Epidemiology
Prolactinomas are the most common functioning pituitary tumour. Lactotroph adenomas (prolactinomas) account for approximately 30–40% of all clinically recognized pituitary adenomas. Microprolactinomas (<1 cm) are more common than macroprolactinomas (>1 cm). Women with microprolactinomas present earlier (with menstrual irregularities) than men.
Clinical presentations
The main action of prolactin is to stimulate lactation. Excess prolactin can result in an inhibition of gonadotrophin-releasing hormone (GnRH) and pituitary gonadotrophin release, and an impairment of gonadal steroidogenesis. Therefore patients with hyperprolactinaemia may present with galactorrhoea and symptoms of hypogonadism.
Women present with galactorrhoea (30–80%) and menstrual irregularities (oligomenorrhoea or amenorrhoea) or delayed menarche. Mild hyperprolactinaemia can cause infertility even when there is no abnormality of the menstrual cycle. These women account for about 20% of those evaluated for infertility. Galactorrhoea is less common in those with longstanding oestrogen deficiency.
Men present with reduced libido, impotence or infertility. They rarely present with galactorrhoea.
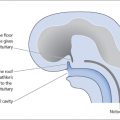
In addition to the symptoms of hyperprolactinaemia, patients with pituitary tumours may present with local mass affects, i.e. headache and visual field defects, and cranial nerve palsies (due to cavernous sinus invasion) or symptoms of hypopituitarism (e.g. adrenal insufficiency, hypothyroidism). Longstanding hyperprolactinaemia may result in low bone mineral density and osteoporosis. Most prolactinomas in females are small at the time of diagnosis.
Evaluation
It must be remembered that stress, sleep, exercise, intercourse and meals can cause a transient rise in serum prolactin levels. Thus borderline results should be repeated.
As mentioned above, prolactin levels can be elevated in patients with non-functioning adenomas due to pituitary stalk compression resulting in a reduction of the inhibitory effect of dopamine on prolactin secretion (‘disconnection’ hyperprolactinaemia). In non-functioning adenomas, elevated prolactin levels due to pituitary stalk compression rarely exceed 2000 mU/L and are almost never more than 4000 mU/L. Prolactin levels of more than 4000 mU/L are usually due to prolactin hypersecretion from a lactotroph adenoma (prolactinoma).
When measuring prolactin levels, it is important to be aware of the following two laboratory pitfalls (Fig. 14.1).
Macroprolactinaemia
Hyperprolactinaemia may be due to a decreased clearance of ‘macroprolactin’, which is a complex of the normal 22 kDa prolactin with immunoglobulin G (Fig. 14.1b
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree