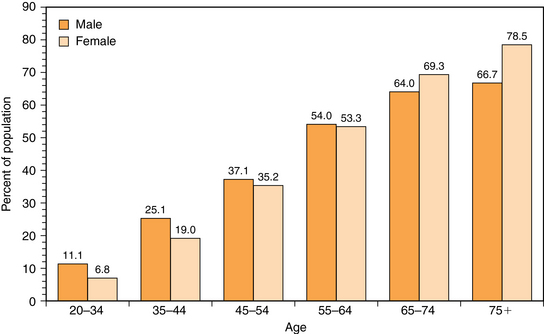
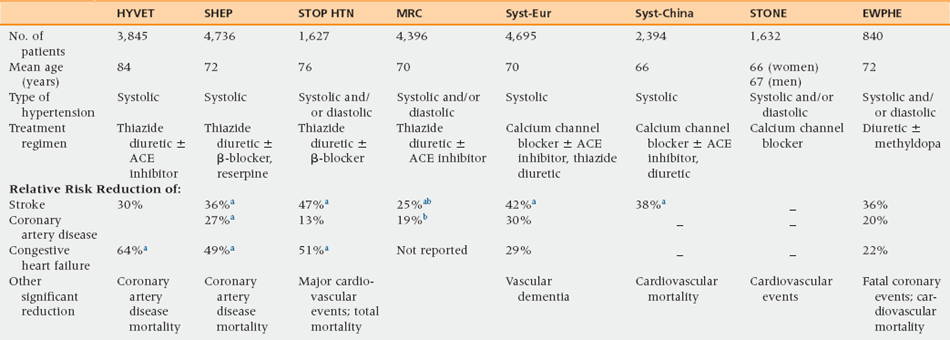
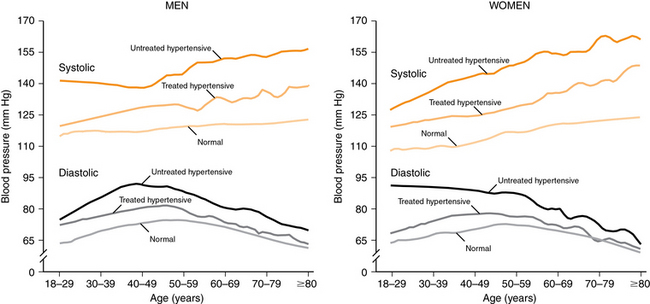
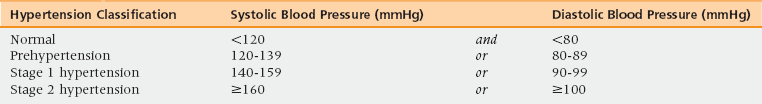
36 Upon completion of this chapter, the reader will be able to: • Define hypertension and its pathophysiologic impact on the cardiovascular system. • Discuss the evidence that treating hypertension is beneficial to the elderly. • Discuss the different types of hypertension. • Discuss the treatment approach, including adjusting therapy in specific clinical conditions common in older people. Hypertension is one of the most common medical conditions in the geriatric population. The percentage of adults with hypertension rises steadily and progressively as people age (Figure 36-1).1 Data on postmenopausal women in the Women’s Health Initiative (WHI) study identified prevalence rates of 27% for women 50 to 59 years of age, 41% for women 60 to 69 years of age, and 53% for women 70 to 79 years of age.2 Figure 36-1 Prevalence of high blood pressure in adults age 20 and older by age and sex. (Source: Roger VL, Go AS, Lloyd-Jones DM, et al; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics 2012 update: A report from the American Heart Association. Circulation 2012;125(1):188-97. doi:10.1161/CIR.0b013e31823ac046. Available at http://circ.ahajournals.org/content/125/1/e2.full.pdf+html.) Compared with whites, blacks of all ages are more likely to have hypertension, a trend that continues as people age.3 Mexican Americans generally have hypertension rates that are lower than those of both whites and blacks.4 Asian Americans are a diverse group, but generally their rates of hypertension are about the same as those of whites, or a little lower, and their risk of death from cardiovascular disease is 50% lower than that of whites.5 The main complication of hypertension in Asian Americans is stroke, whereas in white people it is coronary heart disease.6 Black individuals have the highest rate of hypertension-related mortality.7 Population data consistently show that people with hypertension have a higher rate of all cardiovascular events including myocardial infarctions, stroke, peripheral arterial disease, and heart failure, and that risk of cardiovascular disease associated with hypertension increases markedly with age.8 Among people 80 years of age or older, major cardiovascular events occur in 9.5% of those with normal blood pressure, 19.8% of those with prehypertension, 20.3% of those with stage 1 hypertension, and 24.7% of those with stage 2 hypertension. Hypertension is also linked to functional issues that affect quality of life such as impotence,9 renal function,10 and vascular dementia.11 Whether hypertension increases the risk of Alzheimer’s disease is not clear,12 though cognitive impairment in late life is often a mixture of Alzheimer’s disease and microvascular brain damage, the latter of which is worsened by hypertension. These adverse outcomes lead to increased death rates. In 2008 hypertension was the primary or contributing cause of death for almost 350,000 Americans.1 The death rate associated with hypertension increased 20.2% from 1998 to 2008, and the actual number of deaths rose 49.7%, reflecting increasing numbers of older Americans and their higher prevalence of hypertension. Despite the prevalence of hypertension and evidence of its serious impact on health and mortality, the rate of successful treatment remains low in all ages. Among persons older than 80, only 38% of men and 23% of women have blood pressures that meet targets set by the National High Blood Pressure Education Program’s clinical guidelines.8 Only 29% of older hypertensive women (70 to 79 years of age) in the WHI study had blood pressures within the goal range compared to 41% and 37% of those 50 to 59 and 60 to 69 years of age, respectively.2 The good news is that the percentage of hypertensive adults of the three major race and ethnic groups (non-Hispanic white, non-Hispanic black, and Mexican American) who achieved blood pressure control has steadily increased over recent years as has that of adults age 60 or older.13 The benefits of treating hypertension in older individuals were established in the 1990s when large trials showed that treatment significantly lowered the rate of strokes and cardiovascular disease by 30% to 40% (Table 36-1).14–20 These trials firmly established the benefits for individuals in their 60s and 70s, but concern remained regarding treatment in individuals over age 80 until the Hypertension in the Very Elderly Trial (HYVET) was published in 2008.21 In this older age group, treatment was associated with a 39% reduction in the rate of death by stroke, 23% reduction in rate of death from cardiovascular diseases, 64% reduction in rate of heart failure, and 21% reduction in the rate of death by any cause. TABLE 36-1 Large Randomized, Blinded, Placebo-Controlled Trials of Pharmacologic Hypertension Treatment in the Elderly EWPHE, European Working Party on High Blood Pressure in the Elderly20; HYVET, Hypertension in the Very Elderly Trial21; MRC, Medical Research Council16; SHEP, Systolic Hypertension in the Elderly Program14; STONE, Shanghai Trial of Nifedipine in the Elderly19; STOP-HTN, Swedish Trial in Old Patients with Hypertension15; Syst-China, Systolic Hypertension in China Trial18; Syst-Eur, Systolic Hypertension in Europe Trial17. aStatistically significantly at p < 0.05. bThis reduction was noted only in the thiazide arm. Adapted from Harvey P, Woodward M. Management of hypertension in older people. Aust J Hosp Pharm 2011;31:212-9. Effective treatment of hypertension in older individuals requires an understanding of the pathophysiology that leads to increased blood pressure. Some of these changes occur with normal aging but most are heavily influenced by lifestyle factors. Arterial blood pressure consists of a forward wave generated by the heart and reflective waves returning to the heart from peripheral sites. In young people, the artery is distensible so the pressure wave travels slowly and is reflected back in diastole. Aging is associated with a progressive increase in stiffness of the large vessels.22 With this arterial stiffening, the waves move faster and reflect back to the proximal aorta during systole, augmenting the systolic pressure and lowering the diastolic pressure. Whereas systolic hypertension is associated with an increase in large vessel resistance, diastolic hypertension is associated with an increase in resistance of small peripheral vessels, which hypertension further compounds because the resultant vascular hypertrophy can lead to high resistance and even closure of small vessels.23 Before age 50, most people with hypertension have elevated diastolic hypertension, but as people age the systolic pressure continues to rise and diastolic pressure tends to fall, causing isolated systolic hypertension to be the predominant problem (Figure 36-2).24 These changes lead to a widening pulse pressure (the difference between systolic and diastolic blood pressure) as people age. Framingham data indicate that with increasing age, pulse pressure becomes a better predictor of heart disease than either systolic or diastolic blood pressure.25,26 Figure 36-2 Mean systolic and diastolic pressure for men and women, by age and hypertension status. (Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health and Nutrition Examination Survey, 2001-2008.) With age, blood vessels become less responsive to the vasodilatory effects of β-adrenergic stimulation,27 changes that also contribute to hypertension. Plasma renin activity declines with age, probably because of age-associated nephrosclerosis, and plays less of a critical role in hypertension than the previously described vascular changes.28,29 The decline in the aldosterone level leads to a greater risk of hyperkalemia in older individuals, especially when associated with the overall age-associated decline in renal function. Hypertension is defined as an average blood pressure of 140/90 mmHg or higher, based on at least three readings taken on three separate occasions. Table 36-2 describes blood pressure classifications per the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).30 The JNC is convened by the National Heart, Lung, and Blood Institute and issues the most widely accepted definitions, guidelines, and recommendations in the United States. The most recent report (JNC 7) was released in 2003 and the next report (JNC 8) is in development. TABLE 36-2 Classification of Hypertension Source: Chobanian A, Bakris G, Black H, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. JAMA 2003;289:2560-72. The vast majority of people with high blood pressure have essential hypertension, which is defined as a rise in blood pressure of unknown cause. It is likely the result of an interaction between environmental and genetic factors and tends to coexist with other cardiovascular risk factors such as aging, being overweight, insulin resistance, diabetes, and hyperlipidemia.31 The term essential dates back to the time when it was thought that an increase in blood pressure was a necessary and appropriate response to guarantee adequate perfusion of organs. Hypertension resulting from an identifiable secondary cause is uncommon in elderly individuals but can be considered if there is a sudden rise in blood pressure or a lack of response to three-drug therapy. Probably the most common cause of secondary hypertension in older people is renal disease, although it is often hard to tell if the renal disease is causing the hypertension or vice versa. Renal artery stenosis caused by atherosclerotic disease should be suspected if there is an acute decline in renal function (a rise in serum creatinine of greater than or equal to 0.5 to 1 mg/dL) after starting an angiotension-converting enzyme inhibitor (ACE-I) or angiotension receptor blocker (ARB).30 The renal arteries can be evaluated with computer tomography angiography, magnetic resonance imaging, or ultrasound. However, medical management is as effective as revascularization with similar rates of blood pressure control and cardiovascular deaths and without the risks associated with surgery.32 Thus, diagnosing renal artery stenosis may be of little value in most elderly patients. In rare cases, peripheral arteries may be so stiff and rigid that measuring blood pressure with the arm cuff may lead to an overestimate of the arterial pressure because of incomplete compression of the brachial artery.33 This should be considered in patients whose hypertension does not respond to treatment or who have postural symptoms with treatment. Patients with systolic blood pressure greater than 179 mmHg or a diastolic blood pressure greater than 109 mmHg are at especially high risk of cardiovascular disease and therefore need rapid treatment. These situations are classified as hypertensive urgencies in the absence of acute end-organ damage and as hypertensive emergencies if there is evidence of end-organ damage, such as chest pain, shortness of breath, headache, visual changes, altered mental status, or acute renal failure.30,34 The distinction guides therapy: patients with hypertensive urgency should have blood pressure reduced within 24 to 48 hours and can be treated with oral medications in the outpatient setting, whereas patients with a hypertensive emergency require parenteral drug treatment, usually in a hospital or emergency room setting. A diagnosis of hypertension should be based on at least three different blood pressure readings taken on at least three separate occasions. The principles of blood pressure measurement have changed little since Korotkoff introduced the procedure 100 years ago.31 Mercury sphygmomanometers remain the gold standard but their use is being phased out in many countries because of environmental and health concerns. Aneroid and electronic devices do not use mercury but still report values in millimeters of mercury (mmHg) and are commonly used for safety and convenience. Aneroid sphygmomanometers use auscultation and a dial and require regular calibration to maintain accuracy. Electronic, or digital, devices are widely used and base readings on oscillometric measurements with the device placed at the upper arm or wrist. They do not require auscultation so can be used in noisy environments but may not be accurate in patients with arrhythmias. An up-to-date evidenced-based assessment of specific blood pressure measuring devices is available online at www.dableducational.org. Inappropriately low systolic blood pressure readings in older individuals can occur because of an ausculatory gap, which is the interval of pressure where the Korotkoff sounds that indicate systolic pressure fade away and reappear at a lower pressure point. This gap is related to arterial stiffness and is associated with an increased risk of cardiovascular disease, especially carotid atherosclerosis.35 The true systolic pressure can be obtained by palpating the radial artery pulse, which is recommended whenever a manual blood pressure is taken and is usually around 10 mmHg lower than the pressure heard with auscultation; or, the gap can be avoided by making sure the blood pressure cuff is always inflated to about 30 mmHg higher than that needed to occlude the brachial artery. Office measurement of blood pressure may not accurately reflect a patient’s baseline blood pressure. The blood pressure in the office may be elevated because of patient anxiety (“white coat hypertension”), a phenomenon that is thought to be even more common in the elderly. Conversely, office blood pressure measurement may systematically fail to identify patients with blood pressures that are usually higher than that measured in the office because of a masking effect, which can only be detected with out-of-office readings.36 For accurate diagnosis and monitoring, it is reasonable for nearly all patients to obtain out-of-office blood pressure measurements.37 This can be done by 24-hour ambulatory blood pressure monitoring or intermittent blood pressure monitoring with a validated oscillatory device, the latter being easier and just as reliable.
Hypertension
Prevalence and impact
Adverse outcomes
Low rates of successful treatment
Rationale for treatment
Risk factors and pathophysiology
Diagnosis and assessment
Definitions and criteria
Hypertension
Essential hypertension
Secondary hypertension
Pseudohypertension
Markedly elevated blood pressures
Assessment
Blood pressure measurement
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hypertension

