HYPERTENSION IN THE NON PREGNANT DIABETIC POPULATION
Outside of pregnancy hypertension is more common in diabetic women compared with the background population. The prevalence of hypertension defined as BP greater than 140/90 mmHg was reported as 12% and 22% in non-pregnant women with Type 1 diabetes aged 15–30 and 30–44 years, respectively.1 Hypertension increases in the presence of microalbuminuria or diabetic nephropathy.2 Among women with Type 2 diabetes, the prevalence of hypertension is probably even higher.1
The diagnostic cut-off level for a diagnosis of hypertension in diabetic patients is a matter of debate but a treatment goal of 130/80 mmHg is now widely accepted.3
The development of hypertension in diabetic subjects is often associated with a slightly elevated albumin excretion microalbuminuria or even frank proteinuria. Diabetic nephropathy is characterized by development of proteinuria, hypertension, edema, and decline in kidney function (see chapter 16).
In non-pregnant subjects with Type 1 diabetes, hypertension is closely associated with an increased risk of cardiovascular disease. Reduction of BP with antihypertensive drugs, particularly those affecting the renin angiotensin system, in diabetic patients with microalbuminuria or diabetic nephropathy is of utmost importance to prevent the progression of kidney disease, reduce cardiovascular morbidity, and improve survival. 3–5 Treatment with these drugs is indicated even in normotensive non-pregnant diabetic patients with microalbuminuria, the forerunner of overt diabetic nephropathy.
Table 15.1 Hypertensive disorders in pregnancy.
| Chronic hypertension | BP ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic prior to pregnancy or before 20 weeks of gestation; or hypertension diagnosed for the first time during pregnancy that does not resolve postpartum.1 (However, in diabetic women BP > 135/85 or even BP > 130/80 mmHg may be classified as chronic hypertension in some centers1,7) |
| Gestational hypertension | BP > 140 mmHg systolic or >90mmHg diastolic first detected after 20 weeks of gestation without proteinuria. If increased blood pressure returns to normal by 12 weeks postpartum the diagnosis is retrospectively made as transient hypertension of pregnancy. If it persists, a diagnosis of chronic hypertension applies6 |
| Pre-eclampsia | BP > 140 mmHg systolic or > 90 mmHg diastolic and proteinuria (≥ 1+ on a dipstick or ≥ 300 mg/24 h) after 20 weeks of gestation6 |
| Chronic hypertension with superimposed preeclampsia | In women with hypertension early in pregnancy developing new-onset proteinuria fulfilling the criteria for pre-eclampsia |
| In women with diabetic nephropathy with proteinuria in early pregnancy, development of preeclampisa is defined as above if accompanied by a sudden increase of ≥ 15% in systolic or diastolic blood pressure7 | |
| A sudden 2–3–fold increase in proteinuria and/or thrombocytopenia (platelets < 100 000) and/or an increase in aspartate aminotransferase or alanine aminotransferase above normal levels also indicates pre–eclampsia1 |
BP, blood pressure
HYPERTENSIVE DISORDERS IN PREGNANCY
Hypertension is a very common medical disorder of pregnancy, being reported to complicate one in 10 pregnancies.6 The prevalence is even hig her in diabetic women,1,7 mainly in women with Type 1 or Type 2 diabetes present before pregnancy, but also in women developing gestational diabetes. There are four major hypertensive disorders in pregnancy: (1) chronic hypertension, (2) gestational hypertension, (3) pre-eclampsia, and (4) pre-eclampsia superimposed on hypertension or diabetic nephropathy. Each of these conditions has unique pathophysiologic features that have implications for antihypertensive therapy (Table 15.1). All categories are more common in diabetic than in non-diabetic women.1 The diagnostic criterion for diabetic women follows that of the normal population (≥140/90mmHg), however, as in the non-pregnant diabetic population, lower diagnostic levels for chronic hypertension have been suggested.1,7 In Copenhagen, a diagnostic level of chronic hypertension in pregnancy of 135/85 mm/Hg has been used7 and even lower levels of greater than or equal to 130/80 mmHg for chronic hypertension in diabetic pregnant women are suggested in the 2008 American Diabetes Association (ADA) guidelines.1
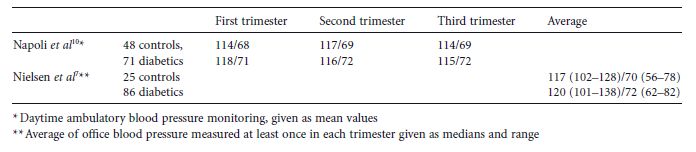
Table 15.2 Blood pressure (mmHg) in normal pregnancy and in women with Type 1 diabetes.
Chronic hypertension, i.e. present before pregnancy, is associated with an increased risk of mid-trimester fetal loss, superimposed pre-eclampsia, preterm birth, intrauterine fetal growth restriction, and neonatal morbidity.8 In addition, women with chronic hypertension are at risk of developing severe hypertension (≥160/110mmHg) and stroke during pregnancy.
Gestational hypertension is the onset of hypertension after 20 weeks of gestation and does not lead to pregnancy complications in mild cases. However, it may progress to pre-eclampsia in a substantial proportion of cases (10 – 50%) or to severe hypertension (≥ 160/110 mmHg) with a comparable risk of severe pregnancy complications as in women with pre-eclampsia.8
Pre-eclampsia presents clinically as development of hypertension later than 20 weeks of gestation accompanied by proteinuria: greater than or equal to 1+ on a sterile urinar y dipstick or ≥ 300 mg/24 h. Pre-eclampsia is associated with a substantial risk of severe maternal and fetal complications, such as placental abruption, cerebral catastrophe, coagulation abnormalities, and even maternal death. Termination of pregnancy is the most effective treatment and, consequently, pre-eclampsia often leads to preterm delivery with all its sequelae. The prevalence (7 – 20%) of preeclampsia is increased in pregnant women with Type 1 diabetes.1 In patients with chronic hypertension, superimposed pre-eclampsia often develops early in pregnancy and with a more severe clinical presentation.
In diabetic women with microalbuminuria or diabetic nephropathy, superimposed pre-eclampsia is also prevalent and often of early onset, leading to preterm delivery.9 The prevalence of pre-eclampsia in Type 1 diabetes is 6 – 10% in women with normal urinary albumin excretion, but is increased to 42% in women with microalbuminuria and 64% in women with diabetic nephropathy.7
Normal blood pressure in diabetes in pregnancy
Knowledge of normal BP is relevant to setting targets for treatment of hypertensive diabetic pregnant women. Even in normotensive normoalbuminuric women, diabetes is associated with a slightly higher BP in pregnancy, but still well within the normal range (Table 15.2).7,10
PRACTICAL ASPECTS OF DETECTING HYPERTENSION IN PREGNANCY
At the first pregnancy visit, BP and urinary albumin excretion should be measured, as well as history of hypertension, microalbuminuria or diabetic nephropathy, and antihypertensive treatment recorded. The patient can thereafter be classified according to presence of hypertension, microalbuminuria or diabetic nephropathy. BP should be recorded at each visit. Home BP measurements might be applicable to women with hypertension in pregnancy, but 24-hour BP monitoring generally has not been useful. Normotensive normoalbuminuric patients should be tested for the presence of proteinuria by dipstix at each visit, while progression of urinary albumin excretion in women with microalbuminuria, hypertension or diabetic nephropathy should be followed at each visit with determinations of the 24-hour urinary albumin excretion or the albumin-to-creatinine ratio in a spot urine sample.
PRINCIPLES FOR TREATMENT OF HYPERTENSION IN PREGNANCY
Mild–to–moderate hypertension
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree