There should be histological confirmation of the disease and separation of carcinomas into mucinous and non‐mucinous adenocarcinomas. Goblet cell adenocarcinomas are classified according to the carcinoma scheme. Grading is of particular importance for mucinous tumours. Appendix (C18.1) The ileocolic are the regional lymph nodes (Fig. 162). Notes 1 Tis includes cancer cells confined within the glandular basement membrane (intraepithelial) or lamina propria (intramucosal) with no extension through muscularis mucosae into submucosa. 2 Direct invasion in T4 includes invasion of other intestinal segments by way of the serosa, e.g., invasion of ileum. 3 Tumour that is adherent to other organs or structures, macroscopically, is classified as T4b. However, if no tumour is present in the adhesion, microscopically, the classification should be pT1–3. 4 LAMN with involvement of the subserosa or the serosal surface should be classified as T3 or T4a respectively. Note * Tumour deposits (satellites) are discrete macroscopic or microscopic nodules of cancer in the pericolorectal adipose tissue’s lymph drainage area of a primary carcinoma that are discontinuous from the primary and without histological evidence of residual lymph node or identifiable vascular or neural structures. If a vessel wall is identifiable on H&E, elastic or other stains, it should be classified as venous invasion (V1/2) or lymphatic invasion (L1). Similarly, if neural structures are identifiable, the lesion should be classified as perineural invasion (Pn1). The pT and pN categories correspond to the T and N categories. Note pM0 and pMX are not valid categories.
APPENDIX (ICD‐O‐3 C18.1)
Rules for Classification
Anatomical Site
Regional Lymph Nodes
Carcinoma
TNM Clinical Classification
T – Primary Tumour
TX
Primary tumour cannot be assessed
T0
No evidence of primary tumour
Tis
Carcinoma in situ: intraepithelial or invasion of lamina propria1
Tis (LAMN)
Low‐grade appendiceal mucinous neoplasm confined to the appendix (defined as involvement by acellular mucin or mucinous epithelium that may extend into muscularis propria)
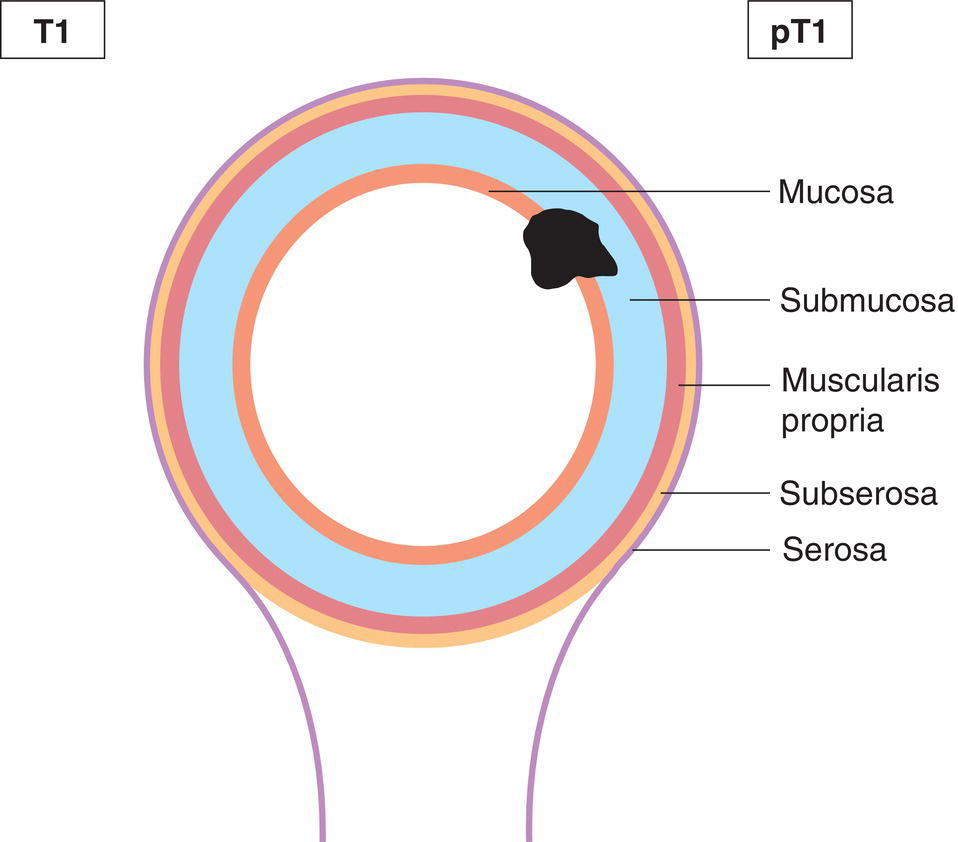
T1
Tumour invades submucosa (Fig. 163)
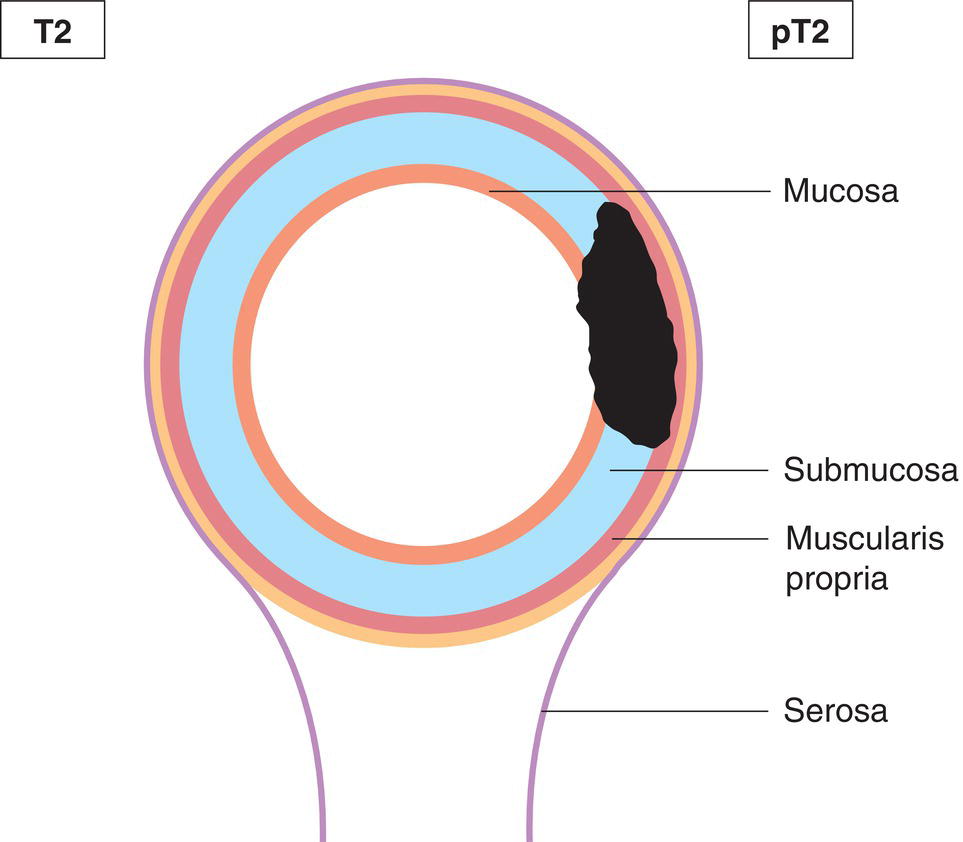
T2
Tumour invades muscularis propria (Fig. 164)
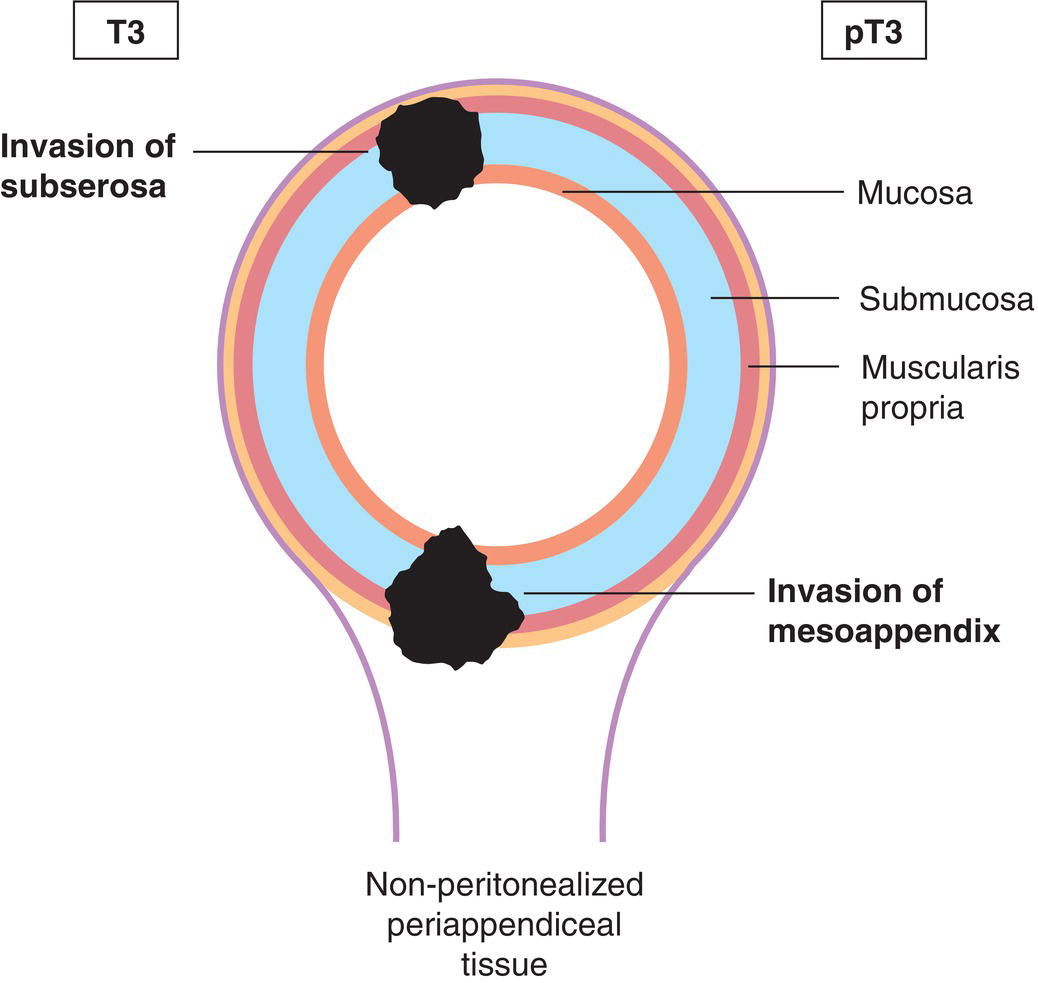
T3
Tumour invades subserosa or mesoappendix (Fig. 165)
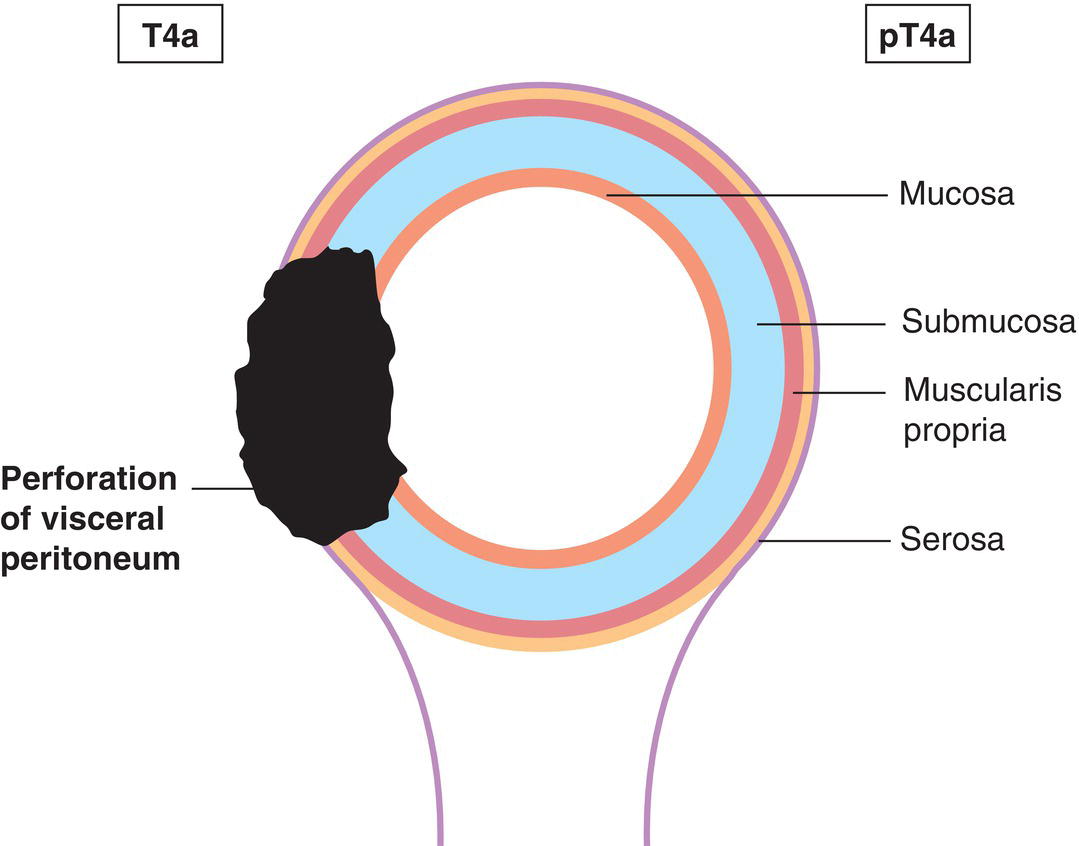
T4
Tumour perforates visceral peritoneum, including mucinous peritoneal tumour within the right lower quadrant and/or directly invades other organs or structures2,3,4 (Figs. 166, 167)
T4a
Tumour perforates visceral peritoneum, including mucinous peritoneal tumour within the right lower quadrant (Fig. 166)
T4b
Tumour directly invades other organs or structures (Figs. 167, 168, 169) 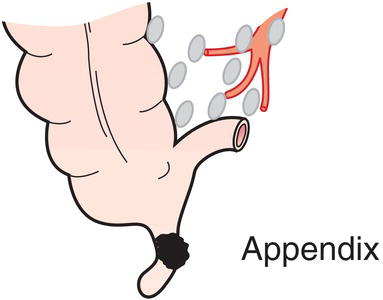
N – Regional Lymph Nodes
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
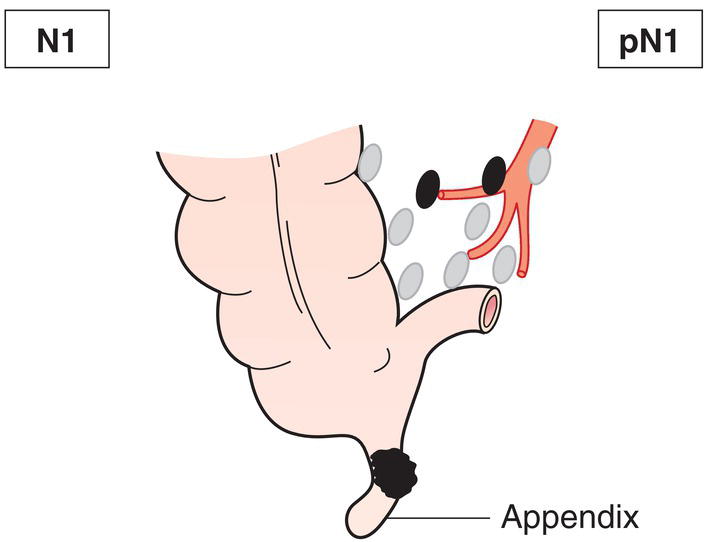
N1
Metastasis in 1 to 3 regional lymph nodes (Fig. 168)
N1a
Metastases in 1 regional lymph node
N1b
Metastases in 2 to 3 regional lymph nodes
N1c
Tumour deposit(s), i.e. satellites,* in the subserosa, or in non‐peritonealized pericolic or perirectal soft tissue without regional lymph node metastasis
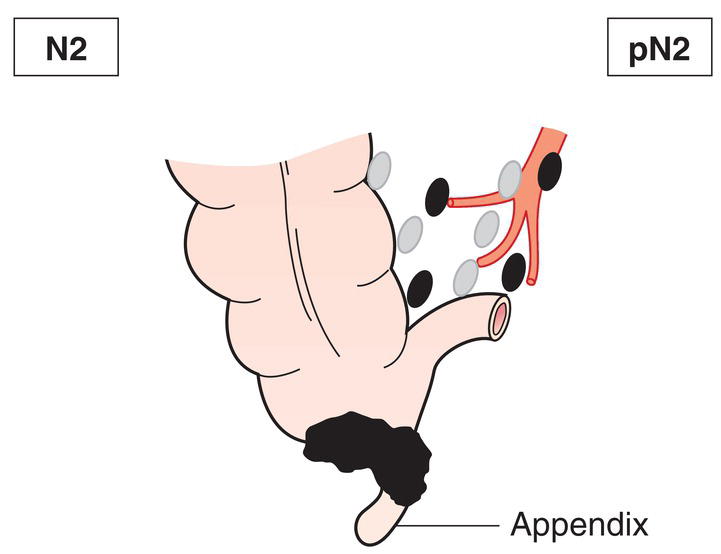
N2
Metastasis in 4 or more regional lymph nodes (Fig. 169)
M – Distant Metastasis
M0
No distant metastasis
M1
Distant metastasis
M1a
Intraperitoneal acellular mucin only
M1bM1c
Intraperitoneal metastasis onlyNon‐peritoneal metastasis
pTNM Pathological Classification
pM1
Distant metastasis microscopically confirmed
pN0
Histological examination of a regional lymphadenectomy specimen will ordinarily include 12 or more lymph nodes. If the lymph nodes are negative, but the number ordinarily examined is not met, classify as pN0. 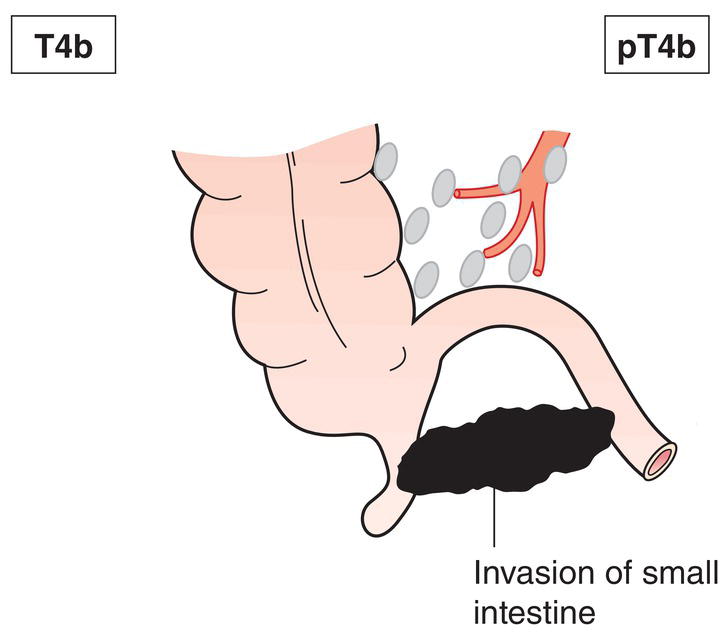
Summary
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree