the local active recognition process (which allows successful implantation of the embryo and development of the placenta) and those systemic mechanisms that help maintain the pregnancy are not discussed. However protection of the fetus against infection is covered, as well as immunological disorders of pregnancy itself.
18.2 Pregnancy and maternal infection
Maternal mortality figures for the UK show that infection is the second most common cause of maternal death within 1 year of pregnancy, a figure that is consistent across the northern hemisphere. Worldwide, pregnancy is associated with a greatly increased risk of infection, particularly with malaria, toxoplasma or mycobacterial infections (tuberculosis and leprosy), which are particularly common in countries where malnutrition may be a major factor. However the risk still persists as illustrated in Case 18.1. Listeria is a risk as are toxoplasmosis and HIV, suggesting that there is reduced TH1 cell activity against intracellular pathogens during pregnancy. Pregnant women are advised to avoid unpasteurized dairy products. In addition all pregnant women are checked routinely for antibodies to sexually transmitted diseases.
 Case 18.1 A mother infected with Listeria
Case 18.1 A mother infected with ListeriaA 22-year-old primagravida stayed on a small-holding in France for the last 3 months of the pregnancy. She had been well, apart from morning sickness during the first 4 weeks of gestation. In France, she had been drinking fresh unpasteurized milk and eating home-made cheeses for 3 weeks when she developed fever, vomiting and diarrhoea followed by headache, myalgia and low back pain which persisted for 5 days. Four weeks later, at 28 weeks’ gestation, she went into premature labour and a still-born, jaundiced child was delivered after 36 h. At the baby’s post mortem, there was evidence of hepatitis, purulent pneumonia, conjunctivitis and meningitis. Listeria monocytogenes was cultured from several sites and a diagnosis of fatal neonatal Listeria monocytogenes infection was made. The organism was sensitive to ampicillin and gentamycin and since there was no longer a teratogenic risk (the pregnancy being over), the mother was given a 4-week course of both antibiotics in case organisms were silently sequestered in her deep tissues. Pregnant women are now all advised to avoid unpasteurized products throughout pregnancy.
Women should check their own immunization status for common viral infections (especially rubella, measles and polio) prior to pregnancy and avoid exposure to chickenpox if they are not immune. The more severe risks to the fetus are discussed in the next section later in the text.
18.3 Protection of the fetus and neonate against infection
The fetus and neonate are susceptible to both bacterial and viral infections by transplacental transfer and during vaginal delivery. The extent and nature of the infection depend not only on the type of infection but also on the immune maturity of the fetus at the time of infection. This, in turn, depends on the gestational age of the fetus (Box 18.1).
18.3.1 Development of fetal immune responses
The fetus becomes partially immunocompetent early in intrauterine life (Box 18.1), for example intrauterine infection with rubella virus provokes the production of fetal IgM antibodies against the virus as early as week 11. However, T-cell development is slow and this may account for the particular susceptibility of the fetus to viruses and intracellular bacteria. Plenty of T cells are detectable early in gestational life and T-cell numbers in blood are much higher at birth than in adults. However, their functional capacity develops late in fetal life, is still reduced at birth and increases in early life to reach adult levels in the first 2 months.
At term, although CD4+ cell numbers are high and IL-2 production is normal, production of other important cytokines, IFN-γ, TNF and TH2 cytokines, is low. Cytotoxic T-cell function is only one-third of that of adults and natural killer cell cytolysis is reduced also. These findings may account for the severity of neonatal infections with herpes simplex virus, cytomegalovirus, Listeria and Toxoplasma. Listeria, a facultative intracellular bacterium, is killed as a result of CD8+ cytotoxic T cells recognizing listerial antigen and MHC class I antigens on the surface of the infected histiocyte or hepatocyte. With reduced cytotoxic T cells and TH1 cytokine production, the fetus is more susceptible to intracellular and viral infections than the mother, as in Case 18.1.
The fetus is protected against bacterial infection by active transfer of maternal IgG across the placenta (see section 18.3.2). Fortunately, neutrophil leucocytes and macrophages are fully competent and plentiful in the circulation within a few days of birth.
18.3.2 Placental transfer of IgG
IgG is transferred across the placenta by means of specific receptors in the trophoblast for the Fc region of IgG, known as FcRn; these are the same receptors used for recycling IgG, albumin and probably IgA in mucosal cells (see section 1.2.4 and Fig. 7.18). Transfer begins at about 12 weeks, but most of the maternal immunoglobulin is transferred after 32 weeks of intrauterine life. Extremely premature babies therefore lack circulating maternal IgG at birth (Fig. 3.3) and are susceptible to bacterial as well as intracellular infections.
Infants with poor fetal growth also have lower levels of IgG at birth, due to poor placental transfer. Infants of very low birth weight (<1.5 g) have a high prevalence (up to 20%) of late-onset infections related to invasive procedures, with an infection-related mortality of 5–10%. Such infections are bacterial (involving staphylococci, enterococci, Klebsiella and Pseudomonas) and are notably those infections against which antibodies play an important protective role. Intravenous immunoglobulin (IVIG) infusions (0.5 g/kg per week) have been shown to reduce late-onset infections (like that in Case 18.2) in placebo-controlled studies in the USA. IVIG is not used routinely in the UK, since the rate of serious late-onset infections is <1%; this is probably due to avoidance of invasive procedures whenever possible.
 Case 18.2 Hypogammaglobulinaemia of prematurity
Case 18.2 Hypogammaglobulinaemia of prematurityStay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree