Human Papillomavirus Infection and Anogenital Warts
Shelly T. Ben-Harush Negari
Jessica A. Kahn
KEY WORDS
Anogenital warts
External genital warts
Human papillomavirus
Human papillomavirus vaccines
Management
Oral human papillomavirus
Sexually transmitted infection
Treatment
Human papillomaviruses (HPVs) are small, nonenveloped, double-stranded DNA viruses of the Papillomaviridae family. More than 40 HPV types have been identified that infect the anogenital and oropharyngeal mucosa.1 Genital HPV types are classified as low risk and high risk.2 Low-risk types (e.g., HPV-6 and -11) may cause anogenital warts, mild vulvar intraepithelial neoplasia (VIN), vaginal intraepithelial neoplasia (VAIN), cervical intraepithelial neoplasia (CIN), penile intraepithelial neoplasia (PIN), and anal intraepithelial neoplasia (AIN). Vertical transmission of low-risk types from mother to child during delivery rarely may cause recurrent respiratory papillomatosis (RRP) in young children. High-risk types (e.g., HPV-16 and -18) may cause mild, moderate, or severe VIN, VAIN, CIN, PIN, and AIN; vulvar, vaginal, cervical, penile, and anal cancers; and oropharyngeal cancer.3
Epidemiology
Prevalence
At least 80% of sexually active adult men and women in the US have been exposed to genital HPV types at some point in their lives. The prevalence of HPV infection peaks during adolescence and young adulthood. In a nationally representative sample of US women, 20% of 14- to 17-year-olds, 38% of 18- to 21-year-olds, and 42% of 22- to 25-year-olds were positive for genital HPV.4 Prevalence rates in men are similar to those in women. Cross-sectional prevalence rates for oral HPV range widely, from approximately 2% to 20% in studies of adolescents and young adults (AYAs).5 The prevalence rate of symptomatic anogenital warts among US adults is estimated to be 1% to 5%, but rates up to 40% have been reported in patients presenting to sexually transmitted infection (STI) clinics. A population-based study in Sweden demonstrated that among 1,045,157 women, the crude incidence rate of condyloma was 528 per 100,000 person-years in unvaccinated individuals, and 138 per 100,000 person-years in fully vaccinated individuals.6 The prevalence of RRP is approximately four cases per 100,000 in children.7
Transmission
In AYAs, HPV transmission occurs primarily through sexual contact, including genital-genital, oral-genital, and digital-genital contact. AYAs acquire HPV infection rapidly after sexual initiation, often within a few months.8 Women who have sex only with women are also at risk for HPV infection and CIN.9
Risk Factors
Increased number of sexual partners, early age of sexual initiation, inconsistent condom use, cigarette smoking (also a cofactor in cervical carcinogenesis), immunosuppression, cervical ectopy, and history of genital warts and other STIs.
Pathophysiology and Natural History of HPV Infection
HPV initially infects the basal layer of epithelial cells through microabrasions in the skin or mucosa. Infected cells migrate to the suprabasal layers, where viral gene expression, viral replication, and particle formation occur. Although HPV infection is extremely common in AYAs, the vast majority of infections do not progress to anogenital warts, precancers, or cancer.10
Clinical Manifestations
Types of Anogenital Warts
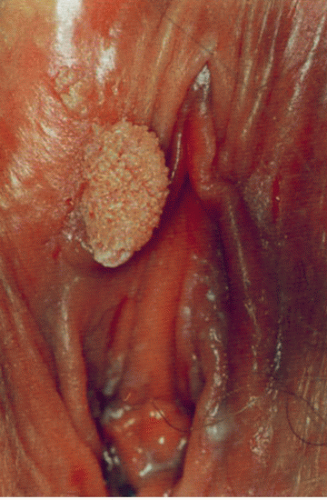
Condylomata acuminata: Exophytic growths with a granular, irregular surface and finger-like projections. They usually have highly vascular cores that produce punctuated or loop-like patterns unless obscured by overlying keratinized surfaces (Figs. 61.1 and 61.2).
Papular warts: Smooth, skin-colored, well-circumscribed papules that are usually 1 to 4 mm in diameter and have a round, slightly hyperkeratotic or smooth surface (Fig. 61.3).
Keratotic warts: These have a thick, horny (crust-like) layer; they resemble common warts or seborrheic keratoses (Fig. 61.4).
Flat-topped macules: These are subclinical lesions that are difficult to detect without techniques such as treatment with a weak acetic acid solution.
Location
Typical sites for anogenital warts in women include the cervix, vagina, vulva, urethra, and anus. Typical sites in men include the inner surface of the prepuce, frenulum, corona, penile shaft, glans, scrotum, and anus. Condylomata can be multifocal or multicentric. Condylomata acuminata tend to occur on partially keratinized, non-hair-bearing (“moist”) skin; keratotic and papular warts tend
to occur on fully keratinized (hair-bearing or non-hair-bearing) skin; and flat-topped warts may occur on either skin surface.
to occur on fully keratinized (hair-bearing or non-hair-bearing) skin; and flat-topped warts may occur on either skin surface.
Color
Pink, red, tan, brown, or gray.
Symptoms
Usually asymptomatic but may cause pruritus, burning, pain, urethral or vaginal discharge, urethral bleeding, or postcoital bleeding.
Exacerbating Factors
Pregnancy, skin moisture, and/or vaginal or urethral discharge.
Clinical Course
Lesions usually appear 2 to 3 months after infection, with a range of approximately 3 weeks to 8 months.11 Warts may regress spontaneously, persist, or increase in size or number. Over a period of months to years, most anogenital warts resolve.
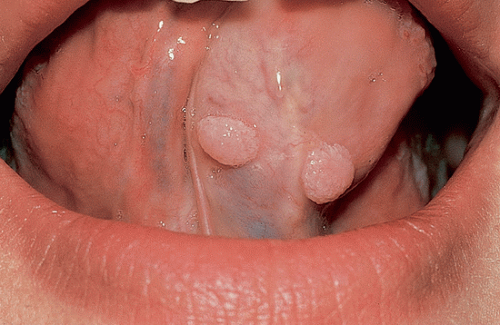 FIGURE 61.3 Papular warts (tongue). (From Lippincott Williams & Wilkins’ comprehensive dental assisting. Philadelphia, PA: Lippincott Williams & Wilkins, 2011.) |
Differential Diagnosis
The differential diagnosis for anogenital warts includes micropapillomatosis labialis of the labia minora, pearly penile papules, seborrheic keratosis, other benign genital lesions (skin tags, fibromas, lipomas, hidradenomas, and adenomas), condylomata lata (secondary syphilis) (see Fig. 61.5), molluscum contagiosum, granuloma inguinale, and high-grade intraepithelial lesions and cancer (Bowen disease, Bowenoid papulosis, dysplastic nevi, VIN, VAIN, PIN, AIN, and squamous cell carcinoma).
Diagnosis
Subclinical HPV Infection
HPV detection methods can be categorized generally as target amplification methods such as polymerase chain reaction, and signal amplification methods.12 In the US, HPV DNA testing is generally
recommended only in the context of cervical cancer screening for women ≥25 years of age to guide further management (i.e., reflex HPV testing for women with a cytologic test demonstrating atypical squamous cells of undetermined significance, and as a “cotesting” strategy with cytologic testing for women 30 to 65 years of age), as discussed in more detail in Chapter 50.13
recommended only in the context of cervical cancer screening for women ≥25 years of age to guide further management (i.e., reflex HPV testing for women with a cytologic test demonstrating atypical squamous cells of undetermined significance, and as a “cotesting” strategy with cytologic testing for women 30 to 65 years of age), as discussed in more detail in Chapter 50.13
 FIGURE 61.5 Condylomata lata (perineum). (From Edwards L, Lynch PJ. Genital dermatology atlas. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010.) |
TABLE 61.1 Recommended Treatment Options for External Genital Warts
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|