Liver imaging is a highly evolving field with new imaging contrast agents and modalities. Knowledge of the different imaging options and what they have to offer in primary and metastatic liver disease is essential for appropriate diagnosis, staging, and prognosis in patients. This review summarizes the major imaging modalities in liver neoplasms and provides specific discussion of imaging hepatocellular carcinoma, cholangiocarcinoma, and colorectal liver metastases. The final sections provide an overview of presurgical imaging relevant to planning hepatectomies and ablative procedures.
Key points
- •
Hepatocellular carcinoma (HCC) diagnostic criteria allow imaging diagnosis to supplant pathology.
- •
Determination of resectability is the main goal of imaging cholangiocarcinoma.
- •
MRI provides the best sensitivity for detecting colorectal metastases.
Introduction
Imaging has become an integral component of managing patients with suspected liver diseases and tumors. Options have evolved along with technology to provide important information and at times supplant pathology for diagnosis of liver lesions. This article provides an overview of the most common liver imaging modalities and their use in HCC, intrahepatic cholangiocarcinoma (ICC), and colorectal cancer (CRC) liver metastatic disease.
Introduction
Imaging has become an integral component of managing patients with suspected liver diseases and tumors. Options have evolved along with technology to provide important information and at times supplant pathology for diagnosis of liver lesions. This article provides an overview of the most common liver imaging modalities and their use in HCC, intrahepatic cholangiocarcinoma (ICC), and colorectal cancer (CRC) liver metastatic disease.
Liver imaging modalities
Ultrasound
Ultrasound basics
Ultrasound (US) is one of the oldest modalities in radiology. Transducers (probes) create sound waves that transmit through tissues and are variably impeded and reflected back to the transducer. Structures appear of varying echogenicity (brightness) based on their acoustic impedance/density. When performing transcutaneous US, transducers of different frequencies (lower frequencies of 3–5 MHz penetrate deeper than higher frequencies) are chosen based on the depth of the region of interest and tissues being penetrated. US gel is required to establish good acoustic contact because air acts as a reflector. Gray-scale and Doppler US have been used to evaluate focal liver lesions based on differences in echogenicity and vascularity; however, definitive diagnosis is often difficult. Transcutaneous US and in some instances endoscopic US can be used to guide percutaneous biopsies when imaging fails to provide definitive diagnosis.
Contrast-enhanced ultrasound
Diagnostic accuracy of US is greatly improved with the addition of contrast; however, to date, the use of contrast-enhanced US (CEUS) has been limited in the United States due to lack of Food and Drug Administration (FDA) approval. There are 3 contrast agents currently used worldwide: SonoVue (Bracco, Milan, Italy), Definity (Bristol-Myers Squibb, New York, NY, USA), and Sonazoid (GE Healthcare, Oslo, Norway). The first 2 act as vascular agents only, providing information regarding the early dynamic appearance of lesions with no diffusivity outside of the vessels (which is slightly different from computerized tomography (CT) and magnetic resonance [MR] agents). Sonazoid is taken up by the Kupffer cells and exhibits a hepatobiliary phase for approximately 1 hour after injection, which has been likened to the hepatobiliary phase on MRI and may be useful for lesion detection, as in metastatic work-ups. The main role of CEUS has been in focal liver lesion characterization and monitoring local ablative treatments. The benefits of CEUS are the real-time visualization of contrast enhancement, lack of nephrotoxicity, lack of ionizing radiation, and decreased cost compared with CT or MRI. The main disadvantage of CEUS is the relative lack of availability in the United States. Additionally, CEUS was dropped from the most recent American Association for the Study of Liver Disease (AASLD) guidelines due to the potential risk of misdiagnosis of ICC as HCC.
Computerized Tomography
Computerized tomography basics
CT is rapidly available, demonstrates high diagnostic accuracy for many indications, and is well known to radiologists and clinicians alike. Image creation on CT is the result of an ionizing radiation (x-ray) source, which rotates around the patient with detectors opposite the source that measure the degree of attenuation of the x-ray beam. The end result is a cross-sectional image with different attenuation values (brightness) assigned to different structures based on their relative attenuation coefficient (degree to which they impede the x-ray beam). Most soft tissues have similar attenuation properties; hence, intravenous contrast is used to improve conspicuity of organs, lesions, and vasculature.
CT contrast is composed of iodinated medium, which causes greater absorption and scatter of x-ray radiation, yielding increased attenuation (brighter appearance) of structures. The relative enhancement of organs is complex and related to an organ’s perfusion rate, tissue volume, composition, and permeability throughout the microvasculature. The initial enhancement is most influenced by the vascular supply and cardiac output, with later enhancement more dependent on intravascular dilution and redistribution of contrast within the extracellular space. Because iodinated contrast medium does not cross into the intracellular compartment, it can be assumed to distribute within the intravascular and extracellular compartments by way of diffusion or transcapillary exchange. A basic understanding of contrast pharmacokinetics allows greater appreciation for the different enhancement patterns (described later).
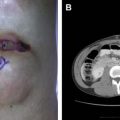
In the liver, there are well-defined postcontrast phases, during which the parenchyma follows a predictable pattern of enhancement. These phases consist of the late arterial, portal venous, equilibrium, and delayed phases. Most tumors within the liver (especially hypervascular lesions like HCC) receive preferential hepatic arterial blood supply compared with normal hepatic parenchyma, which is supplied predominately by portal venous blood. This differential blood supply allows for greatest lesion:background conspicuity of hypervascular tumors during the late arterial phase. Hypovascular tumors (many metastatic tumors) are generally seen most easily on the portal venous or equilibrium phases of contrast. A routine CT with contrast is usually timed for the portal venous phase; hence, arterially enhancing lesions may not be readily seen ( Fig. 1 ). In addition to improved conspicuity of lesions, the pattern of enhancement on the different phases of contrast helps narrow the differential diagnosis and in some instances is pathognomonic, such as in hemangiomas ( Fig. 2 ). Therefore, when assessing a liver tumor, multiple phases of contrast or a liver protocol CT should be obtained ( Table 1 ).
| Contrast Phases | Comments | Technical Specifications |
|---|---|---|
| Noncontrast |
|
|
| Late arterial phase |
| |
| Portal venous phase | Peak liver parenchymal enhancement, beginning contrast enhancement of hepatic veins | |
| Delayed phase | >120 s After injection, variable appearance |
Nephrotoxicity of computerized tomography contrast
Although CT contrast is essential to liver tumor characterization, it should be avoided in patients with poor renal function because it is potentially nephrotoxic. The American College of Radiology defines contrast-induced nephrotoxicity (CIN) as sudden deterioration in renal function after recent administration of iodinated contrast in the absence of another nephrotoxic event. Controversy exists as to the diagnostic criteria for CIN with variable definitions in the literature leading to a lack of consensus as to the actual incidence, risk factors, and diagnosis. The Acute Kidney Injury Network in a consensus group suggested the diagnosis of acute kidney injury could be made if one of the following criteria is met within 48 hours of a nephrotoxic event: absolute serum creatinine increase of greater than or equal to 0.3 mg/dL; percentage increase in serum creatinine of greater than or equal to 50%; or urine output reduced to less than or equal to 0.5 mL/kg/hour for at least 6 hours. Given that these creatinine changes are small, it remains controversial and difficult to apply these strict cutoffs in practice. In a retrospective study, including 8826 contrast-enhanced CT studies, administration of iodinated contrast was identified as a nephrotoxic risk factor in patients with estimated glomerular filtration rate (eGFR) less than 30 mL/min/1.73 m 2 and a trend toward significance in patients with eGFR 30 to 44 mL/min/1.73 m 2 . Clinical risk factors may also contribute to development of contrast-induced nephropathy, including diabetes, liver disease, chronic kidney disease, hypertension, low hematocrit, and heart failure. Policies for administration of contrast to patients with borderline function vary from institution to institution and screening patients who are potentially at risk is advised. See Table 2 for our institutional policy. Although there is abundant literature on the use of normal saline, bicarbonate drips, and other measures to reduce risk of nephrotoxicity, no clearly superior method exists and the best mitigation is avoidance of exposure in at-risk patients. In patients who cannot undergo a contrast-enhanced CT, MRI may be an option with a wider range of creatinine acceptance due to the lack of nephrotoxicity of gadolinium agents.
| Renal Function | Guideline |
|---|---|
| Serum Cr <1.4 | Contrast permitted |
| Chronic serum Cr <2 | Contrast permitted |
| Chronicity unknown, serum Cr >1.4 | Calculate eGFR; if >30, then contrast permitted |
| Acute elevation in serum Cr | Contrast should be avoided if possible |
| Patient on dialysis | Contrast may be permitted (allowing preservation of residual renal function is not a goal) Arrangement of dialysis after contrast administration is advised |
| |
In addition to CIN, allergy to iodinated contrast presents a challenge. Premedication for prior mild reactions (hives, itching, and so forth) can be performed with steroids and antihistamines; however, avoidance of contrast in patients with prior severe reactions (laryngeal edema, dyspnea, and shock) is recommended. Although a prior reaction indicates a degree of predisposition/atopia, there is insufficient evidence to support cross-reactivity between CT contrast and MR contrast. Therefore, depending on institutional policy, a contrast MRI examination may be an alternative in patients with prior severe reaction to CT contrast.
MRI
Basics of magnetic resonance
MRIs are created by combining strong magnetic fields, radiofrequency pulses, and weaker magnetic fields (gradients), all of which have an impact on the hydrogen protons within the body that become energized and spin at a resonant frequency. This frequency information is decoded by complex mathematical equations (Fourier transform) to produce images. The brightness and darkness of an image are described as signal intensity, either hyperintense or hypointense, respectively. As part of a routine liver MRI, several sequences are obtained. These give different information about the organs and tumors being imaged. Table 3 shows the routine liver MRI sequences.
| MR Pulse Sequence | Comments | Technical Specifications |
|---|---|---|
| T1-weighted chemical shift (in- and opposed phase, dual-echo gradient-recall echo) |
|
|
| T2-weighted (TSE T2, ssFSE) T2-weighted fat suppressed (inversion recovery, T2 TSE FS) |
| |
| T1-weighted fat suppressed (VIBE, THRIVE, LAVA, GRE) | Provides precontrast baseline signal intensity to help determine enhancement postcontrast | |
| Dynamic postcontrast (VIBE, THRIVE, LAVA, GRE) | Similar dynamic phases to CT (see Table 1 ) | |
| Diffusion-weighted images |
|
Similar to CT, contrast is often used to characterize liver lesions and improve visualization. MR contrast agents consist of gadolinium-containing medium. Gadolinium interacts with the water molecules in the blood to produce T1 shortening (bright signal). A majority of MR contrast agents behave in an extracellular fashion, similar to CT contrast, providing dynamic enhancement information during the late arterial, portal venous, and equilibrium/delayed phases. In addition, there are 2 commonly used hepatobiliary contrast agents: gadobenate dimeglumine (MultiHance, Bracco) and gadoxetic acid (Eovist, Bayer Healthcare Pharmaceuticals, Whippany, NJ, USA). Approximately 4% of gadobenate dimeglumine is excreted in the bile, with peak parenchymal enhancement (hepatobiliary phase timing) occurring at approximately 1 hour after injection. Up to 50% of gadoxetic acid is excreted in the bile, with peak enhancement occurring approximately 20 minutes after injection. The mechanism of uptake in the hepatocytes is thought primarily related to active transport by liver specific multidrug organic anion-transporting polypeptides (OATP1B1 and OATP1B3) on the hepatocyte cell surface. The degree of uptake and diagnostic reliability may be diminished in patients with underlying severe fibrosis, cirrhosis, and cholestasis due to reduced transporter function. Hepatobiliary contrast agents are generally suggested for focal liver lesion characterization and gadoxetic acid has been shown to add value in the setting of metastatic tumor detection. Gadoxetic acid has also shown promise in depicting the ductal anatomy due to its relatively high excretion into the bile. The role of hepatobiliary agents in HCC remains controversial and is discussed in greater depth later.
The main advantages of MRI in liver evaluation hinge on the high diagnostic accuracy, improved contrast resolution, noninvasive imaging of the biliary tree, and lack of ionizing radiation. An additional advantage is the lack of nephrotoxicity of gadolinium contrast agents. The main disadvantage of MRI relates to patient suitability. The most common reasons for nonsuitability are certain contraindicated implanted ferromagnetic devices, claustrophobia, severe ascites, and inability to comply with breath-holding commands. Patients with large-volume ascites should have paracentesis prior to MRI. In addition, for optimal image quality, patients must be able to lie very still and hold their breath for at least 15 to 18 seconds. Motion due to patient discomfort and inability to hold the breath is a common cause of image artifact and may be severe enough to render an examination nondiagnostic.
Nephrogenic systemic fibrosis and MRI contrast agents
Although initially reported as a disease in 1997, nephrogenic systemic fibrosis (NSF) has more recently been linked with gadolinium contrast administration in patients with severe acute or chronic renal insufficiency. The FDA first issued an advisory in 2006 regarding the safety concerns of gadolinium use in renal failure, followed by a black box warning on gadolinium contrast in 2010. NSF is a progressive skin condition in which the skin eventually becomes thickened and hardened and may lead to joint contractures. A vast majority of NSF cases have occurred in patients with a glomerular filtration rate (GFR) less than 15 mL/min in combination with hemodialysis or peritoneal dialysis. No reports of NSF in normal renal function patients exist. The American College of Radiology advises against use of high-risk gadolinium agents in patients with GFR less than 45 mL/min. Most hospitals have institutional policies that emphasize screening for at-risk patients and avoidance of administration of gadolinium in the setting of severe dysfunction. Table 4 discusses the institutional policy at Washington University on gadolinium contrast and renal dysfunction as well as some special considerations for MRI contrast.
| Renal Function | Guideline |
|---|---|
| GFR>30 | Contrast ok |
| GFR <30 | Assess risk benefit for patient to determine whether a viable alternative exists |
| Dialysis (hemodialysis or peritoneal) a | No contrast |
| |
a Some institutions allow for contrast administration to patients on hemodialysis, allowing patients are dialyzed after administration.
PET/Computerized Tomography
PET/CT is an imaging study in which a radioactive tracer, commonly fluorodeoxyglucose F 18 (FDG), is injected intravenously and the radioactivity within local tissue distributions is imaged tomographically and fused with CT images. The CT images provide not only anatomic information but also attenuation correction for the PET data, allowing for accurate quantitative estimates of uptake within tissues of varying densities (soft tissue, fat, and bone). FDG is a glucose analog that distributes to regions of high cellular glucose utilization, such as are seen in malignancies. Glucose metabolism is often up-regulated in inflammatory conditions as well, which can be problematic for differentiating tumor from inflammation. The radiation dose to a patient is a combination of the injected radiopharmaceutical and that obtained from the CT scan. The radiopharmaceutical is typically excreted in the urine; however, there are often physiologically significant levels of uptake within the liver and bowel. The uptake in the liver can be heterogeneous and may make discrimination of focal liver lesions difficult, especially if the lesions are small. An additional challenge related to PET imaging of the liver is the effects of respiratory motion. The PET data are acquired from free-breathing images due to the length of acquisition required to obtain sufficient PET counts and image quality (typically 90–120 seconds per bed position). As a result of the free-breathing acquisition, motion of the diaphragm and liver results in significant loss of resolution and blurring (reducing the intrinsic spatial resolution from 4 mm to closer to 11 mm). The end result is that small liver lesions (less than 1 cm) may not be easily seen.
Imaging liver lesions
Hepatocellular Carcinoma
HCC is the most common primary hepatic malignancy and typically arises in the setting of chronic liver disease. Although controversy exists as to the appropriate combination of imaging and laboratory surveillance for HCC, there is strong support for screening an at-risk population because the early treatment of HCC provides much improved survival. Fig. 3 shows the updated AASLD guidelines for screening and diagnosis of HCC.