10 Communication is Essential in the Hospital Hospital Design and Systems Change to Benefit Older Adults The Admission Process: Opportunities for Health Status Updates Perioperative Care of the Elderly Patient in the Hospital Cardiac Risk Reduction through Medical Interventions Perioperative Pulmonary Complications Perioperative Pulmonary Evaluation Interventions to Reduce Pulmonary Complications Preventative Measures in the Hospital Venous Thromboembolism Prophylaxis Respiratory Illness Prevention Preventing Infections in the Hospital Selective Interventions to Improve Outcomes Care Transition Initiatives and Unplanned Hospital Readmissions Upon completion of this chapter, the reader will be able to: • Understand ways in which the admission process to the hospital can be an opportunity for a review of health status for older adults. • Describe ways that perioperative care of older adults in the hospital is different from the care of younger patients. • Know how to apply preventative measures in the hospital to reduce risks to hospitalized older patients. • Describe how to apply selective interventions to improve hospital outcomes and decrease unplanned readmissions and adverse patient outcomes. Nosocomial infections, loss of independence, functional status decline, medication interactions, polypharmacy, overtreatment, falls, cognitive loss, delirium, misinformed handoffs, and poor care transitions are just some of the complications that can occur during the hospitalization of an older adult. Although advances in medical and surgical care have decreased the morbidity and mortality of many diseases, the hospital has remained a dangerous place for older patients. Care provided to older adults in the hospital should strive to limit exposure to iatrogenic complications, maintain functional status, and provide patient- and family-centered care that is evidence based and disease focused. The risk of an older adult developing a new activity of daily living (ADL) disability during a hospitalization is estimated to be at least 30%, and about half of all older adults’ disabilities develop during a hospitalization.1 Frail elders with limited functional reserves fare even worse. Unfortunately, one year after hospital discharge, less than half of older adults have returned to their prehospitalization level of functioning.2 Certainly, hospitalization may be necessary to provide treatment to older adults. Knowledge of the many causes of functional decline in the hospital and actions aimed at functional status preservation are paramount for any practitioner caring for hospitalized older patients. It has been estimated that 7% to 15% of the 1 million older adults with Medicare who are hospitalized each year experience a preventable adverse event. Caring for older adults in the hospital should involve an interprofessional group of care providers. Optimal geriatric hospital care is provided by nursing case managers and geriatric social workers to assist in coordinating discharge needs, dieticians working to find food that is the correct caloric density and texture, nurses and nursing assistants providing direct patient care who are often the first to notice a patient change, consulting physicians, hospitalists, pharmacists, physical therapists, occupational therapists, and speech and language pathologists all working together to bring optimal care to older adults and their families. This large number of team members all must communicate with each other and with the patient and family during the hospitalization. This gathered information must additionally be communicated in an efficient and accurate way to the receiving facility that will take over care once the patient has left the hospital. This can include a rehabilitation facility, a skilled nursing facility, a long-term acute care hospital, a family member’s home, or the patient’s own residence (see Chapter 2. Since the term hospitalist was first used in 1996 to describe the growing number of physicians whose primary site of practice was within the hospital, the field has expanded rapidly.3 In urban areas today, hospitalists provide the majority of nonsurgical care to hospitalized adults in the United States.3 The hospitalist often is the primary care coordinator and communicator among the many team members involved in the care of an older adult in the hospital. In 1992, with funds from the John A. Hartford Foundation, New York University began broadly field-testing nursing care models including the geriatric resource nurse (GRN) program. This project became known as Nurses Improving Care for Health System Elders (NICHE) and aimed to create a better care environment for the hospitalized elderly patient by improving nursing practice.4 Nursing leadership is integral to good care of older adults, and the NICHE program provides resources, project management support/mentoring for NICHE-based hospital initiatives, evidence-based clinical protocols that address “never events,” and shared information, knowledge, and expertise to more than 300 participating hospitals.5 Acute care for the elderly (ACE) units have demonstrated improved functional outcomes without increased costs or length of stay.6 This model of comprehensive inpatient geriatric care incorporates (1) hospital environment modifications, (2) minimization of adverse effects of hospitalization, (3) early discharge planning, and (4) patient-centered care protocols.7 The benefit of ACE units is also being expanded hospitalwide. The concept of a mobile acute care for the elderly (MACE) unit has also been described. The main goals of the MACE unit are to bring the interdisciplinary, patient-centered team approach to hospitalized older adult patients throughout a hospital, rather than having the team located solely on one geographically based unit. A 2010 study found that among more than 8000 older adults, those being treated via MACE service (compared to those admitted to an ACE or a traditional unit) had lower length of stay and lower costs with no change in in-hospital mortality or 7- or 30-day readmission rates.6 In addition to a redesign of care processes and procedures for caring for older hospitalized adults, the physical environments of hospitals are additionally being designed to allow for improved care.8 Hospital design that focuses on the needs of older adults and their families has improved the hospital campus, the unit, the room, and the amenities available. Design features can include reserved or valet parking and benches along long walkways; handrails; matte floor finishing or low-pile carpeting; low-color-contrast floors with clear contrast with walls; sound-absorbing materials in rooms with available assistive listening devices; choice of chairs with armrests; automatic faucets and doors; and easy-to-see and easy-to-activate call systems.8 Because many older adults rely on additional support for successful aging, geriatric hospital care must embrace the principles of patient- and family-centered care. As defined by the Institute for Patient- and Family-Centered Care, the core principles include respect and dignity, collaboration, participation, and meaningful information sharing.9 Family is defined as broadly as possible to include any person that an older adult may rely on for support, whether emotional, physical, or financial.9 Partnership with family during the hospitalization of older adults is paramount to a successful admission, and every attempt to involve family at the highest level desired by the patient should be sought. Minimizing barriers to family participation in health care should always be a paramount goal of excellent care. Screening for elder mistreatment among asymptomatic populations has not been evaluated, but the presence of elder abuse has been estimated to be between 2% and 10%.10 Elder abuse can broadly be defined as physical, psychological, or sexual abuse, material exploitation of money or property, or neglect and failure to meet a dependent older person’s needs. The possibility of nonaccidental trauma or neglect of an older adult admitted to the hospital should be entertained by the clinician based on a high index of suspicion.10 Identification of social support and appropriate referral to area Adult Protective Services agencies should be made whenever elder abuse is suspected (see Chapter 33). During the admission to the hospital, a discussion on alcohol use should be completed. The prevalence of older adults with alcohol-related problems has been reported to be between 2% and 22%, depending on the definition used.11 With the aging population, even with a constant prevalence, the number of older adults with alcohol use problems will increase dramatically. Screening tools for younger adults usually focus on work or legal difficulties that arise from drinking, and these consequences are rarer in older adults with harmful drinking patterns.11 Unfortunately there are currently no appropriate screening questionnaires validated for older adults to detect harmful or hazardous drinking patterns (see Chapter 34). Frailty is a geriatric syndrome defined as a state of increased vulnerability to both acute and chronic stressors as a consequence of reduced physiologic reserve.12 Frailty is associated with functional decline, loss of independence, and mortality. The identification of this syndrome should be readily considered for any older adult being admitted to the hospital (see Chapter 29). The concept of frailty is relevant for providers of geriatric hospital care, because it provides a ready explanation for the different stress tolerances of older adults. Stressors in the hospital are summative and can include not only the inciting medical or surgical event, but also sleep deprivation, medication side effects, sensory deprivation, and caloric deficiencies resulting from restrictive diets, nothing-by-mouth status, or general illness.12–14 For men and women older than age 60, ten days of bed rest results in a similar loss of muscle mass as a decade of normal aging.13 To help lessen the impact of hospitalization on older adults, physical activity (especially resistance training), nutritional consultations and supplementation, and vitamin D supplementation when appropriate should be strongly considered.13 Nearly half of all patients undergoing a surgical procedure are now older than age 65, with the percentage expected to increase further over the next 15 years as the population continues to age.15 Studies have shown 21% of elderly patients will suffer from at least one perioperative complication following a nonthoracic surgery, potentially leading to prolonged hospitalization, increased mortality, and long-term morbidity.16,17 Because of the heterogeneity of elderly patients, a patient-centered approach in close conjunction with the surgical team is required to reduce the risk of complications and adverse outcomes. The preoperative evaluation of elderly patients begins with a frank discussion on goals of care (Figure 10-1). Survival and longevity may be the most important outcomes for a younger population but it may not be the primary goals for every elderly patient. A more important outcome may be related to the patient’s functional status following the surgery. A full discussion of all the potential outcomes is necessary, with an honest discussion of prognosis of recovery related to functional status and the potential loss of independence. Elderly patients may elect to forgo emergent interventions if the outcome would likely lead to loss of independence and functional status, and instead may elect for only comfort care measures. The role of the medical clinician in the preoperative evaluation is to help review all of the options for the patient including the option for palliative care. The preoperative evaluation provides an excellent opportunity to better define end-of-life decision making for the patient, especially for those surgical interventions that carry significant risks for the elderly patient. Patients should be encouraged to discuss their decisions with family members and their health care power of attorney to prevent undesired interventions in the future. Figure 10-1 Preoperative evaluation. (Adapted from Fleisher LA, Beckman JA, Brown KA, et al. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2009;120(21):e169-e276.) For nonemergent surgeries, the clinician must inquire about any active cardiac conditions. Active cardiac conditions include all of those conditions that would warrant urgent treatment whether the patient was planning a surgical intervention or not: acute coronary syndrome, myocardial infarction within 30 days, significant arrhythmias, and severe valvular disease.24 The time frame for delaying the surgical intervention depends on the cardiac event and the intervention. There is a paucity of evidence for the correct timing of surgery following medical intervention. Decisions are based on best available evidence and consensus statements (Figure 10-2). Figure 10-2 Preoperative cardiac evaluation. EKG, Electrocardiogram; METs, metabolic equivalents of a task. (Adapted from Fleisher LA, Beckman JA, Brown KA, et al. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2009;120(21):e169-e276.) A vital component of the perioperative care of patients with a history of a recent cardiac event is the management of antiplatelet therapy. Dual therapy with aspirin and clopidogrel is required for 3 to 6 months following acute myocardial infarction, 2 weeks following angioplasty, 6 weeks following a bare metal stent, and 1 year following a drug-eluting stent.18 All nonemergent surgeries that require discontinuing clopidogrel must be delayed until these time frames are met. Then the surgery can be performed with the patient taking aspirin alone. Primary care doctors must work closely with their surgical colleagues to weigh the risk of bleeding against the risk of coronary artery disease, with strong consideration to continue aspirin for secondary prevention of coronary heart disease in the perioperative period. The procoagulant, proinflammatory state following surgery places patients at a significantly higher risk for cardiac in-stent stenosis with potential catastrophic results, with an odds ratio of 3.1 peaking 10 days after surgery.19 Restenosis has been reported with withdrawal of aspirin even after 2 years from stent placement, which emphasizes the absolute importance of continuation of aspirin.20,21 Evidence on the risk of continuation of aspirin in the perioperative period has not been well studied, but a meta-analysis did not demonstrate increased mortality or postoperative complications when aspirin was continued.22 In addition, outside of neurosurgical interventions, there is no evidence to demonstrate that the increased risk of bleeding with continuation of aspirin therapy translates to an increase in mortality.23 Patients undergoing low-risk ambulatory surgical procedures (e.g., endoscopic procedures or cataract, simple breast, or ambulatory surgeries) do not have a higher 30-day risk of cardiac events compared to peers.24 With the lack of apparent increased cardiac risk, patients may proceed to the operating room (OR) without any additional evaluation for low-risk surgeries. Functional assessment is of vital importance, especially in the elderly population who can have a broad range of activity and functional levels. Functional capacity can be estimated by history using published charts or having the patient perform a treadmill test using standard protocol. Patients who are able to perform physical activities at or higher than 4 METS (metabolic equivalents of a task) may proceed to the planned procedure without additional evaluation.25 For patients who are unable to achieve 4 METs or if functional capacity is unknown, an evaluation of risk factors for perioperative events (e.g., ischemic heart disease, renal insufficiency, cerebrovascular disease, diabetes, or history of congestive heart failure) should be pursued.24 Patients who have no risk factors may proceed to the OR without any further cardiac evaluation. Patients with one to two risk factors may proceed to OR with beta-blockade, or noninvasive coronary evaluation can be considered. Patients with three or more risk factors undergoing an intermediate-risk surgery may also proceed to OR with beta-blockade or may undergo noninvasive coronary evaluation. Those patients with three or more risk factors undergoing high-risk surgery may proceed to the OR with beta-blockade and a statin, or noninvasive coronary evaluation should be considered if those results have the potential to alter decision making and change management. There have been multiple studies looking at beta-blockade in the perioperative period, with conflicting results.25–28 Early studies showed significant promise for the prevention of acute myocardial infarction; unfortunately, follow-up studies have not consistently demonstrated this benefit. Two studies in 2007 and 2009 led to an update of the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Perioperative Guidelines in 2009, and provide guidance for applying the conflicting data in practice.25 More recent studies confirmed the cardioprotective benefit of perioperative beta-blockade but demonstrated the increased risk of stroke and death. The differences between the studies provide insight into the mechanism of risk for perioperative beta-blockade and provide guidance for initiating beta-blockade. The avoidance of hypotension and bradycardia appears vital to reduce the risk of ischemic stroke. Beta-blockade should be initiated at a low dose and titrated slowly up to goal prior to surgery. The exact timing for initiating beta-blockade has not been established, but based on the results of available data, same-day initiation with rapid titration should be avoided.27 The only prospective randomized trial on perioperative statin use was a small study of 100 patients investigating the perioperative use of atorvastatin for vascular surgery.29 Patients were placed on 20 mg atorvastatin for a total of 45 days and a minimum of 2 weeks prior to the surgery with a composite outcome of death from stroke and acute coronary syndrome. A statistically significant difference in composite outcome was reached in the atorvastatin arm versus placebo at 6 months (8% vs. 26%). Multiple retrospective studies have also shown reduced perioperative cardiac events with the use of statins in both vascular and nonvascular studies. Based on the limited evidence available, the 2009 ACCF/AHA Guidelines find the use of statins “reasonable” for patients undergoing vascular surgery and “may be considered” for patients with one or more risk factors undergoing intermediate-risk surgery.25 Perioperative pulmonary complications (PPCs) are encountered frequently following noncardiothoracic surgeries and contribute significantly to perioperative and long-term morbidity and mortality. The American College of Chest Physicians includes atelectasis, pneumonia, respiratory failure, and exacerbation of underlying chronic lung disease as PPCs. An incidence of 5.5% to 6.8% is found when using rigorous methods to define PPC.17,31 PPCs are an even stronger predictor than perioperative cardiac complications for longer term perioperative mortality in the elderly, with a hazard ratio of 2.41.30 Despite being a stronger predictor for adverse outcomes and having a similar frequency as perioperative cardiac events, perioperative pulmonary evaluation and PPCs prevention are often placed at a lower priority by clinicians and patients. Because advanced age is a risk factor for PPCs, clinicians who care for the elderly need to have increased awareness and diligence in evaluating and preventing PPCs. The preoperative pulmonary evaluation starts with identification of risk factors for developing PPCs (Box 10-1). Of the risk factors listed, a history of chronic obstructive pulmonary disease (COPD) and age older than 60 are the two highest predictors of the development of PPCs. The risk for PPCs increases with each decade, with odds ratios of 2.09 for patients 60 to 69 and 3.04 for patients 70 to 79.32 Another important risk factor is functional status, which predicts both overall mortality and risk for PPCs with an odds ratio of 2.51 for developing PPCs if patients are unable to perform any ADLs and 1.65 if they require assistance for some of their ADLs. Those patients who are identified as having any risk factors for PPCs should proceed to additional evaluation and undergo preoperative and postoperative interventions to reduce risk. Pulmonary function tests (PFTs) have an important role in the evaluation and risk analysis for patients undergoing cardiothoracic surgery, but evidence has not demonstrated benefit for non-cardiothoracic surgeries. A PFT threshold level used to decide when to withhold surgery has not been demonstrated in non-cardiothoracic surgeries. Patients who meet criteria for PFTs for alternative reasons, such as initial evaluation of COPD, should have PFTs ordered. There is not a separate indication for non-cardiothoracic perioperative PFT evaluation, even in the setting of stable COPD, because the test results do not add any additional value past what is obtained in the history and examination.32 The routine use of chest x-ray examinations also does not provide additional data past what can be identified with a history and physical. Although abnormalities may be identified, rarely do they lead to a change in management for the patient. Based on the available evidence, the American College of Physicians does not recommend the routine use of chest x-ray studies for a preoperative pulmonary evaluation.32 Low albumin is a very powerful predictor of perioperative mortality and long-term morbidity in addition to a predictor of PPCs. Patients with an albumin lower than 3.5 g/dL had an incidence of 27.6% of PPCs compared to an incidence of 7.0% in patients with normal albumin.32 Unfortunately, nutritional support strategies such as total parenteral nutrition (TPN) in the perioperative period have not demonstrated any benefit over regular diet.33 Patients who have one or more risk factor for PPCs or are undergoing a high-risk surgery should have a preoperative albumin level test so they can be better counseled about the potential risk of the surgery. Evidence-based interventions to reduce PPCs are limited, with studies either not rigorously designed or not demonstrating any significant benefit. The best evidence for the prevention of PPCs has been seen with deep breathing exercises or incentive spirometry (IS) in the perioperative period. IS has been compared to deep breathing exercises, with both modalities appearing to have similar results. PPCs are cut in half with either of these techniques.34 The results seem to be superior if the patient receives education prior to the surgery and even greater if the patient begins inspiratory training exercises several weeks prior to surgery.35
Hospital care
Communication is essential in the hospital
Hospital design and systems change to benefit older adults
Hospital physical design
Patient- and family-centered geriatric hospital care
The admission process: Opportunities for health status updates
Elder abuse
Alcohol abuse
Frailty as a risk for poor hospital outcomes
Perioperative care of the elderly patient in the hospital
Establishing goals of care

Cardiac evaluation
Active cardiac conditions

Low-risk surgery
Functional assessment
Cardiac risk factors
Cardiac risk reduction through medical interventions
Beta-blockade
HMG-COA reductase inhibitors (statin therapy)
Perioperative pulmonary complications
Preoperative pulmonary evaluation
Interventions to reduce pulmonary complications
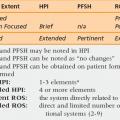
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hospital care