John Potter, Phyo Myint Demographic changes in most Westernized societies have highlighted the increasing number of older and very old (80+ years) adults in the global population, of whom over two thirds will have raised blood pressure (BP) levels. These elevated BP levels cannot be regarded as benign, only reflecting the effects of the natural aging process on the cardiovascular system, because they are associated with significant rates of cardiovascular disease, which remains the single biggest causes of death in this age group. Intervention trials have shown the benefits of BP reduction even in those aged 90+ years in terms of reducing cardiovascular events; this evidence has perhaps swung the pendulum from reluctance to treat hypertension in older adults to active lowering of BP, even in the very old, in more recent years. Following the publication of the Hypertension in the Very Elderly Trial,1 and other important studies involving older adults, many new and relevant guidelines have been published centered on the optimal treatment of the older hypertensive patient. This chapter deals with the epidemiologic and pathophysiologic changes associated with hypertension in older adults, as well as some of the therapeutic changes that have resulted from the more recent studies involving older hypertensive patients, to give a practical guide to diagnosis and management. Cross-sectional and longitudinal studies in industrialized cultures have shown an age-related rise in BP, with increases in systolic BP (SBP) being almost linear up to age 80 years, plateauing thereafter, whereas diastolic BP (DBP) levels plateau earlier, at 50 to 60 years, and then fall.2 These changes herald the important age-related changes that occur in pulse pressure (PP), which rises steeply after the age of 60 years irrespective of SBP levels when young, whereas mean arterial pressure (MAP) shows a much greater increase with age in those with high values in their 30s and 40s and reaches a plateau after the age of 50 to 60 years. Many factors govern these changes, genetic and environmental. For example, Afro-Caribbeans tend to have a greater age-related BP rise than whites, especially in women, and a higher prevalence of hypertension up to the age of 75 years, although this ethnic difference is significantly attenuated after this age.3 Important gender differences in the BP changes with age are also found when comparing the results from cross-sectional and longitudinal studies, with the former showing women to have higher SBP and DBP values than men after 50 years of age. Cohort studies show a different pattern, with SBP increasing to the same degree in both genders, with little difference in age-related values, whereas DBP levels for women are consistently lower than for men, about 5 mm Hg. It is possible that some of these differences in cross-sectional studies are due to selective mortality differences (e.g., death rates being higher in those with higher BP levels), resulting in an underrepresentation of those with initially high BP levels in the older age groups. Lifestyle differences probably influence some of these age-related alterations, little change in BP being seen with advancing years in some non-Western cultures. Hypertension may be defined as the BP threshold at which the benefits of treatment outweigh those of nontreatment, but the actual BP levels and how they are measured for defining hypertension have changed considerably recently (see later). In the United Kingdom, using a threshold of 140/90 mm Hg for hypertension, the Health Survey for England found that 60% of men and 53% of women aged 60 to 69 years were hypertensive, with prevalence rates rising to 72% for men and 86% for women aged 80+ years.4 Despite these high prevalence rates, awareness, treatment, and control rates have significantly improved over the past 2 decades, with control rates increasing from 33% in 1994 to 63% in 2011. There are, however, marked differences in prevalence rates between countries (e.g., in rural India rates ≅ 46% compared to 80% in Venezuela for those aged 65+ years).5 In most studies, these rates are based on just two or three recordings at a single visit and, given the increased BP variability in older adults, the estimates are probably too high; rates based on repeated measurements may be up to 30% less than those quoted.6 SBP tends to increase to a greater extent than the DBP with advancing years, so isolated systolic hypertension (ISH) is the most common form of hypertension in older adults. Prevalence rates for ISH in the BIRNH Study were 9.9% in men and 11.7% in women aged 65 to 74 years, compared with rates for diastolic hypertension (DBP = 95 mm Hg) of 15.8% and 10.6%.7 For those aged 75 to 89 years, ISH rates increased to 15.3% and 17.4% in men and women, whereas diastolic hypertension (DH) fell to 7.7% in men but increased slightly to 11.2% in women. Interestingly, 84% of all female hypertensives in this study were aware of their diagnosis, compared with less than 70% of men, highlighting the need for BP screening in this age group. Other studies using multiple BP recordings made on several visits have found prevalence rates for ISH of 4.2%, combined hypertension (CH) in 3.9%, and isolated DH of 1% in those aged 65 to 84 years.6 Increasing hypertension prevalence rates have been reported in several countries; for example, in the U.S. National Health and Nutrition Examination Survey (NHANES), rates of hypertension in men aged 70+ years increased from 56.6% in 1988 to 1994 to 63.3% in 1999 to 2004 and for women increased from 68.7% to 78.8% over the same time periods.8 However, the Health Survey for England has shown that hypertension prevalence rates between 1994 and 2011were basically unchanged, remaining at around 30% for all age groups combined.4 Reliable hypertension incidence data are relatively scarce, particularly in the very old population. Recent U.S. studies have shown that incidence rates vary markedly with ethnicity, with crude incidence rates/1000 person-years being 118 in blacks aged 65 to 74 years compared to 74 in whites, although no such ethnic differences are seen in older age groups.3 However blacks had a greater awareness and were more likely to be treated for their raised BP levels than whites, although not necessarily with better BP control. Hypertension in older adults is associated with a twofold to fourfold greater risk of a cardiovascular (CV)–related death than for age- and gender-matched normotensives. There has been much discussion as to whether the link between BP and CV morbidity and mortality is linear, U-shaped, or J-shaped, although many of the intervention studies suggesting an increased risk with lower BP levels were of relatively short duration and did not control for potentially confounding variables. The largest meta-analysis of prospective observational studies to date, involving nearly 1 million adults with no previous history of CV disease, has clearly shown a log linear relationship between increasing BP levels and CV mortality, at least up to the age of 89 years. There was no evidence of a J– or U-shaped effect down to SBP levels of 115 mm Hg and DBP values of 75 mm Hg.9 A reduction in SBP of 20 mm Hg would potentially reduce stroke mortality by 74% in those aged 40 to 49 years but only by 33% in those aged 80 to 89 years. However, because the absolute risk of stroke and coronary heart disease (CHD) events is much greater in older adults, a 20-mm Hg lower SBP or 10-mm Hg lower DBP would result in an annual difference in absolute risk that is almost 10 times greater in those aged 80 to 89 years compared with the 50- to 59-year-old group. For the very old, some prospective observational studies have suggested that high BP is not a risk factor for mortality, and low values are more closely associated with excess deaths.10 Little is known about the pattern and factors associated with long-term change (either rise or fall) in BP at a population level, and its impact on important outcomes, including CV incidence, mortality, and cognition, has been less well researched. Cardiovascular events are more closely related to SBP than DBP levels in older adults. In the Copenhagen Heart Study,11 the risk ratio (RR) for stroke due to ISH (SBP = 160 mm Hg; DBP < 90 mm Hg) in men was 2.7, but for diastolic hypertension (DBP = 90 mm Hg, irrespective of SBP) it was 1.7 compared with normotensives. For myocardial infarction, no such difference was seen in the relative risk between ISH and diastolic hypertension. More importantly, borderline ISH (SBP = 140 to 159; DBP < 90 mm Hg) in the Physicians Health Study12 was associated with a 32% increase in CV events and a 56% increase in CV deaths compared to normotensives. If future studies show that treatment of borderline ISH reduces CV risk, this will have enormous implications, because over 20% of those older than 70 years fall into this BP category. The difference between SBP and DBP values (PP) increases greatly after the age of 50 years as a result of arterial wall stiffening with the associated increase in SBP and fall in DBP. In older age groups in the Framingham study,13 coronary heart disease was found to be inversely related to DBP at any given level of SBP, suggesting that higher PP is as important, if not more so, than any other component of BP in predicting CHD risk. Pulse pressure was also a better predictor than SBP, independent of DBP levels, for congestive heart failure (CHF); for each 10-mm Hg increase in pulse pressure, there was a 14% increased risk of CHF compared with a 9% increase for the same change in SBP. However, for stroke, mean arterial pressure has been found, in some studies at least, to be a better predictor than SBP or PP. In the Systolic Hypertension in the Elderly Programme,14 a 10-mm Hg increase in PP was associated with an RR of stroke of 1.11 (1.01 to 1.22) compared with 1.20 (1.02 to 1.42) for a similar MAP rise, suggesting that in older adults, CHD events are more closely related to pulsatile load than steady-state components of BP. Although much attention has previously focused on actual BP levels and CV risk, new data have highlighted the potential role of BP variability as an additional risk factor. Studies have shown that increasing visit to visit SBP variability (a feature of increasing age), as well as maximum SBP values at each visit, are associated with a greater CV risk, in particular for stroke and cognitive decline, compared to average BP values; however, this has not been found in all studies in older adults, particularly for mortality.15,16 It has also been suggested that the reason some antihypertensive agents (e.g., calcium channels blockers) appear to reduce CV events more effectively in older adults than other agents (e.g., β-blockers) for a similar reduction in BP levels is that they reduce BP variability and/or or central aortic BP more, although this remains to be proven. Masked hypertension (MHT—normal office BP but elevated home and ambulatory BP levels) has also been identified as another element of the BP spectrum that is important in predicting CV events. It is common (up to 40% of normotensive older adults have MHT) and is particularly common in older men, the 80+ age group, and those with diabetes, but is difficult to recognize because it is impossible to perform self-ambulatory BP measurement in all older adults. Studies have shown that it is not a benign condition, increasing the risk of CV events compared to normotensives, with a hazard ratio of 1.55 compared to 2.1 for those with sustained hypertension.17 White coat hypertension (WCH—high clinical but normal home and ambulatory BP levels) is also common. In the HYVET trial, 50% of participants had WCH18 but it appears to be a more benign condition, having a similar or only marginally raised CV risk compared to normotensives. As yet, however, there is no clear evidence that treating WCH or MHT is of benefit at any age. MAP is determined by cardiac output and peripheral vascular resistance (PVR) and is the steady-state component of blood pressure. The dynamic component, PP, is the variation around the mean state and is influenced by large artery stiffness, early pulse wave reflection, left ventricular ejection, and heart rate. A rise in PVR and large artery stiffness will increase the systolic BP component, whereas a decrease in PVR or increase in large artery stiffness will result in a fall in diastolic BP, with the latter being the dominant change in older hypertensives. The main cardiovascular pathophysiologic changes associated with aging are arterial dilation and a decrease in large artery compliance and increased arterial stiffness, especially in the aorta, because of the loss of elastic fibers in the vessel wall and a concomitant increase in collagen. Arterial stiffening leads to enhanced pulse wave velocity (PWV) and early reflected waves augmenting the late systolic aortic pressure wave, resulting in an SBP increase and DBP fall (the underlying findings in isolated systolic hypertension), although the BP changes with age do not generally parallel those of PWV. The rise in mean aortic pressure is augmented by the rise in PVR, seen particularly in older women, and enhanced by impaired endothelial release of nitric oxide, especially in older hypertensives. The increase in systolic load puts excess mechanical strain on the left ventricle, leading to concentric wall thickening. Because coronary artery perfusion is primarily dependent on the diastolic pressure, any reduction in DBP can have adverse effects on coronary artery perfusion, especially because left ventricular myocardial demands are increased in hypertension. The other main features associated with hypertension in older adults are a reduction in heart rate, cardiac output, intravascular volume, glomerular filtration rate, and cardiac baroreceptor sensitivity (BRS), although cerebral autoregulation is unimpaired with normal aging and hypertension.19,20 This decrease in cardiac BRS accounts for the increased BP variability found in older hypertensives and plays a role in the increased susceptibility to postural hypotension. Both renal plasma flow and plasma renin activity (PRA) levels decrease with age, with the fall in PRA being more marked in older adult hypertensives than in normotensives. Plasma noradrenaline (norepinephrine) levels increase with age and are associated with a decrease in β-adrenoreceptor sensitivity. Primary prevention of CV events is based on the assessment and treatment of classical risk factors, and hypertension should not be considered in isolation, irrespective of patient age. However, it is increasingly clear that the predictive value of the usual risk factors alters with age and therefore standard risk charts, as used in many guidelines, cannot be used in the very old who, because of their age, are already at high risk. The management of dyslipidemia in older adults, especially in those 75 years and older, has been poorly studied but is important, especially because increases in lipid levels and BP are often closely related. Serum total cholesterol (TC) levels increase with age and remain a significant independent predictor for CHD in men. The effect in women is less clear because the numbers of women studied have been too small to draw firm conclusions. The SHEP study14 found that TC and low-density lipoprotein (LDL) cholesterol levels remained significant indicators of risk in both genders, such that a 1-mmol/L increase in TC was associated with a 30% to 35% higher CHD event rate. The Prospective Studies Collaboration meta-analysis of prospective observational studies of more than 900,000 adults has shown increasing TC levels to be a risk factor for CV mortality, even in the very old. However, although the risk is attenuated with age, such that a 1-mmol/L lower TC was linked to a significant reduction in the hazard ratio (HR) for CHD in those aged 50 to 59 years to 0.57, compared with 0.85 in the 80- to 89-year-old group.21 This effect was greater in men than women in the older age groups, but was present in both up to 90 years of age. However, for stroke, the link with TC was not as strong as for CHD. For a similar TC reduction, there was a significant lowering of the HR for stroke by 9% in 50- to 59-year-olds compared with a nonsignificant 5% increase in the HR in those aged 80 to 89 years. For CHD, but not stroke, the ratio of TC to high-density lipoprotein (HDL) cholesterol was a better predictor than TC alone, but the predictive power fell with age. A 1.33 lower ratio was related to a 31% decrease in CHD mortality in the 70- to 89-year-old group compared with a 44% reduction in 40- to 59-year-olds. For stroke in those aged 70 to 89 years, and with an SBP higher than 145 mm Hg, TC was negatively correlated with hemorrhagic and total stroke mortality. Up to 10% of older adults with hypertension will have impaired glucose tolerance, and diabetes doubles the risk of developing CHD and stroke in those aged 65 to 94 years. Like total cholesterol, however, its impact on CV events decreases with age: women remain slightly more at risk than men, although the absolute risk from diabetes is greater in older adults than in younger adults. Increasing body mass index (BMI) is associated with a BP increase, but the risk of obesity-related hypertension declines with age compared to those of normal weight; the risk of hypertension is increased threefold in obese 20- to 45-year-olds compared to a 1.5 increase in 65- to 94-year-olds. For each unit of BMI increase (kg/m2), SBP can be expected to increase by 1.2 mm Hg and DBP by 0.7 mm Hg. Interestingly, for older hypertensive men, the CV relative risk increases from 1.8 to 2.9 between the lowest and highest tertiles of BMI, whereas the reverse is true for women. Even so, hypertension still more than doubles the risk of developing CV disease in both genders. In the European Working Party on Hypertension in the Elderly (EWPHE) study,22 those with the lowest total mortality and CV terminating events were found in the moderately obese group with a BMI of 28 to 29 kg/m2, whereas those with a BMI of 26 to 27 kg/m2 had the lowest cardiovascular mortality. Truncal obesity (reflected in an increased waist- to-hip ratio) is more strongly related to hypertension and is a better predictor for coronary heart disease and stroke than BMI alone. Adiposity tends to decrease in those 75 years and older, and the CV risk associated with increasing BMI, waist circumference, or waist-to-hip ratio is three to four times less in those 70 years and older compared to 40- to 59-year-olds.23 Although the number of smokers decreases with age, smoking remains a significant risk factor for CV mortality in older adults (RR for men is 2.0 and 1.6 for women). The stroke risk among older hypertensive smokers is five times that of normotensives but 20 times that of normotensive nonsmokers. The benefits of stopping smoking in terms of reducing CHD and stroke mortality are still present, even in those 70 years and older, with the excess risk of mortality declining within 1 to 5 years of quitting. Older smokers should therefore be encouraged to stop. Encouragingly, hypertensive ex-smokers of less than 20 cigarettes/day have, after only a few years of quitting, a similar CV risk to that of hypertensive nonsmokers. In patients with atrial fibrillation, hypertension doubles the stroke risk compared with normotensives. Electrocardiographically diagnosed left ventricular hypertrophy (LVH) increases with age, with reported prevalence rates of 6% in men and 5% in women aged 65 to 74 years, compared with 9.4% and 10.8%, respectively, in those older than 85 years. LVH has a significant effect on CV risk. Its presence in those aged 65 to 94 years nearly triples the risk for men and quadruples that in women, but this effect is less than that seen in younger age groups with a similar BP. Increasing alcohol consumption is associated with a rise in BP, although the relationship is not linear in most epidemiologic studies, with the lowest incidence of hypertension being seen in those consuming about five to ten units of alcohol per week. Large falls in BP (19/10 mm Hg) have been recorded with abstention in those aged 70 to 74 years who had a long history of heavy alcohol intake. Excessive alcohol intake has been directly related to stroke risk; whether this is due to its direct pressor effect or to some other mechanisms, such as increased risk of atrial fibrillation, is unclear. Because there appears to be a mild protective effect of a small amount of alcohol in older adults, there is no reason to advise strict abstinence. The relationship between dietary sodium intake and hypertension strengthens with age. For a 100-mmol/day increase, mean BP rises by 5 mm Hg in those aged 20 years but this more than doubles in those 60 to 69 years. Conversely, increasing potassium intake by 60 mmol/day reduces BP in older adults by as much as 10/6 mm Hg. Increasing potassium dietary intake may also reduce stroke risk independently of its hypotensive effect. The average daily potassium intake in older adults in the United Kingdom is about 60 to 70 mmol. This could be raised to over 100 mmol simply by increasing the consumption of vegetables and fruit. Even mild to moderate physical exercise, such as walking for 30 minutes three to four times a week, has a hypotensive effect and reduces stroke risk, even in older age groups, and has other beneficial effects (e.g., reducing the risk of falls). Whether these effects are mediated solely through BP lowering or are a result of other mechanisms, such as exercise-induced decreases in fibrinogen levels or an increase in HDL cholesterol levels, is unknown. Hypertension remains the major treatable risk factor for stroke, although the attributable risk for increasing BP levels decreases with age. For a 10-mm Hg increase in usual DBP, the risk of stroke is almost doubled. A reduction of 9/5 mm Hg can be expected to produce about a 30% decrease in stroke incidence, whereas a fall of 18/10 mm Hg halves the risk; these expectations are irrespective of baseline BP levels. The relative risk of cerebral infarction varies, depending on the hypertension type in older age groups.24 ISH is a bigger risk factor (RR, 2.3) than combined systolic and diastolic hypertension (RR, 1.5) compared to normotensives. The population-attributable risk for stroke in those aged 70 to 79 years with ISH is about 21% for women and 17% for men, whereas for those aged 50 to 59 years, the figures are 5% for women and 4% for men. Although the relative risk of stroke from raised BP decreases with age, this is not because hypertension per se loses its effect as a risk factor, but that more strokes occur in those with normal blood pressure. Intracerebral hemorrhage is also closely related to hypertension; the relative risk varies from 2.0 to 9.0 in different studies, being greater for combined hypertension than ISH, particularly in younger patients. Deep white matter lesions (leukoaraiosis) in asymptomatic hypertensive older adult patients are frequently found on magnetic resonance scanning. Whether these lesions account for the age-related cognitive impairment seen with hypertension that has been reported in many studies is unknown. It is also uncertain whether they increase the risk of subsequent cerebral infarction or hemorrhage. ISH, in particular, is associated with subcortical lesions, and good BP control appears to have a protective effect. Large diurnal falls in BP are associated with silent subcortical white matter lesions and lacunar infarcts, but these are also found in those who have marked nocturnal rises in BP. The influence of blood pressure on cognitive decline and psychomotor function, over and above its association with vascular dementia, has been widely debated. Some studies have shown no such relationship, whereas others have reported a strong positive correlation with vascular and Alzheimer-type dementia. Studies have suggested that increasing BP levels in midlife are a risk factor for cognitive impairment and dementia in old age, but that there is an inverse correlation between BP measured in old age and dementia in cross-sectional studies. The results of longitudinal studies of BP and cognition in later life are inconsistent, as are those for BP and dementia, although most suggest that a low BP is common in those with severe cognitive impairment.25 Treating hypertension, even with small decreases in BP, is associated with improvements in MMSE scores and immediate and delayed memory scores, as well as significantly reducing the risk of dementia in some but not all studies.26,27 In a recent systematic review of placebo-controlled trials of BP reduction in older adults with dementia, Beishon and colleagues28 showed that there was no clear evidence for benefit (or harm) on cognition or other CV outcomes from antihypertensive use. The pathogenesis of hypertension-related cognitive impairment is unclear but could be linked to a decrease in cerebral blood flow with increasing BP levels and alterations in cerebral metabolism, beyond the changes associated with leukoaraiosis. The Scottish Birth Cohorts data have suggested that the negative relationship between white matter hyperintensities and late-life intelligence is linear and increases with age and hypertension.29 The relationship between CHD and hypertension is discussed in a later chapter. Hypertension accelerates the development of coronary artery atheroma via many mechanisms, particularly in association with metabolic abnormalities, as in the insulin resistance syndrome. Increased blood glucose and insulin levels, changes in total cholesterol, HDL, and LDL levels, and endothelial dysfunction result in impaired endothelial-dependent relaxation and increased leukocyte adherence, smooth muscle proliferation, intimal macrophage accumulation, fibrosis, and arterial medial wall thickening. These changes, along with increased vascular oxidative stress and free radical production, result in inflammatory changes in the arterial wall, monocyte migration into the intima, and plaque formation. Accurate measurement of BP levels in older adults is of paramount importance and, despite posing particular problems, it is essential if patients are not to receive unnecessary or inadequate treatment. Minute to minute BP variations occur with respiratory and vasomotor changes, whereas during the 24-hour period, fluctuations are related to mental and physical activity, sleep, and postprandial changes. Seasonal variations are also seen, with BP levels being higher during the winter months. Clinically important differences in BP are frequently found between individual readings at a single visit and between visits. Large falls in BP with repeated measurements in older adult hypertensives have been demonstrated in nearly every placebo-controlled interventional trial, with the effect increasing with age and amounting to as much as a 10/5 mm Hg decrease. The tendency for BP levels to decrease with time is related in part to regression to the mean and familiarity with the procedure of BP measurement. Guidelines recommend that in uncomplicated cases, an average of two readings (although more will be required in certain cases in which variability is high, as in atrial fibrillation [AF]) be taken with the patient sitting in a quiet relaxed atmosphere on at least two separate occasions, usually during the initial assessment period. It is particularly important to measure BP levels after standing to assess postural BP change in view of the frequency of orthostatic hypotension in this age group and to use standing values if a significant postural BP is found (e.g., >20/10 mm Hg, or the patient is symptomatic). Mercury sphygmomanometers are being phased out and replaced by semiautomatic devices, but it is important to check the accuracy of any device used and ensure that it has been properly validated in older adults. A list of validated BP measuring devices for use in younger persons and older adults is constantly updated on the British Hypertension Society website (www.bhsoc.org). Cuff size is important, because undercuffing gives falsely high BP values. The cuff width should equal two thirds of the distance between the axilla and antecubital fossa and, when the bladder is placed over the brachial artery, it should cover at least 80% of the arm’s circumference, which should be kept supported at heart level. Clinicians should have standard and large cuffs available and ensure that they are used appropriately. Measurement should be taken in both arms initially because more than 10% of older adults have at least a 10-mm Hg difference between arms. The arm with the highest reading should be used for subsequent measurements. Patients should sit quietly, legs not crossed, and be relaxed, and all measurements should be taken at least 2 hours after a meal to ensure that a falsely low level is not recorded due to postprandial decrease. All older adults should have their BP measured every 5 years if untreated, up to age 80 years at least, and in those with high-normal BP (135 to 139 mm Hg and 85 to 89 mm Hg), it should be reassessed annually. Cuff measurements tend to underestimate intraarterial levels of SBP by up to 5 to 10 mm Hg and to overestimate DBP by about 5 to 15 mm Hg. The term pseudohypertension refers to falsely high noninvasive recordings caused by arterial rigidity. The prevalence of this condition in an unselected older adult population is probably very low, about 1% to 2%, but unfortunately there is no accurate clinical method of easily predicting the condition. NICE guidelines30 have highlighted the role of ambulatory BP monitoring (ABPM) or self-BP monitoring (SBPM) in the assessment and management of older adults with hypertension; in the United Kingdom, at least routine use of ABPM or SBPM is needed to confirm the diagnosis of hypertension in those with repeatedly raised clinical values with mild hypertension (140 to 159 mm Hg; 90 to 99 mm Hg). Both forms of monitoring reduce the variability and alerting response to measurement, so that 75% of older adult hypertensives will have lower ABPM and SBPM values than clinical values. For daytime ABPM, this is about 10 to 15/5 mm Hg, with the difference increasing with age. It is suggested that for ABPM, three readings/hour are taken during the daytime (minimum, 14 readings) and hourly readings at night (11 PM to 7 AM). The value of other information that the 24-hour ABPM profile can provide, such as day-night differences, is unknown. For SBPM, there should be two readings in the morning before medication and two readings in the evening for 7 days, and the mean of all 28 readings calculated, although some authorities remove the first day’s values. Both ABPM and SBPM can be used to diagnose WCH, MHT, postural and postprandial hypotension and truly resistant hypertension in older adults. SBPM, rather than ABPM, has also been used to assess BP control on treatment, although the measuring period is reduced to 3 to 4 days. One common feature of hypertension in younger and older adults alike is that it is very often asymptomatic. Complaints often attributed to increased BP levels, such as headache, are unrelated in most cases. The history and examination should include assessment for the presence of important CV risk factors (e.g., diabetes) and for symptoms and signs of secondary causes of hypertension. Other important factors to be considered are the presence of confusion, urinary incontinence, decreased mobility, and other medication use (for possible drug interactions, which will affect the need for and type of antihypertensive agent), all of which will influence treatment decisions. The examination should focus on evidence of target organ damage, including peripheral pulses and bruits (renal or carotid) and cardiac murmurs. Ophthalmoscopy is used for possible malignant phase hypertension (a condition seen in older adults) and diabetic changes, and a neurologic examination is used for signs of cerebrovascular disease and vascular dementia. Initial investigations should include height, weight, blood samples for renal function, lipid profile, glucose and HbA1c level estimations, 12-lead electrocardiogram (to exclude ischemic change, dysrhythmias, and LVH), and urine dipstick test for protein and blood. A chest x-ray is of doubtful benefit, except for those who may have heart failure or pulmonary disease, and echocardiography is rarely needed. Renal artery stenosis is the only major secondary cause of hypertension in this age group and should be considered if there is a sudden onset or rapid progression of hypertension and BP control suddenly becomes difficult, particularly in those at greater risk of atherosclerotic renal artery stenosis (e.g., diabetics, smokers, and those with peripheral vascular disease). It should also be suspected in those who develop malignant phase hypertension and there is rapid deterioration of renal function, particularly after starting angiotensin-converting enzyme (ACE) inhibitors, and in those who develop sudden onset pulmonary edema for no other obvious cause.
Hypertension
Introduction
Epidemiology
Prevalence and Incidence
Blood Pressure and Risk
Systolic Blood Pressure, Diastolic Blood Pressure, Pulse Pressure, and Risk
Blood Pressure Variability, Masked Hypertension, White Coat Hypertension, and Risk
Pathogenesis
Other Cardiovascular Risk Factors
Lipid Abnormalities
Diabetes Mellitus
Body Mass Index
Smoking
Atrial Fibrillation and Left Ventricular Hypertrophy
Alcohol
Diet and Physical Exercise
Complications of Hypertension
Stroke
Blood Pressure and Asymptomatic Cerebrovascular Disease
Cognitive Impairment
Cardiac Disease
Diagnosis and Evaluation
General Issues
Measuring Blood Pressure
Ambulatory and Self-Monitoring Blood Pressure
Clinical Assessment and Investigations
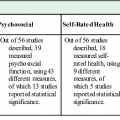
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hypertension
42